Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 1 in 5 adults in the United States will have gastrointestinal surgery at some point. It’s a key part of medical care.
Gastrointestinal surgery treats many digestive system issues. This includes problems with the colon, stomach, pancreas, liver, and gallbladder.
These surgical procedures are complex. They need a lot of skill and precision. This article will explain the different GI surgeries and their techniques.
Overview of the methods for gastrointestinal surgery, including open, laparoscopic, and robotic approaches.
Key Takeaways
- GI surgery includes many procedures, like colon and stomach surgery.
- The techniques used depend on the condition being treated.
- There are many surgical methods for digestive system issues.
- GI surgery requires a lot of skill and precision.
- Knowing about different GI surgeries helps patients prepare.
The Scope of Gastrointestinal Surgery
Gastrointestinal surgery covers a wide range of procedures. These are key for treating many digestive system disorders. They help with issues in the esophagus, stomach, small intestine, colon, rectum, and more.
Definition and Common Indications
Gastrointestinal surgery treats digestive system conditions. It’s used for cancers, severe injuries, blockages, and problems like appendicitis or gallstones. Minimally invasive techniques, like laparoscopic surgery, are popular. They help in reducing recovery time and scarring.
A leading surgeon notes, “Surgical techniques have improved a lot. Now, we can do more precise and less invasive procedures.” This change has been a big step forward.
“Surgical techniques have evolved dramatically, giving patients more options and better results.”
Evolution of Digestive System Surgical Techniques
New surgical techniques have led to laparoscopic and minimally invasive procedures. These methods cut down on recovery time and scarring. While traditional open surgery is used for complex cases, the trend is towards less invasive methods.
- Laparoscopic surgery uses small incisions for instruments and a camera.
- Robotic-assisted surgery offers better precision and control.
- Endoscopic procedures diagnose and treat without external cuts.
These advancements have changed the field. Surgeons can now do complex procedures with more precision and less harm to patients. Patients get to leave the hospital sooner, feel less pain, and recover faster.
Patient Evaluation and Surgical Candidacy
Checking if a patient is right for gastrointestinal surgery is key. It helps pick the best surgery and lowers risks.
Diagnostic Workup
A detailed check is needed to know the patient’s health. This includes imaging, endoscopy, and lab tests.
- Imaging Studies: CT scans, MRI, and ultrasound show the GI tract and find problems.
- Endoscopic Examinations: Upper GI endoscopy and colonoscopy let doctors see the inside and take samples.
- Laboratory Tests: Blood tests and other tests check the patient’s health and find issues.
Risk Assessment and Stratification
Knowing the risks is important. It finds factors that could lead to surgery problems.
| Risk Factor | Description | Mitigation Strategy |
| Age | Older patients may face more risks because of health issues. | Geriatric assessment is done. |
| Comorbid Conditions | Heart disease, diabetes, etc., raise surgery risks. | Health is improved before surgery. |
| Nutritional Status | Being underweight can slow healing and increase infection risk. | Nutrition is improved. |
Determining the Optimal Surgical Approach
The right surgery depends on the condition, patient health, and surgeon skill.
Minimally invasive techniques, like laparoscopy, are chosen when possible. They help in faster recovery and less scarring.
In summary, evaluating patients and choosing the right surgery are essential. They involve detailed checks, risk assessment, and picking the best surgery. This way, doctors can ensure better results and safety for patients.
Major Types of Gastrointestinal Surgery
There are many different types of gastrointestinal surgeries. They range from fixing the esophagus to working on the colon. These surgeries are key in treating many digestive problems. They can cure or help manage symptoms.
Esophageal Procedures
Esophageal surgery treats issues like cancer, achalasia, and GERD. Some common surgeries are:
- Esophagectomy: This is when part or all of the esophagus is removed, often for cancer.
- Heller Myotomy: It’s a surgery to ease achalasia by cutting muscles at the esophagus end.
- Fundoplication: This surgery wraps the stomach around the esophagus’s lower part to treat GERD.
Stomach and Duodenal Surgery
These surgeries target the stomach and duodenum for ulcers, cancer, and more. Key surgeries include:
- Gastrectomy: This is removing part or all of the stomach, often for cancer or severe ulcers.
- Vagotomy: It involves cutting the vagus nerve to lower stomach acid.
- Duodenal resection: This is removing part of the duodenum, needed for duodenal cancer or ulcers.
Small Intestine Operations
Operations on the small intestine treat issues like blockages, Crohn’s disease, and tumors. Common surgeries are:
- Resection and anastomosis: This involves removing the sick part of the intestine and joining the healthy ends.
- Strictureplasty: It widens a narrowed intestine section, often in Crohn’s disease.
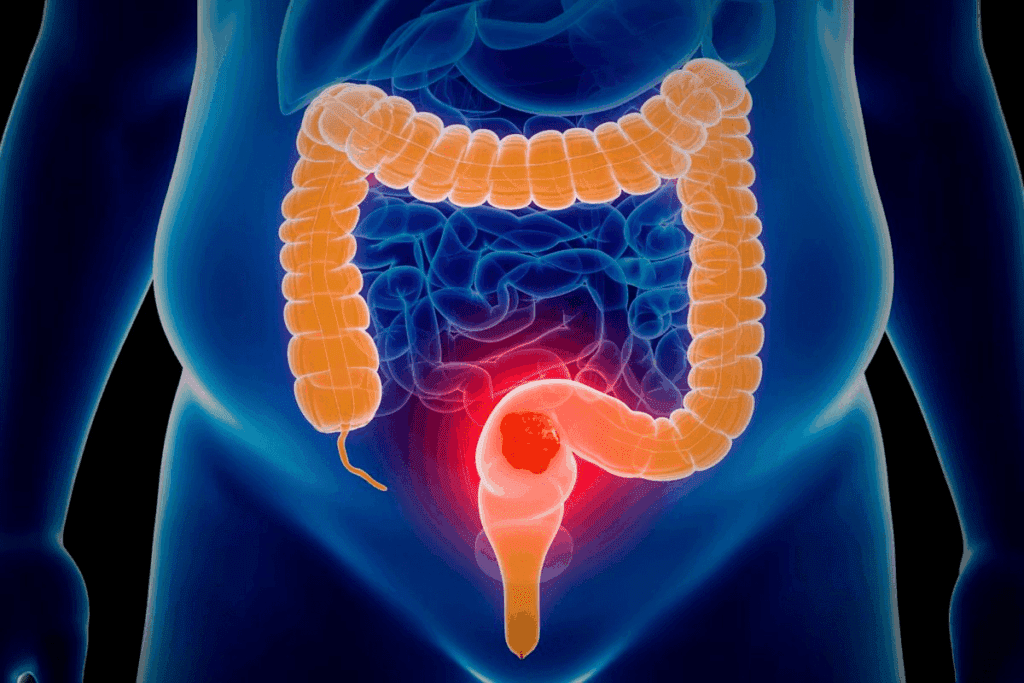
Colorectal Surgical Procedures
Colorectal surgery tackles problems like cancer, diverticulitis, and inflammatory bowel disease. Some procedures are:
- Colectomy: This is removing part or all of the colon.
- Proctectomy: It involves removing the rectum, sometimes with a colectomy.
- Low anterior resection: This surgery removes the sick part of the rectum and connects the colon.
These surgeries are vital in managing gut diseases. They improve patient outcomes and quality of life.
Hepatobiliary and Pancreatic Surgical Procedures
Hepatobiliary and pancreatic surgeries are complex. They need a lot of skill and care. These operations help treat problems with the liver, gallbladder, and pancreas.
Liver Resection and Transplantation
Liver resection and transplantation are big surgeries. Liver resection means taking out part of the liver. This is done for liver tumors or damaged liver.
Liver transplantation is for those with very sick livers. It replaces the sick liver with a healthy one from a donor.
- Liver resection is for liver tumors or damage.
- Liver transplantation is for very sick livers.
Gallbladder Surgery Techniques
Gallbladder surgery, or cholecystectomy, treats gallstones and diseases. There are two ways: laparoscopic cholecystectomy and open cholecystectomy.
- Laparoscopic cholecystectomy is less invasive, leading to quicker recovery and less pain.
- Open cholecystectomy is for harder cases or when laparoscopic surgery can’t be done.
Pancreatic Surgery Approaches
Pancreatic surgery is very complex. It includes the pancreaticoduodenectomy (Whipple procedure) for pancreatic cancer. The surgery choice depends on the patient’s health and the disease.
- The Whipple procedure removes the pancreas head, duodenum, and bile duct part.
- Other surgeries like distal pancreatectomy and total pancreatectomy depend on the disease’s extent and location.
Open Gastrointestinal Surgery Techniques
Open gastrointestinal surgery has improved a lot over the years. This is to help patients get better results from complex digestive system surgeries.
Incision Types and Placement
The right incision type and placement are key to open gastrointestinal surgery success. Surgeons look at several things. These include the patient’s body, the surgery type, and the need for good exposure.
There are different incisions like midline laparotomy, transverse, and paramedian. Each is picked for the surgery’s specific needs.
Exposure and Retraction Methods
Exposure and retraction are very important for open gastrointestinal surgery. Surgeons use many retractors and methods to keep the area clear.
Retractors can be self-retaining or handheld. The choice depends on the surgery’s needs and the surgeon’s preference.
Traditional Surgical Instruments
Traditional surgical instruments are a big part of open gastrointestinal surgery. These tools have gotten better to give surgeons the precision and control they need.
Scalpels, forceps, and retractors are key tools. Surgeons use them to do surgeries safely and well.
Laparoscopic Approaches to GI Surgery
Laparoscopic surgery has changed GI surgery a lot. It uses less invasive methods. This has made recovery times shorter and reduced complications for patients.
Port Placement and Access Techniques
The success of laparoscopic GI surgery depends on good port placement and access. Surgeons need to plan port placement carefully to get the best access to the area being operated on.
Ultrasound-guided access is getting more popular. It helps surgeons enter the abdominal cavity more precisely. This reduces the risk of harming nearby structures.
- Initial access is usually through the umbilicus.
- More ports are added based on the procedure needed.
- Optical trocars help with better vision during port placement.
Specialized Equipment and Instruments
Laparoscopic GI surgery uses special tools and equipment. This includes high-definition cameras, insufflators, and laparoscopic instruments like graspers and dissectors.
| Equipment | Description | Application in GI Surgery |
| High-Definition Camera | Provides clear vision of the surgical area. | Needed for all laparoscopic GI surgeries. |
| Insufflator | Keeps the air in the abdomen. | Important for a clear operating field. |
| Laparoscopic Graspers | Helps with tissue manipulation. | Used in dissection and retraction during GI surgery. |
Conversion Criteria to Open Surgery
Even with laparoscopic surgery’s advancements, sometimes open surgery is needed. This decision is made when the procedure is too complex, there are unexpected complications, or there’s not enough visibility.
Clear criteria for conversion include not being able to progress, significant bleeding, or too many adhesions that can’t be managed laparoscopically.
- Deciding on conversion based on the case’s complexity.
- Making quick decisions to avoid more problems.
- Being ready for open surgery from the start is important.
Robotic-Assisted Digestive System Surgery
Robotic-assisted surgery has made complex GI procedures easier and more precise. It uses advanced technology for better visualization and control. This allows surgeons to do detailed operations with more skill.
Technical Setup and Operation
The setup for robotic surgery includes a complex system, a surgeon’s console, and a team. First, ports are set for the robotic arms. Then, the robot is docked and the area is prepared for surgery.
Key components of the technical setup include:
- High-definition 3D visualization system
- Robotic arms with wristed instruments
- Surgical console for the operating surgeon
Advantages in Complex GI Procedures
Robotic surgery brings many benefits, like better precision and less blood loss. It also means less pain after surgery. The technology helps surgeons do complex tasks more easily.
The benefits of robotic-assisted surgery are most seen in:
- Complex resections and reconstructions
- Delicate dissections around vital structures
- Procedures requiring precise suturing
Learning Curve and Training Requirements
Learning robotic surgery is a big challenge. It needs special training and practice. Surgeons go through detailed programs to learn the skills.
Key elements of training programs include:
- Familiarization with the robotic system and its operation
- Practice in a simulated environment
- Proctored cases to gain hands-on experience
Endoscopic Gastrointestinal Procedures
Gastrointestinal endoscopy is key in treating many digestive issues. It’s a precise, less invasive way compared to old surgery methods. These procedures let doctors see inside the GI tract, helping diagnose and treat digestive problems.
Upper and Lower Endoscopy Techniques
Endoscopy is split into upper and lower types. Upper endoscopy looks at the esophagus, stomach, and duodenum with a camera tube. It’s used to find issues like esophagitis and ulcers. Lower endoscopy, or colonoscopy, checks the colon and rectum for polyps and cancer.
Both upper and lower endoscopy have improved with new tech. High-definition and chromoendoscopy make it easier to see and diagnose problems.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP uses endoscopy and X-rays to look at bile and pancreatic ducts. It’s great for treating bile duct blockages and pancreatitis. ERCP can also do things like remove stones and place stents.
ERCP’s success relies on the doctor’s skill and the tools used. New tech, like digital cholangiopancreatography, has made it safer and more precise.
Advanced Interventional Endoscopy
Advanced interventional endoscopy includes treatments beyond just looking. It can remove early cancers and big polyps without surgery. Techniques like endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are part of this.
Other advanced methods include endoscopic ultrasound (EUS)-guided treatments. These help diagnose and treat things like pancreatic cysts. New tools and methods keep improving what interventional endoscopy can do.
In summary, endoscopic GI procedures are essential today. They offer non-invasive ways to diagnose and treat. As tech gets better, these methods will likely become even more effective and common.
Pre-Operative Preparation for GI Surgery
Getting ready for GI surgery is key to its success. It includes steps to make the patient’s body ready, lower risks, and help with recovery.
Bowel Preparation Protocols
Cleaning the bowel is a big part of getting ready for GI surgery. It helps avoid infections and lets the surgeon see better during the surgery.
Patients often follow a special diet and take laxatives or enemas. The exact steps depend on the surgery, the patient’s health, and the surgeon’s advice.
- Dietary Restrictions: Patients might eat only clear liquids for a day or two before surgery.
- Laxatives: These are used to clean out the bowel.
- Enemas: Sometimes, enemas are used to clean the lower bowel.
Nutritional Optimization
Being well-nourished is important for recovery after surgery. Pre-surgery, the focus is on making sure the patient is as healthy as possible.
This might include special diets, supplements, or even feeding through an IV for those who are very malnourished.
| Nutritional Element | Pre-Operative Goal | Potential Interventions |
| Protein | Optimize protein levels | High-protein diet, supplements |
| Hydration | Ensure adequate hydration | Fluid intake guidance |
| Vitamins and Minerals | Correct deficiencies | Supplementation |
Medication Management
Managing medications is also very important before surgery. The goal is to lower the risk of bleeding and other problems by adjusting the patient’s meds.
This might mean stopping some medications, like blood thinners, and changing the doses of others. It’s important for patients to tell their healthcare team about all their medications.
By managing bowel prep, nutrition, and medications well, patients can be best prepared for GI surgery. This reduces risks and improves results.
Anesthesia and Monitoring During Gastrointestinal Surgery
In gastrointestinal surgery, anesthesia does more than just manage pain. It keeps the patient stable during complex surgeries. Good anesthesia and monitoring are key to keeping patients safe and comfortable.
Anesthetic Considerations for Abdominal Procedures
Choosing the right anesthesia for gastrointestinal surgery is important. It depends on the patient’s health, the surgery type, and other medications. General anesthesia is often used, but regional anesthesia might be better for some patients and surgeons.
| Anesthetic Type | Characteristics | Use in GI Surgery |
| General Anesthesia | Induces unconsciousness and analgesia | Commonly used for most GI surgeries |
| Regional Anesthesia | Numbness in a specific region of the body | Used for certain procedures, for post-operative pain relief |
Intraoperative Monitoring Techniques
Monitoring during surgery is critical. It helps catch any changes in the patient’s condition. This includes watching vital signs like heart rate and blood pressure. Advanced methods might include invasive blood pressure monitoring or transesophageal echocardiography for complex cases.
Pain Management Strategies
Pain control is a big part of gastrointestinal surgery. Multimodal analgesia uses different pain medicines to reduce side effects. Enhanced Recovery After Surgery (ERAS) protocols often use these methods to help patients recover better.
By managing anesthesia and monitoring well, healthcare providers can make surgery safer and better for patients. Using advanced monitoring and pain control strategies is essential for these improvements.
The Step-by-Step Process of Gastrointestinal Surgery
Understanding the steps of gastrointestinal surgery is key for both patients and surgeons. This detailed process includes several important stages. These stages help ensure the best results for patients.
Initial Access and Exploration
The first step is getting initial access to the surgical area. This can be done through open surgery or laparoscopy. Laparoscopy uses small incisions for a camera and tools, allowing for a detailed look at the tract.
After gaining access, the surgeon explores the abdominal cavity. They look for any abnormalities or disease. This step helps plan the surgery.
Identification and Management of Pathology
The surgeon then finds the problem that needs surgery. They use visual inspection, touch, or tools like ultrasound. They might take biopsies or remove diseased tissue.
- Visual inspection to identify visible abnormalities
- Palpation to detect abnormalities not visible on the surface
- Intraoperative ultrasound for detailed imaging
Resection and Reconstruction Techniques
The next step is removing the diseased part of the tract. Resection techniques depend on the disease’s location and size. Then, the tract is rebuilt to keep it working right. This might involve anastomosis, connecting healthy parts.
- Resection of the diseased segment
- Reconstruction through anastomosis or other techniques
Closure and Wound Management
The last step is closing the surgical site. This is done with sutures, staples, or other methods. Good wound management is key to avoid problems like infection.
“Proper wound closure is a critical aspect of postoperative care, significantly impacting patient recovery and outcomes.”
By following these steps, surgeons can make sure surgery is done safely and well. This leads to the best results for patients.
Emergency vs. Elective Gastrointestinal Surgery
Gastrointestinal emergencies need immediate surgery, unlike elective surgeries which are planned. Knowing the difference is key to choosing the right surgery and improving patient care.
Acute Abdomen Management
Managing acute abdomen means quickly finding and treating problems like appendicitis or bowel obstruction. Emergency surgery for these issues must be fast and effective to avoid more harm.
Key considerations include quick assessment, right imaging, and timely surgery. The aim is to fix the problem and reduce risks of death or serious illness.
Trauma-Related GI Procedures
Trauma-related GI surgeries are vital for fixing digestive system injuries from accidents. These surgeries need a team effort from trauma surgeons, radiologists, and others.
The main goals are to stop bleeding, fix damaged areas, and get the GI system working right again. These complex surgeries require great skill and precision.
Modified Approaches in Emergency Settings
Emergency GI surgery often means using different methods than planned surgeries. This can include special incisions, different positions, or special tools.
In emergencies, surgeons must be flexible, making fast decisions based on the patient’s condition. Being able to adapt quickly is essential for the best results in urgent situations.
Post-Operative Care and Recovery
Good post-operative care is key for a smooth recovery after stomach surgery. It focuses on managing pain, avoiding complications, and keeping the patient healthy.
Immediate Post-Surgical Monitoring
Right after GI surgery, patients are watched closely in the recovery room. They check vital signs, manage pain, and look for bleeding or other problems.
Monitoring protocols help spot and fix any issues fast. This keeps the patient safe and comfortable at the start of their recovery.
Pain Control Approaches
Managing pain is a big part of post-operative care. Doctors use medicines, regional anesthesia, and other methods to keep pain under control.
A multidisciplinary approach means surgeons, anesthesiologists, and others work together. They make a pain plan that fits each patient’s needs.
Early Mobilization Protocols
Moving early is important to avoid problems like blood clots and to help recovery. Patients start moving and walking soon after surgery.
Mobilization protocols are safe and effective. They consider the patient’s health and the surgery type.
Dietary Progression After GI Surgery
Managing diet is a big part of post-operative care. Moving from liquids to solid foods is planned carefully to ensure it’s safe and well-tolerated.
Nutritional advice is given to help the patient recover well and stay healthy after surgery.
Minimally Invasive Innovations in GI Surgery
The field of GI surgery is seeing big changes with new, less invasive methods. These new techniques are making surgery better for patients. They help with faster recovery, less pain, and better looks after surgery.
Single-Incision Laparoscopic Surgery
Single-incision laparoscopic surgery is a big step forward. It uses just one small cut, usually at the belly button. This means less scarring and possibly less pain after surgery. It also looks better after healing.
Doctors use special tools to do surgeries like removing the gallbladder or appendix through this method.
Natural Orifice Transluminal Endoscopic Surgery (NOTES)
NOTES surgery is even more advanced. It’s done through a body opening like the mouth or vagina, without any cuts on the outside. It aims to cause less damage and help patients heal faster. But, it needs special training and tools.
NOTES is new in GI surgery but could be very promising for the future.
Fluorescence-Guided Surgery
Fluorescence-guided surgery uses special dyes to light up body parts during surgery. It helps doctors see important areas like blood vessels and ducts. This makes surgeries safer and more precise. Near-infrared light is very useful for surgeries like liver removals.
Artificial Intelligence Applications
Artificial intelligence is starting to help in GI surgery. It helps with planning before surgery, making decisions during it, and caring for patients after. AI looks at lots of data to guess how well a patient will do and find problems early. It’s also being used with robots to make surgeries even more precise.
These new methods are making GI surgery better for patients. As technology gets better, we’ll see even more improvements in the future.
Conclusion
Gastrointestinal surgery includes many procedures and techniques. These aim to improve patient results. The different methods, like open, laparoscopic, and robotic-assisted, bring benefits. These include shorter recovery times and better precision.
It’s important to know the different surgical techniques for better treatment plans. Choosing the right technique for each patient can greatly improve patient outcomes. New advancements in surgery, like minimally invasive methods, are key to these improvements.
The future of gastrointestinal surgery looks bright. It will keep being a key part of healthcare, solving many digestive problems. Healthcare workers need to stay up-to-date with new techniques to give the best care.
FAQ
What is gastrointestinal surgery?
Gastrointestinal surgery deals with the digestive system. This includes the esophagus, stomach, small intestine, colon, liver, gallbladder, and pancreas. It uses different methods like open surgery, laparoscopic surgery, robotic-assisted surgery, and endoscopic procedures.
What are the common indications for gastrointestinal surgery?
Common reasons for GI surgery include gallstones, hernias, and inflammatory bowel disease. Cancer and gastrointestinal bleeding are also common reasons. Other conditions like appendicitis, diverticulitis, and bowel obstruction may also require surgery.
What is the difference between open and laparoscopic gastrointestinal surgery?
Open surgery makes a big cut in the abdomen. Laparoscopic surgery uses small cuts and a laparoscope. Laparoscopic surgery is less painful and leads to quicker recovery.
What is robotic-assisted digestive system surgery?
Robotic-assisted surgery uses a robotic system to help the surgeon. It offers clear views, precise cuts, and better control. This makes it great for complex GI surgeries.
What is the role of endoscopy in gastrointestinal surgery?
Endoscopy helps surgeons see inside the digestive tract. It’s used to diagnose and treat conditions. Endoscopic retrograde cholangiopancreatography (ERCP) is used for bile and pancreatic duct issues.
How is pain managed during and after gastrointestinal surgery?
Pain management uses anesthetics, pain meds, and other methods. Anesthesiologists work with surgeons to create a pain plan for each patient.
What is the importance of pre-operative preparation for GI surgery?
Preparing before surgery is key. It reduces risks and improves outcomes. This includes bowel prep, nutrition, and managing medications.
What are the benefits of minimally invasive gastrointestinal surgery?
Minimally invasive surgery has many benefits. It reduces pain, speeds up recovery, and lowers risks. It also allows for more precise and accurate procedures.
What is the role of artificial intelligence in gastrointestinal surgery?
Artificial intelligence helps in planning and improving surgery. AI analyzes data, finds patterns, and offers insights. This helps surgeons make better decisions.
How is post-operative care managed after gastrointestinal surgery?
Post-operative care includes monitoring, pain management, and support. It involves early movement, diet, and follow-up visits. This helps patients recover smoothly.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10724411/