Last Updated on December 2, 2025 by Bilal Hasdemir

Did you know many young girls have medical exams every year? A big part of these exams check the groin area. An inguinal examination is a key medical step to find health issues and oddities in the groin.Our amazing guide to the female inguinal examination. We explain the simple, critical process and what your doctor is looking for.
Many young girls may find the prospect of a medical check-up intimidating. We aim to give you all the info you need. We’ll help you understand the pediatric inguinal exam and its benefits.
Key Takeaways
- Understanding the importance of inguinal examination for girls
- What to expect during a pediatric inguinal exam
- Benefits of early detection and diagnosis
- Preparing your child for a physical examination
- Inguinal palpation technique used during the examination
Understanding the Inguinal Region in Females

It’s key for doctors to know about the female inguinal anatomy. This area, also called the groin, is complex and important for women’s health.
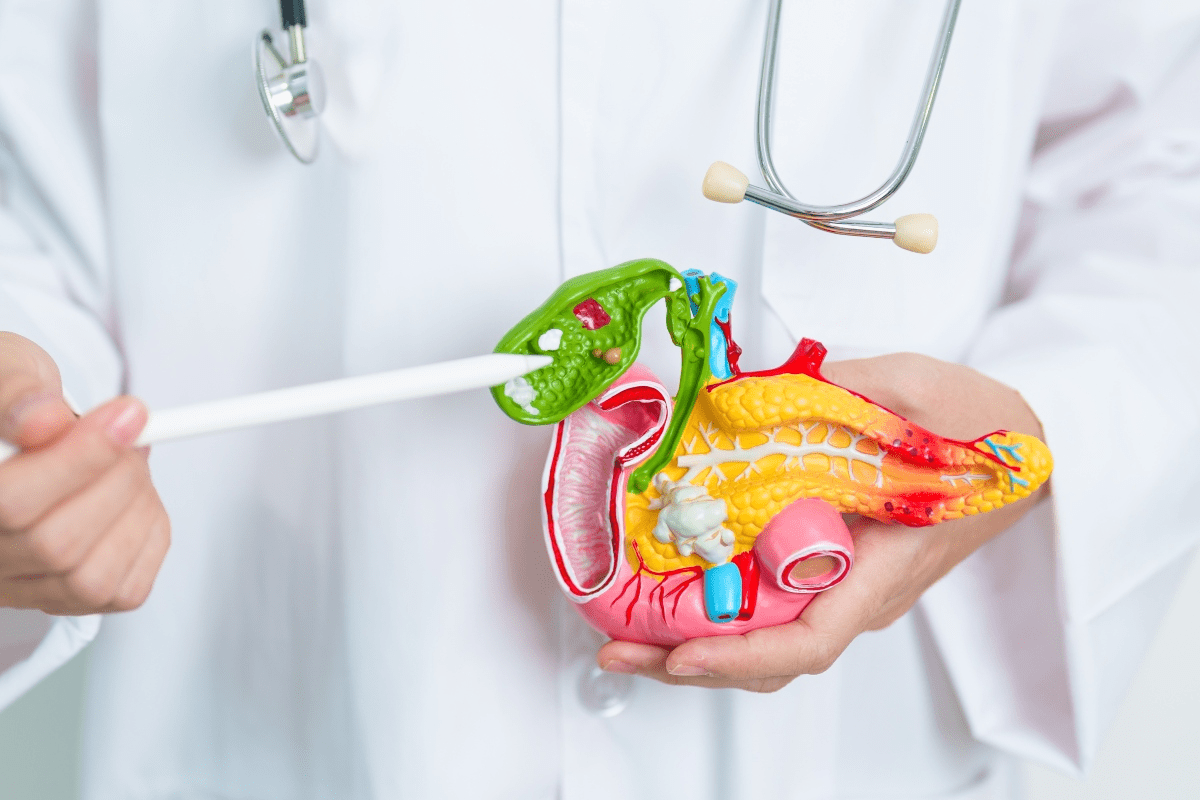
Anatomy of the Female Inguinal Area
The female groin has an inguinal canal, a path through the belly. Inside this canal is the round ligament of the uterus. The area’s anatomy is detailed, with layers of fascia and muscles.
Key components of the female inguinal anatomy include:
- The inguinal ligament, which forms the floor of the inguinal canal
- The transversalis fascia, a layer that lies beneath the muscular layer
- The ilioinguinal nerve, which provides sensory innervation to the region
Differences Between Male and Female Inguinal Anatomy
While the inguinal region’s basic structure is similar, there are big differences. In males, the canal has the spermatic cord. In females, it has the round ligament of the uterus. This is important for understanding female anatomy.
Anatomical Feature | Male | Female |
Contents of Inguinal Canal | Spermatic Cord | Round Ligament of Uterus |
Purpose of Contents | Supports testicular structures | Supports uterine structures |
A leading medical expert says, “Knowing these differences is key for diagnosing and treating inguinal issues in women.”
“The female inguinal region’s unique anatomy demands a tailored approach to examination and diagnosis.”
Understanding the female inguinal region helps doctors better manage conditions. This leads to better care for patients.
Purpose and Importance of Inguinal Examinations

Inguinal examinations are key in preventive healthcare for girls and women. They help find health problems early. This is important for keeping everyone healthy and catching serious issues before they get worse.
Medical Conditions Detected Through Inguinal Examination
Healthcare providers use inguinal exams to find many medical issues. This includes inguinal hernias, problems with lymph nodes, and other health concerns. Finding these problems early is key to treating them well and avoiding bigger issues.
Inguinal hernias are a big concern. They happen when part of the intestine bulges through a weak spot in the muscles. If not treated, they can cause a lot of pain and even be life-threatening.
Preventive Health Benefits
Regular inguinal exams have many benefits for health. They help find problems early, so they can be treated quickly. This lowers the chance of serious problems and improves health outcomes. These exams also let doctors teach patients how to stay healthy.
Preventive care, like inguinal exams, is vital for girls and women’s health. Prioritizing these exams allows individuals to safeguard their health and prevent significant medical concerns.
When Is a Female Inguinal Examination Necessary?
Whether a female inguinal examination is needed depends on several factors. These include routine check-ups and specific symptoms. We will look into these factors to understand when such an examination is advised.
Routine Physical Examinations
Routine physical exams are key to preventive healthcare. During these, a healthcare provider might do an inguinal exam. This is to check for any issues or abnormalities. For girls, these exams are very important as they grow and develop.
Key aspects of routine inguinal examinations include:
- Checking for inguinal hernias
- Examining lymph nodes for any abnormalities
- Assessing overall health and development
Symptom-Based Indications
Certain symptoms may mean a girl needs an inguinal exam. These symptoms include pain or discomfort in the groin, swelling, or other unusual signs. If a girl has any of these symptoms, she should see a healthcare provider.
Common symptoms that may require an inguinal examination are:
- Pain or discomfort in the groin
- Swelling or lumps in the inguinal area
- Redness or inflammation
Age-Specific Considerations
The need for an inguinal exam can change with age. For infants and toddlers, these exams are part of developmental checks. For older girls and teens, the exam might focus on specific symptoms or concerns.
Age-specific considerations include:
Age Group | Considerations |
Infants and Toddlers | Developmental assessments, checking for congenital issues |
School-Age Children | Monitoring for hernias, assessing for injury or trauma |
Adolescents | Evaluating symptoms, reproductive health considerations |
Preparing for the Examination
Getting ready for an inguinal examination is key. It involves educating the patient, making the environment comfortable, and having the right equipment.
Patient Education and Consent
Teaching the patient about the examination is vital. We need to make sure they know why and how it’s done. This means explaining it clearly and answering their questions. We also need to get their consent.
- Explain the examination process and its importance.
- Discuss what the patient can expect during the examination.
- Address any patient concerns or questions.
- Obtain informed consent before proceeding.
Creating a Comfortable Environment
Making the environment comfortable is key to a smooth exam. This means keeping the room at a good temperature and ensuring privacy. Sometimes, having a chaperone is also necessary.
- Adjust the examination room temperature to a comfortable level.
- Ensure the patient has adequate privacy during the examination.
- Offer the presence of a chaperone if required.
Necessary Equipment and Setup
Having the right equipment is essential for a good examination. This includes a well-lit area, the right table, and any special tools needed.
- A well-lit examination area.
- An appropriate examination table.
- Specific medical instruments for the examination.
By focusing on these areas, we can make sure the examination is done well. This means getting the right diagnosis and keeping the patient comfortable.
The Female Inguinal Examination Procedure: Step-by-Step
A thorough inguinal examination in females involves a systematic approach. This includes patient positioning, visual inspection, and palpation. We will guide you through the step-by-step process that healthcare professionals follow to assess the inguinal region.
Patient Positioning
Proper patient positioning is key for a successful inguinal examination. The patient should lie on their back with their legs slightly apart. This makes it easier to access the inguinal area and reduces discomfort.
Visual Inspection Techniques
Visual inspection is the first step in assessing the inguinal region. We look for any visible signs of abnormalities such as swelling, redness, or bulges. The patient is asked to cough or strain to help identify any possible hernias.
Palpation Methods
Palpation involves gently feeling the inguinal area with the fingers to detect any abnormalities. We use a systematic approach, starting with the superficial inguinal ring and then moving to the inguinal canal. The patient is asked to cough during palpation to aid in the detection of hernias.
Examination Technique | Purpose | Key Findings |
Visual Inspection | Identify visible abnormalities | Swelling, redness, bulges |
Palpation | Detect abnormalities through touch | Hernias, lymphadenopathy |
Patient Positioning | Facilitate examination | Optimal access to inguinal area |
By following this step-by-step guide, healthcare professionals can conduct a thorough inguinal examination in female patients. This ensures accurate diagnoses and appropriate treatment plans.
Assessing for Inguinal Hernias in Girls
Checking for inguinal hernias in girls is very important in pediatric care. It needs a careful approach. An inguinal hernia happens when part of the intestine bulges through a weak spot in the abdominal muscles. Girls face special challenges when it comes to diagnosing these hernias.
Types of Hernias Common in Females
Inguinal hernias are less common in girls than in boys but are a big health issue. The most common type in girls is the indirect inguinal hernia. This happens when tissue pushes through the internal inguinal ring.
Key characteristics of inguinal hernias in females:
- Often smaller and less likely to incarcerate or strangulate
- May be more challenging to diagnose due to their smaller size
- Can be associated with increased risk of complications if not promptly treated
“Early diagnosis and treatment of inguinal hernias in children are critical to avoid complications.”
Diagnostic Techniques
Diagnosing inguinal hernias in girls needs a mix of clinical checks and diagnostic methods. A detailed physical exam is key.
Diagnostic Method | Description | Advantages |
Physical Examination | Visual inspection and palpation of the inguinal region | Non-invasive, cost-effective |
Ultrasound | Imaging technique using high-frequency sound waves | High sensitivity, non-ionizing |
Differentiating Hernias from Other Conditions
It’s important to tell inguinal hernias apart from other conditions that might look similar. These include lymphadenopathy or hydroceles. Getting the right diagnosis is key for the right treatment.
Differential diagnoses to consider:
- Enlarged lymph nodes
- Cysts or tumors
- Hydroceles or other fluid collections
Healthcare providers use a mix of clinical skills and diagnostic tools to accurately diagnose and treat inguinal hernias in girls. This ensures the best results.
Lymph Node Examination in the Inguinal Region
Lymph nodes in the inguinal region are key to our immune system. They help check the health of our lower legs and genital area. These nodes drain lymph from our lower limbs, external genitalia, and lower abdominal wall. So, checking them can tell us a lot about health issues.
Normal vs. Abnormal Findings
It’s important to know the difference between normal and abnormal lymph nodes. Normally, these nodes are small, soft, and move easily. But, if they’re enlarged, tender, firm, or stuck in place, it could mean trouble.
Abnormal findings include nodes that are over 1 cm, hurt when touched, or look irregular. These signs need more investigation to find out why.
Clinical Significance of Enlarged Lymph Nodes
Big lymph nodes in the inguinal area can mean serious things. They might show infections like STIs, urinary tract infections, or skin infections. They could also point to cancer, like lymphoma or cancer spreading from the genital or lower limb areas.
Big lymph nodes are a big deal. They need a careful look at the patient’s history and a physical check-up. Finding out why they’re big helps decide what tests and treatments are needed.
Palpation Techniques for Lymph Nodes
Checking lymph nodes needs a soft but firm touch. The patient should lie on their back with their legs bent and turned out. The examiner uses their finger pads to feel the inguinal area, looking for nodes along the inguinal ligament and nearby.
Good palpation techniques compare both sides for evenness. They check the size, tenderness, feel, and how easy it is to move any found nodes. This skill is vital for doctors to spot important signs.
Age-Appropriate Approaches to Examinations
When we do inguinal exams on girls, we need to think about their age. Each age has its own needs, both physical and emotional. We aim to care for them in a way that’s right for their stage of growth.
Infants and Toddlers
Infants and toddlers need a soft touch during exams. We do these exams with them lying on their back. Sometimes, we use toys or distractions to help them relax.
The exam should be quick and simple. We look for things like hernias or swollen lymph nodes.
Key considerations for this age group include:
- Maintaining a calm environment to reduce stress
- Using appropriate-sized equipment for the examination
- Involving parents or caregivers in the process to provide reassurance
School-Age Children
School-age kids need a different way of being approached. They know more about what’s going on and might feel nervous. We tell them what will happen in a way they can understand.
The exam is gentle but more detailed. These kids can usually tell us more about how they feel.
Effective communication is key in making the child feel comfortable and cooperative during the examination.
Age Group | Examination Approach | Key Considerations |
Infants/Toddlers | Gentle, non-invasive, distraction techniques | Calm environment, appropriate equipment, parental involvement |
School-Age | Explanatory, gentle, thorough | Clear communication, child cooperation, symptom feedback |
Adolescents
Adolescents get their exams with privacy and respect in mind. We explain everything in detail and make sure they agree to the exam. The method is similar to adults, but we talk about what we find and its health implications.
“Adolescents benefit from a respectful and professional approach to their care, which includes thorough explanations and consideration of their privacy.”
Cultural Sensitivity and Psychological Considerations
Doing inguinal exams on girls needs more than just medical skills. It also needs understanding of cultural sensitivity and psychology. Healthcare workers must know about their patients’ backgrounds and values. This way, they can give care that is both kind and respectful.
Addressing Patient Anxiety
Patient anxiety is a big issue during inguinal exams, more so in kids and teens. Creating a calm and comfortable space is key. This means explaining things clearly and gently, keeping things private, and involving parents when needed.
To lower anxiety, healthcare providers can use simple language, let patients ask questions, and be gentle and respectful. This makes the exam less scary.
Cultural Competence in Physical Examinations
Being culturally competent is vital for care that respects patients’ cultural and personal values. It means knowing how culture might affect a patient’s comfort during an exam. Providers should be sensitive to modesty concerns and adjust their approach.
For example, having a female chaperone can make patients from modest cultures feel more at ease. Also, paying attention to non-verbal cues and cultural norms helps providers handle sensitive situations with empathy.
Trauma-Informed Approaches
Using trauma-informed approaches in inguinal exams is critical, mainly for those who’ve been through trauma. It’s about making a safe space, being aware of triggers, and letting the patient feel in charge.
Healthcare providers need training to spot trauma signs and act right. This might mean going at the patient’s pace, avoiding sudden actions, and explaining each step clearly.
Key Considerations | Description | Benefits |
Patient Education | Explaining the examination process clearly | Reduces anxiety, increases trust |
Cultural Sensitivity | Understanding and respecting cultural norms | Enhances patient comfort, improves care delivery |
Trauma-Informed Care | Recognizing and responding to trauma signs | Creates a safe environment, supports healing |
Pathological Findings and Differential Diagnoses
During an inguinal examination, many different findings can show up. It’s important for healthcare providers to know about these. They need to watch for various conditions in the inguinal area.
Common Abnormalities
Several common issues can be found during an inguinal exam. Inguinal hernias are more common in men but can happen in women too. This is often due to certain health conditions or body shapes.
Lymphadenopathy, or swollen lymph nodes, can also be seen. It might mean an infection, inflammation, or another health issue. It’s key to figure out what it is through a detailed check-up.
Differential Diagnostic Considerations
When finding something unusual during an inguinal exam, doctors have to think about many possible causes. They look at the symptoms, medical history, and might do more tests. This helps find out what’s really going on.
Some possible causes include hydroceles, cysts, or other lumps in the inguinal area. Knowing about these and how they usually show up is vital for making the right diagnosis and treatment.
By looking at all the possible findings and possible causes, doctors can give patients the best care possible.
Documentation and Follow-Up Protocols
Keeping detailed records and following up properly is key in inguinal exams. Accurate notes and clear talks help girls get the care they need.
Proper Medical Documentation
Good medical records are vital for ongoing care. We must write down all findings, whether they’re normal or not. This includes the exam details, any observations, and the inguinal area’s condition.
Key elements of proper documentation include:
- Patient history and relevant clinical information
- Description of the examination technique used
- Findings, including any abnormalities detected
- Recommendations for follow-up care or further investigation
Documentation Element | Description | Importance |
Patient History | Relevant medical and surgical history | Provides context for examination findings |
Examination Technique | Description of methods used during examination | Ensures reproducibility and clarity |
Findings | Results of the inguinal examination | Critical for diagnosis and treatment planning |
Communication with Patients and Families
Talking clearly and kindly with patients and families is vital. We need to explain the exam’s results in simple terms. This helps address any worries or questions they might have.
Effective communication strategies include:
- Using plain language to explain medical terms
- Providing written information to supplement verbal explanations
- Encouraging questions and addressing concerns sensitively
Referral Guidelines
Deciding when to send a patient to a specialist is important. We have rules to help figure this out. This ensures patients get the right care.
Referral criteria may include:
- Suspected inguinal hernias or other abnormalities requiring surgical evaluation
- Unclear or complex diagnoses needing further investigation
- Conditions that are beyond our scope of practice
By sticking to these guidelines and focusing on the patient, we make sure girls get top-notch care during inguinal exams.
Special Considerations in Pediatric Gynecology
In pediatric gynecology, we take a detailed approach to meet the unique needs of young patients. When doing inguinal exams, we look at the bigger picture of gynecological health.
Integrating Inguinal Examination with Gynecological Assessment
In pediatric gynecology, inguinal exams are part of a full gynecological check-up. This helps us understand a patient’s health fully. It lets us spot any problems early.
Young girls’ bodies are different from adults’, and their inguinal areas are developing. Any unusual findings can signal serious issues that need quick action.
Reproductive Development Concerns
Watching how a child’s reproductive system grows is key in pediatric gynecology. We look for signs of early or late puberty. These signs can affect a child’s health and future well-being.
- Monitoring for signs of early or delayed puberty
- Assessing for any anatomical abnormalities
- Addressing concerns related to menstrual health in adolescents
When to Refer to a Specialist
Deciding when to send a patient to a specialist is important in pediatric gynecology. We consider how complex the case is and if it needs special care.
Referring to a specialist might be needed for complex genital issues, suspected cancers, or when advanced tests like laparoscopy are required.
Conclusion
A female inguinal examination is key for preventive care and health screenings for girls and women. It helps find and treat health problems early. This improves overall health and well-being.
Doing these exams well means educating patients, being sensitive to their culture, and knowing female anatomy well. We must keep stressing the importance of preventive care for our patients’ health.
Adding female inguinal exams to regular healthcare can lead to better health outcomes. It shows our commitment to top-notch healthcare and support for international patients. We focus on preventive care with great attention to detail.
FAQ
What is an inguinal examination, and why is it necessary for girls?
An inguinal examination checks the inguinal area for health issues. It’s important for girls to find problems like hernias early. This way, they can get the right treatment quickly.
How is the inguinal examination performed?
The exam starts with the patient in a certain position. Then, doctors look and feel the area. They use special methods to check for any problems.
What are the benefits of regular inguinal examinations for girls?
Regular exams help prevent health problems. They catch issues early and allow for quick treatment. This keeps girls and women healthy.
At what age should girls undergo their first inguinal examination?
The first exam depends on the girl’s health and risk factors. It usually happens during routine check-ups. The frequency might change based on age or symptoms.
How can healthcare providers make girls feel more comfortable during an inguinal examination?
Doctors can make the exam comfortable by explaining things and getting consent. They use gentle methods and try to reduce anxiety. They also respect the patient’s culture.
What are the common abnormalities detected during an inguinal examination?
Doctors often find hernias, big lymph nodes, and other problems in the inguinal area. They use different methods to figure out what’s wrong.
How are inguinal hernias diagnosed in girls?
Doctors use physical checks and sometimes tests to find hernias. Knowing the different types helps them make the right diagnosis.
What is the role of lymph node examination during an inguinal assessment?
Checking lymph nodes helps doctors see if the immune system is working right. They feel the nodes to see if they’re normal or not.
How do healthcare providers document findings from an inguinal examination?
Doctors write down all the findings from the exam. They talk to patients and families about what they found. They also give guidelines for further care.
When should a girl be referred to a specialist following an inguinal examination?
If the exam finds a serious problem, like a hernia, a specialist might be needed. The decision to refer depends on the complexity of the issue.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK423/