Gastroenterology covers the digestive system. It focuses on diagnosing, treating, and managing conditions of the stomach, intestines, liver, and pancreas.
Send us all your questions or requests, and our expert team will assist you.

Irritable Bowel Syndrome is a chronic functional gastrointestinal condition characterized by recurring abdominal discomfort and changes in bowel habits without visible structural damage to the intestines. The digestive tract appears normal on examination, yet its function is altered in a way that leads to persistent or intermittent symptoms. This functional nature is central to understanding why symptoms can be significant even when medical tests do not show abnormalities.
In everyday life, Irritable Bowel Syndrome means that the intestines respond more strongly than expected to routine digestive processes. Eating, bowel movements, emotional stress, and even normal gas production may trigger discomfort. Symptoms often follow a fluctuating course, with periods of relative stability alternating with flare-ups. While the condition does not cause permanent injury to the bowel, it can substantially affect daily comfort, confidence, and quality of life if not properly understood and managed.

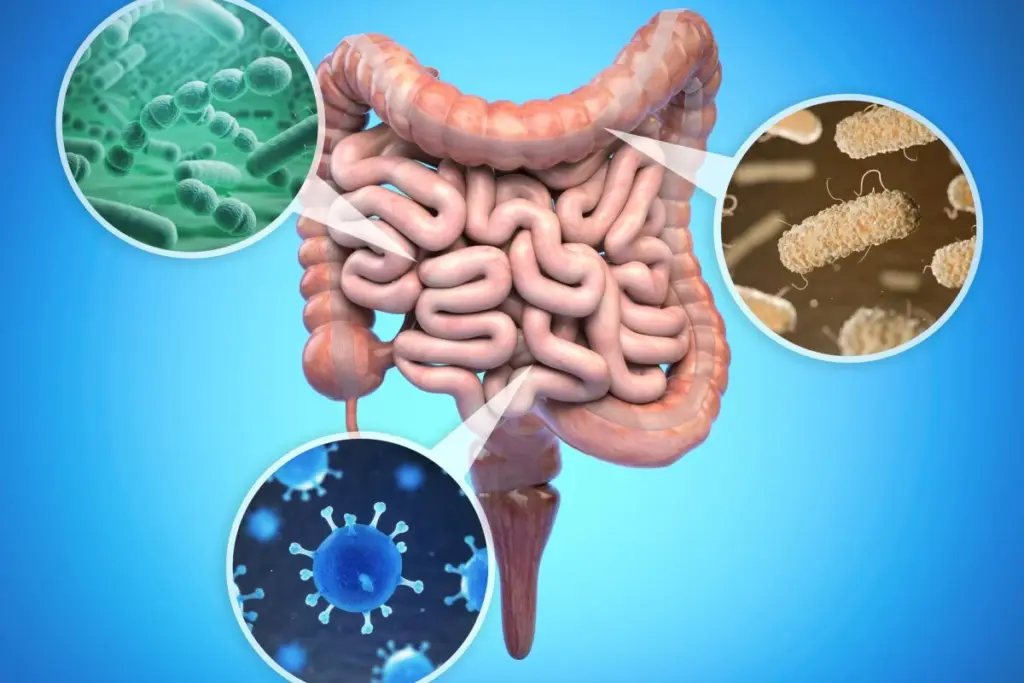
Under normal conditions, the intestines move food forward through coordinated muscle contractions while sensory nerves transmit minimal signals to the brain. In Irritable Bowel Syndrome, this balance is disrupted. The bowel may contract too quickly, too slowly, or irregularly, while sensory pathways become overly responsive.
This heightened sensitivity means that normal levels of stretching, gas, or stool are perceived as uncomfortable or painful. The gut becomes less tolerant of routine digestive activity, leading to cramping, bloating, and urgency. These functional changes occur at a microscopic and neurological level rather than through visible tissue damage, which explains why the condition is classified as functional rather than structural.

The symptoms of Irritable Bowel Syndrome vary widely between individuals and may change over time in the same person. Abdominal pain is a defining feature and is typically cramping in nature. It often improves after bowel movements, reflecting the link between discomfort and altered bowel function.
Bloating is another prominent symptom and may present as a sensation of fullness, pressure, or visible abdominal distension. Many individuals also experience changes in bowel habits, including diarrhea, constipation, or alternating patterns. Urgency, irregular timing of bowel movements, and a feeling of incomplete emptying are also commonly reported. These symptoms may intensify after meals, during stressful periods, or when daily routines are disrupted.
Although Irritable Bowel Syndrome primarily affects the digestive tract, its impact often extends beyond the intestines. Many individuals report fatigue, sleep disturbances, headaches, and generalized body discomfort. These symptoms reflect the close interaction between the digestive system and the nervous system.
The persistent nature of digestive discomfort can contribute to mental strain, heightened body awareness, and reduced energy levels. Sleep quality may decline when abdominal discomfort or urgency interferes with rest. These non-digestive symptoms do not indicate separate disease processes but rather highlight the systemic effects of chronic gut–brain interaction.
A defining feature of Irritable Bowel Syndrome is the strong connection between the digestive system and the brain. This relationship, often referred to as the gut–brain axis, involves complex communication through neural, hormonal, and immune pathways.
Emotional stress, anxiety, and psychological strain can directly influence intestinal movement and sensitivity. In turn, digestive discomfort sends distress signals back to the brain, reinforcing symptom awareness and stress responses. This bidirectional loop explains why symptoms often worsen during emotionally demanding periods and why addressing stress is an important component of long-term management.

Irritable Bowel Syndrome does not arise from a single cause. Instead, symptoms develop through the interaction of multiple factors that affect gut function and sensitivity. Lifestyle patterns such as irregular eating habits, inconsistent sleep, and sedentary routines can disrupt digestive rhythm and increase symptom frequency.
Biological factors also play a role, including heightened sensitivity of intestinal nerves, hormonal fluctuations, and individual stress reactivity. A history of digestive disturbances may further sensitize the gut. These influences do not act in isolation but combine over time to shape symptom patterns and intensity.

Irritable Bowel Syndrome does not arise from a single cause. Instead, symptoms develop through the interaction of multiple factors that affect gut function and sensitivity. Lifestyle patterns such as irregular eating habits, inconsistent sleep, and sedentary routines can disrupt digestive rhythm and increase symptom frequency.
Biological factors also play a role, including heightened sensitivity of intestinal nerves, hormonal fluctuations, and individual stress reactivity. A history of digestive disturbances may further sensitize the gut. These influences do not act in isolation but combine over time to shape symptom patterns and intensity.
Diagnosis of Irritable Bowel Syndrome is based on characteristic symptom patterns rather than visible disease markers. The evaluation process focuses on identifying recurring abdominal pain associated with changes in bowel habits while excluding other conditions that may cause similar symptoms.
The absence of structural abnormalities is not a diagnostic weakness but a defining feature of the condition. Recognizing Irritable Bowel Syndrome as a functional disorder helps validate patient experience and supports appropriate management strategies that focus on symptom control and quality of life rather than invasive intervention.
Management of Irritable Bowel Syndrome emphasizes consistency, awareness, and adaptability rather than rigid control. Because symptoms fluctuate, long-term success depends on recognizing early signs of flare-ups and adjusting habits accordingly.
Regular daily routines, balanced activity, stress awareness, and attention to digestive signals all contribute to symptom stability. Management is not about eliminating all discomfort but about reducing symptom intensity and restoring confidence in daily life. Over time, many individuals learn which patterns support comfort and which increase vulnerability.

Living with Irritable Bowel Syndrome involves developing a practical understanding of the condition and integrating supportive habits into everyday life. While the condition does not cause permanent intestinal damage, unmanaged symptoms can interfere with work, travel, social activities, and emotional well-being.
With informed awareness and consistent routines, quality of life can improve significantly. At Liv Hospital, Irritable Bowel Syndrome is approached as a functional gastrointestinal condition requiring individualized understanding of symptom patterns, gut physiology, and lifestyle influences. This perspective supports sustainable management, improved comfort, and long-term well-being.
Send us all your questions or requests, and our expert team will assist you.
It is a functional digestive condition characterized by abdominal discomfort and altered bowel habits without structural damage.
No. Symptoms often fluctuate, with periods of improvement and flare-ups.
No. It does not cause permanent injury to intestinal tissue.
Yes. Stress strongly influences gut sensitivity and bowel function.
Yes. With consistent habits and awareness, many people achieve good symptom control.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)