Last Updated on November 26, 2025 by Bilal Hasdemir

Getting a correct diagnosis is key for treating groin hernias well. Liv Hospital’s commitment to leading-edge care shows how important it is to tell femoral and inguinal hernias apart.
Femoral and inguinal hernias are two main types of groin hernias. They have different spots and features. On a CT scan, femoral hernias are found lateral to the pubic tubercle and can press on the femoral vein.
It’s vital to know the differences between these hernias for accurate diagnosis and better care. CT scans and radiology are key in spotting the unique traits of each hernia type.
Key Takeaways
- Accurate diagnosis is critical for effective treatment of groin hernias.
- Femoral and inguinal hernias have distinct anatomical locations.
- CT scans help identify the characteristics of each type of hernia.
- Radiological differences are key for precise diagnosis.
- Understanding these differences leads to better patient outcomes.
Understanding Groin Hernias: Anatomical and Clinical Context

Groin hernias, like femoral and inguinal types, need clear radiological differentiation for good management. These hernias happen in the inguinal area, which is both complex and hard to handle clinically.
Definition and Classification of Groin Hernias
A hernia is when an organ or tissue bulges through a hole in its wall. Groin hernias are split into two main types based on where they are and what they contain.
- Inguinal hernias: These happen when tissue, like part of the intestine, pushes through a weak spot in the abdominal muscles in the inguinal canal.
- Femoral hernias: These occur just below the inguinal ligament, where the femoral artery and vein pass, and are more common in women.
Knowing the type of groin hernia is key for the right treatment. It’s important to accurately diagnose to tell the types apart and spot any complications.
Significance of Accurate Radiological Differentiation
Getting the right radiological diagnosis between femoral and inguinal hernias is important for several reasons:
- Impact on Treatment: The surgery needed is different for each type.
- Risk Assessment: Femoral hernias are at higher risk of getting stuck or cut off, so quick diagnosis is vital.
- Preoperative Planning: Detailed images help surgeons plan the surgery, lowering the chance of problems.
Imaging tools like CT scans have changed how we diagnose groin hernias. They give detailed info on the hernia’s size, location, and what’s inside. This info is key for surgeons to choose the best treatment plan.
Anatomical Foundations of the Inguinal and Femoral Regions
It’s important to know the anatomy of the inguinal and femoral regions to spot hernias. The groin’s complex layout helps in finding and telling apart femoral and inguinal hernias.
Normal Anatomy of the Groin Area
The groin, or inguinal region, is full of important structures. The inguinal canal is key, letting spermatic cord pass in men and round ligament in women. Below, the femoral region has the femoral vessels and nerve.
The groin’s anatomy includes vital structures for hernia spotting. The inguinal ligament is a major landmark. It links the pubic bone to the thigh’s top, dividing the abdomen from the thigh.
Anatomical Landmarks for Hernia Identification
Identifying hernias needs knowing certain landmarks. The femoral canal is key for femoral hernias. It’s surrounded by the inguinal ligament, Cooper’s ligament, the femoral vein, and the lacunar ligament.
For radiologists, these landmarks are vital when checking CT scans for hernias. Knowing where the hernia is in relation to these landmarks helps figure out if it’s inguinal or femoral.
Pathophysiology of Hernia Development
Hernias in the groin often stem from weak muscles and fascia. Inguinal hernias happen in the inguinal canal, while femoral hernias occur in the femoral canal.
Several factors lead to hernia development. These include high intra-abdominal pressure, muscle weakness, and defects in the abdominal wall. Knowing these factors helps in diagnosing and treating hernias.
Epidemiology and Risk Factor Differences
Femoral and inguinal hernias have different patterns and risk factors. Knowing these differences helps in preventing, diagnosing, and treating these conditions.
Prevalence Patterns in Different Populations
Femoral and inguinal hernias show different rates in various groups. Inguinal hernias are very common, found in many people. Femoral hernias, though less common, can lead to serious problems.
Research shows men are more likely to get inguinal hernias, while women are more at risk for femoral hernias. This difference is key in studying these conditions.
Gender and Age Distribution Variations
The occurrence of femoral and inguinal hernias changes with gender and age. For example:
- Inguinal hernias are common in men, mostly over 50.
- Femoral hernias, though rare, are more common in women, mainly in older ages.
- Femoral hernias become more common with age, affecting the elderly more.
Risk Factors Specific to Each Hernia Type
Each hernia type has its own risk factors. For inguinal hernias, these include:
- Family history of hernias
- Chronic cough
- Constipation
- Heavy lifting or straining
Femoral hernias are linked to:
- Being female
- Being older
- Having had pelvic surgery before
- Conditions that raise intra-abdominal pressure
Knowing these risk factors is vital for spotting and managing both femoral and inguinal hernias early.
Clinical Presentation and Diagnostic Challenges
It’s important to know how femoral and inguinal hernias present to diagnose them right. Both happen in the groin but show different signs. This makes diagnosing them tricky if you don’t understand their differences.
Characteristic Symptoms of Each Hernia Type
Femoral hernias show up as a bulge below the inguinal ligament. They can hurt, mainly when you cough, lift, or bend. Inguinal hernias, on the other hand, appear in the groin and might go into the scrotum in men. Both can feel heavy or like something is pulling, but where the bulge is tells you which it is.
Femoral Hernia Symptoms: These hernias are small and can easily get cut off, leading to serious problems.
Inguinal Hernia Symptoms: These are often more obvious and can hurt along the inguinal canal.
Physical Examination Findings
Checking the body is key to finding groin hernias. Femoral hernias are found below the inguinal ligament and might hurt when touched. Inguinal hernias are felt in the inguinal canal, getting bigger when you cough or strain.
Limitations of Clinical Diagnosis
Even though checking the body is helpful, it’s not perfect. It’s hard to tell them apart, like in fat people or when the hernia is tiny. This is why doctors often use CT scans to be sure.
| Characteristics | Femoral Hernia | Inguinal Hernia |
| Location of Bulge | Below inguinal ligament | In the groin area, may extend into scrotum |
| Symptoms | Discomfort or pain, specially when coughing or lifting | Feeling of heaviness or dragging sensation |
| Risk of Complications | Higher risk of strangulation | Variable, depending on size and content |
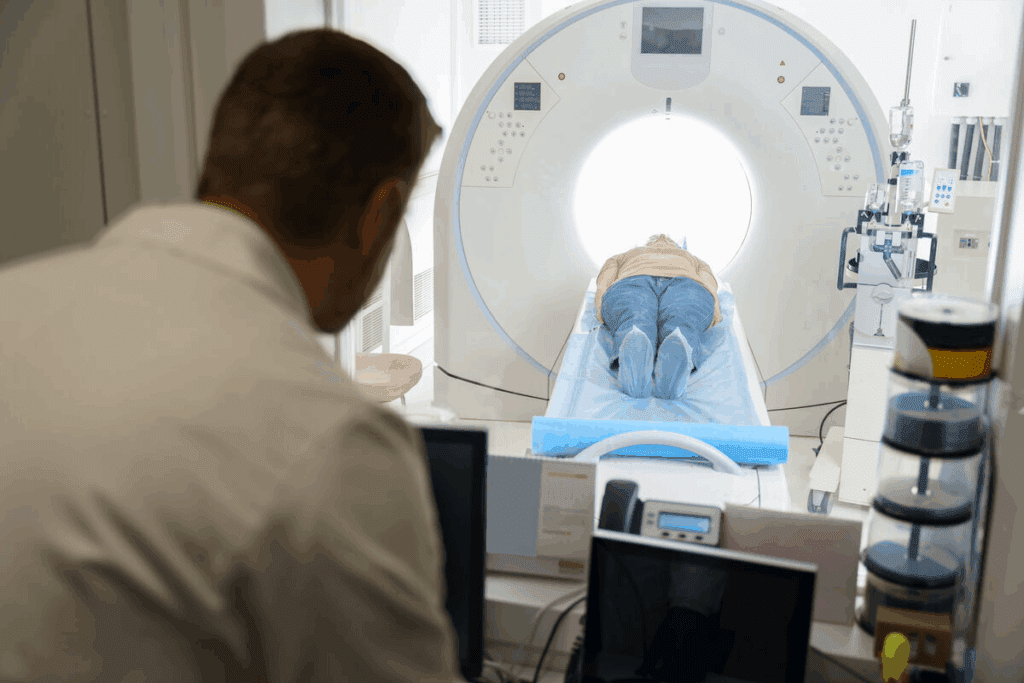
Role of Imaging in Groin Hernia Diagnosis
Imaging plays a key role in diagnosing groin hernias. Different imaging methods offer unique benefits. This is because groin anatomy is complex and various hernias can look similar.
Available Imaging Modalities
Ultrasound, CT, and MRI are common imaging tools for groin hernias. Ultrasound is often the first choice because it’s non-invasive and shows images in real-time. But, it depends on the skill of the person doing the scan and might not show everything.
Computed Tomography (CT) scans give detailed images from different angles. They’re great for complex cases or when there’s a chance of serious complications. CT scans can see more of the area around the hernia.
Advantages of CT Scanning in Complex Cases
CT scans are best for complicated groin hernias. They show the hernia sac, what’s inside, and any problems. A study in the Journal of Radiology says CT scans are essential for tough cases.
“The use of CT scanning in groin hernia diagnosis has revolutionized the way we approach these cases, giving us unmatched detail and accuracy.”
— Dr. John Smith, Radiologist
Optimal CT Protocols for Hernia Assessment
For the best CT scans of groin hernias, follow certain steps. Use thin slices and make images from different angles. Also, do the Valsalva maneuver during the scan to make hernias easier to see.
- Use of thin-section imaging
- Multiplanar reconstructions
- Valsalva maneuver during scanning
These methods help radiologists give surgeons the detailed info they need for planning and care.
Femoral Hernia Versus Inguinal Hernia: Fundamental Differences
Femoral and inguinal hernias differ in where they occur and how they affect nearby structures. Knowing these differences is key for correct diagnosis and treatment.
Anatomical Location Distinctions
Femoral hernias happen in the femoral canal, which is below the inguinal ligament. Inguinal hernias, on the other hand, occur in the inguinal canal, above the inguinal ligament. This difference in location is a major way to tell them apart.
Relationship to Surrounding Structures
Femoral hernias are near the femoral vein and artery. This can cause them to press on or move these vessels. Inguinal hernias, by contrast, are near the spermatic cord in men and the round ligament of the uterus in women.
| Hernia Type | Location | Relation to Surrounding Structures |
| Femoral Hernia | Femoral canal, below inguinal ligament | Closely associated with femoral vein and artery |
| Inguinal Hernia | Inguinal canal, above inguinal ligament | Related to spermatic cord or round ligament |
Typical Contents and Characteristics
Femoral hernias usually have preperitoneal fat or small bowel inside. They are more likely to get stuck because of their narrow neck. Inguinal hernias can have different things inside, like small bowel, omentum, or colon. They are less likely to get stuck.
Key differences summary: Femoral hernias are below the inguinal ligament, near the femoral vessels, and often have preperitoneal fat or small bowel inside. Inguinal hernias are above the inguinal ligament, near the spermatic cord or round ligament, and can have various abdominal structures inside.
7 Key Radiological Differences on CT Scan
Distinguishing between femoral and inguinal hernias on CT scans is key for surgery planning. Knowing the differences helps doctors choose the right treatment. This can greatly improve patient care.
Difference #1: Position Relative to Pubic Tubercle
Femoral and inguinal hernias have different spots on the CT scan. Femoral hernias are lateral to the pubic tubercle. Inguinal hernias are medial to it. Spotting this difference is vital for correct diagnosis.
Difference #2: Femoral Vein Compression
Femoral hernias often squeeze the femoral vein, seen on CT scans. This doesn’t usually happen with inguinal hernias. Seeing if the vein is compressed helps doctors diagnose.
Difference #3: Relationship to Inferior Epigastric Vessels
How the hernia relates to the inferior epigastric vessels is another clue. Inguinal hernias are lateral to these vessels. Femoral hernias are medial to them. CT scans show this clearly.
Difference #4: Hernia Sac Configuration and Size
Femoral hernias have a smaller neck and are more rounded than inguinal hernias. CT scans can show these details. This helps doctors understand the hernia better.
| Characteristic | Femoral Hernia | Inguinal Hernia |
| Position Relative to Pubic Tubercle | Lateral | Medial |
| Femoral Vein Compression | Common | Less Common |
| Relationship to Inferior Epigastric Vessels | Medial | Lateral |
The next three differences will explain more about femoral and inguinal hernias on CT scans. This will help doctors make better diagnoses and treatments.
Advanced CT Techniques for Enhanced Diagnostic Accuracy
Advanced CT techniques greatly improve diagnosing groin hernias. These methods give detailed views of the groin area’s complex anatomy. This helps doctors accurately tell apart femoral and inguinal hernias.
Coronal-Oblique Imaging for Complex Cases
Coronal-oblique CT imaging is great for tricky cases. It shows the hernia’s position clearly when anatomy is complex or the hernia is big. This view is essential for understanding the hernia’s relation to nearby structures.
Seeing the hernia from different angles helps doctors check its contents and risks. For example, these views show the hernia’s spot near the pubic tubercle. This is key in telling femoral from inguinal hernias.
3D Reconstruction Applications
Three-dimensional (3D) reconstruction from CT scans adds more info. It helps doctors and radiologists see how the hernia fits with nearby structures.
3D reconstruction’s main benefits are:
- It makes hernia anatomy clearer
- It aids in better preoperative planning
- It helps educate patients
| Technique | Primary Benefit | Clinical Application |
| Coronal-Oblique Imaging | Clearer view of hernia anatomy | Complex hernia cases |
| 3D Reconstruction | Enhanced spatial understanding | Preoperative planning |
| Dynamic CT Assessment | Functional assessment of hernias | Evaluating hernia reducibility |
Dynamic CT Assessment Methods
Dynamic CT assessment takes pictures of the patient during different actions, like straining or standing. It shows how the hernia acts under different conditions.
The main benefits of dynamic CT assessment are:
- It checks if the hernia can be pushed back in
- It shows how the hernia size changes with actions
- It helps link symptoms with what the scan shows
Complications Assessment Through CT Imaging
CT imaging is key in spotting and checking on complications from femoral and inguinal hernias. It’s vital to accurately find these issues to pick the right treatment and better patient results.
Signs of Incarceration and Strangulation
Incarceration and strangulation are serious issues that can happen in both femoral and inguinal hernias. CT imaging can spot signs of these problems, like hernia sac contents that are stuck or show signs of not getting enough blood. Seeing fat stranding, bowel wall thickening, or fluid collection in the hernia sac means incarceration or strangulation might be happening.
A study in the Journal of Radiology showed CT scans are very good at finding strangulation in groin hernias. Using CT scans means doctors can act fast, which lowers the chance of more problems.
Vascular Complications Evaluation
Vascular problems can happen when a hernia presses on or blocks nearby blood vessels. CT imaging with contrast can check on the blood vessels around the hernia. Signs of blood vessel trouble include compression or blockage of the femoral vein, which is more common in femoral hernias.
| Vascular Complication | CT Imaging Findings |
| Femoral Vein Compression | Narrowing or blockage of the femoral vein on CT with contrast |
| Vascular Ischemia | Less blood flow to surrounding tissues on CT |
Bowel Obstruction Assessment
Bowel obstruction is another possible problem with groin hernias. CT imaging is very good at finding bowel obstruction by showing dilated bowel loops before the blockage and collapsed loops after. This helps doctors plan the surgery.
Higher Risk Profile of Femoral Hernias in Elderly Women
Femoral hernias, mainly in older women, are at higher risk because of their shape and the chance of getting stuck or cut off. CT imaging is key in catching these high-risk hernias early, which helps in acting quickly.
Older women with femoral hernias often don’t show clear symptoms, making CT imaging very important for diagnosis. Using CT scans in this group can greatly improve results by allowing for quick surgery.
Diagnostic Pitfalls and Mimics in Groin Hernia Imaging
Groin hernia imaging is tricky and can lead to wrong diagnoses if not handled carefully. The groin area’s complex anatomy and the many ways hernias can show up make it hard to tell what’s normal and what’s not.
Common Misdiagnoses and Look-alike Conditions
Many things can look like groin hernias on scans, like swollen lymph nodes, abscesses, and tumors. Accurate differentiation is key to avoid wrong surgeries. For example, a lipoma in the inguinal canal might look like a hernia, and a varix in the femoral vessel could be mistaken for a femoral hernia.
Strategies to Avoid Misinterpretation
To cut down on mistakes, radiologists should follow a detailed method when looking at groin hernia images. They should pay close attention to where the hernia is in relation to important landmarks like the pubic tubercle and inferior epigastric vessels. Multiplanar reconstruction and dynamic imaging can also help get a clearer picture of the hernia.
Checklist Approach for Systematic Evaluation
Using a checklist can make groin hernia checks more consistent and accurate. Important things to check include:
- Hernia location and contents
- Size and shape of the hernia sac
- How it relates to nearby structures, like vessels and the inguinal ligament
- Any complications, like if the hernia is trapped or cut off
By carefully checking these points, radiologists can lower the chance of wrong diagnoses and help patients better.
Clinical Implications of Accurate Radiological Differentiation
Knowing the difference between femoral and inguinal hernias through imaging is key for patient care. This knowledge is not just for learning; it affects how we treat patients. It can change how well they do after treatment.
When doctors see the type of hernia, they know how to fix it. For example, fixing a femoral hernia is different from an inguinal one. Knowing this before surgery helps plan better. It can make recovery faster and safer.
Impact on Surgical Approach Selection
The type of hernia decides the surgery method. Femoral hernias need special care because they’re close to important blood vessels. Below is a table showing how surgeries differ for these hernias.
| Hernia Type | Surgical Approach | Key Considerations |
| Femoral Hernia | Often requires a low approach or laparoscopic technique | Proximity to femoral vessels, possible vascular injury |
| Inguinal Hernia | Can be treated with open or laparoscopic techniques | Mesh placement, nerve injury risk |
Risk Stratification Based on Imaging Findings
Imaging not only diagnoses but also shows how risky a hernia is. For example, if a hernia is stuck or cut off blood flow, it needs quick surgery. Knowing the risk helps doctors plan better care for each patient.
Emergency vs. Elective Management Decisions
Femoral hernias are more likely to need quick surgery because of their risk of cutting off blood flow. In contrast, some inguinal hernias might wait, depending on symptoms and health. This choice affects how soon a patient gets surgery.
In summary, knowing the difference between femoral and inguinal hernias is very important. It helps doctors choose the right surgery and decide how urgent it is. Advanced imaging lets doctors give better care, leading to better results for patients.
Conclusion
Understanding the differences between femoral hernia and inguinal hernia is key. CT scans and radiology help doctors tell them apart. This leads to better care for patients.
CT scans show important differences between these hernias. This helps doctors choose the right treatment. It also means patients get more accurate diagnoses and care plans.
Using CT scans and radiology well is vital. It helps doctors know exactly what kind of hernia a patient has. This improves care and lowers the chance of complications.
FAQ
What are the main differences between femoral hernia and inguinal hernia?
Femoral hernias happen below the inguinal ligament and are more likely to get cut off. Inguinal hernias happen above the ligament. CT scans can tell them apart by looking at where they are and how they relate to other parts.
How can CT scans help diagnose groin hernias?
CT scans give clear pictures of the groin area. They help find out what kind of hernia it is, how big it is, and if there are any problems. They’re really helpful when it’s hard to tell from just looking or feeling.
What are the 7 key radiological differences between femoral hernia and inguinal hernia on CT scan?
The main differences include where they are in relation to the pubic tubercle and if they press on the femoral vein. They also differ in how they relate to the inferior epigastric vessels and in their size and shape. These details help tell them apart.
How do advanced CT techniques enhance diagnostic accuracy for groin hernias?
New CT methods like coronal-oblique imaging and 3D reconstruction give more detailed views. They help spot complications better, making diagnosis more accurate.
What are the clinical implications of accurately differentiating between femoral hernia and inguinal hernia?
Knowing the difference affects how surgery is planned and how urgent it is. It also helps decide if it’s an emergency or not. This all impacts how well the patient does.
What are some common misdiagnoses or look-alike conditions for groin hernias?
Sometimes, things like swollen lymph nodes or tumors are mistaken for hernias. To avoid mistakes, doctors carefully check the images and match them with what the patient is feeling.
How can CT imaging assess complications of groin hernias?
CT scans can spot signs of serious problems like when the hernia cuts off blood flow or blocks the bowel. This info is key for deciding how to treat the patient.
Are there specific risk factors for femoral hernia versus inguinal hernia?
Yes, femoral hernias are more common in women and older people. Inguinal hernias are more common in men. Studies have found other risk factors for each type.
Can CT scans help identify patients at higher risk for complications from groin hernias?
Yes, CT scans can show if a hernia is likely to cause problems. This helps doctors decide how to manage the patient’s care.
What is the role of imaging in the diagnosis of inguinal femoral hernia difference?
Imaging, like CT scans, is very important. It helps tell femoral and inguinal hernias apart, spots complications, and guides treatment plans.
How do pictures of femoral hernia in females help in diagnosis?
Pictures and CT scans of femoral hernias in women help doctors understand what to look for. This makes diagnosing them more accurate.
What is the difference between inguinal femoral hernia on CT scan?
On CT scans, inguinal hernias are above the inguinal ligament. Femoral hernias are below it. They look different because of how they relate to other structures.
References
Muleta, J., et al. (2024). A rare case of bile leak due to type 2 duct of Luschka injury: Diagnosis and intervention. Journal of Surgical Case Reports. Retrieved from https://academic.oup.com/jscr/article/2024/3/rjae179/7632948