Last Updated on November 27, 2025 by Bilal Hasdemir

Knowing how glioblastoma multiforme progresses is key for patients and their families. It helps them understand brain cancer care better. We aim to be clear and caring in meeting their needs.
Patients usually live 12-15 months after being diagnosed. When treatments stop working, they often move to hospice brain tumor care. We offer full support, like managing symptoms and end-of-life care, to improve their life quality.
At Liv Hospital, we follow international standards and put patients first. We offer support and confidence to families facing brain cancer challenges.
Key Takeaways
- Understanding the GBM timeline is key for care planning.
- Glioblastoma multiforme is a fast-growing brain cancer.
- Hospice care focuses on symptom management and family support.
- Typical survival time after diagnosis is 12-15 months.
- Switching to hospice care is a big step in care.
Understanding Glioblastoma Multiforme (GBM)

It’s important for patients and doctors to understand Glioblastoma Multiforme (GBM). This brain cancer is aggressive and needs a detailed plan to manage it. This plan helps patients live better despite the challenges.
What is GBM and Its Impact on the Brain
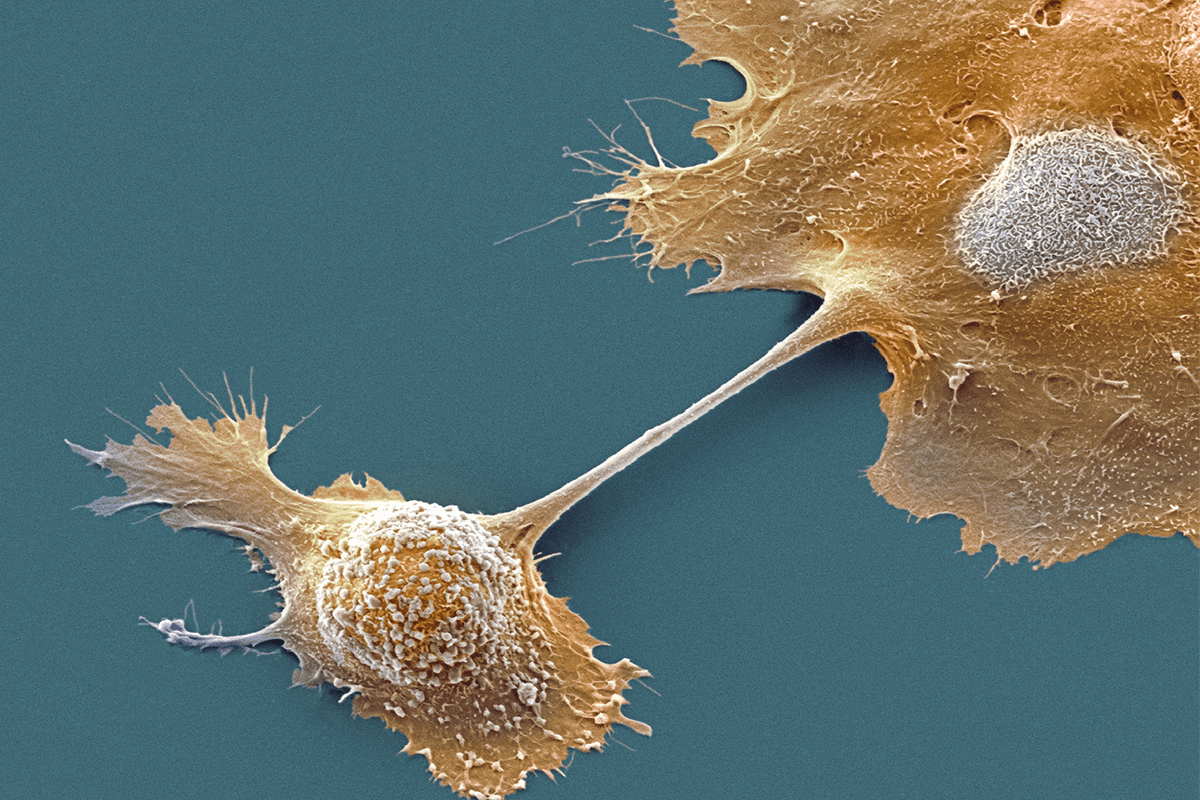
Glioblastoma Multiforme (GBM) starts in the brain’s glial cells. It’s known for being very aggressive and hard to treat. GBM can harm the brain a lot, causing many symptoms and problems.
GBM affects the brain in many ways. It can cause seizures, headaches, and problems with thinking. As it grows, it can also increase pressure inside the skull, making things worse.
Typical 12-15 Month Survival Trajectory
GBM patients usually live 12-15 months after being diagnosed. This time can vary based on the patient’s age, health, and treatment success.
Studies show that GBM’s genetics and the brain’s environment are key to its fast growth. Knowing this helps doctors find better ways to treat it.
| Survival Period | Typical Characteristics |
|---|---|
| 0-3 months | Initial diagnosis, surgery, and beginning of adjuvant therapy |
| 3-6 months | Continuation of adjuvant therapy, possible tumor return |
| 6-12 months | Disease gets worse, looking into new treatments or care for comfort |
| 12-15 months | Disease is very advanced, focus on managing symptoms and quality of life |
Why GBM Progresses Differently Than Other Cancers
GBM is different from other cancers because of its genetics and the brain’s environment. The blood-brain barrier makes it hard to treat GBM effectively.
GBM can quickly become resistant to treatments, leading to its return. This shows the need for new and tailored treatments to help patients more.
The Complete GBM Timeline: From Diagnosis to End-Stage

The journey from diagnosis to end-stage GBM has many key phases. Patients and caregivers need to understand these phases. We will cover the GBM timeline, from symptoms and diagnosis to supportive care.
Initial Symptoms and Diagnostic Phase
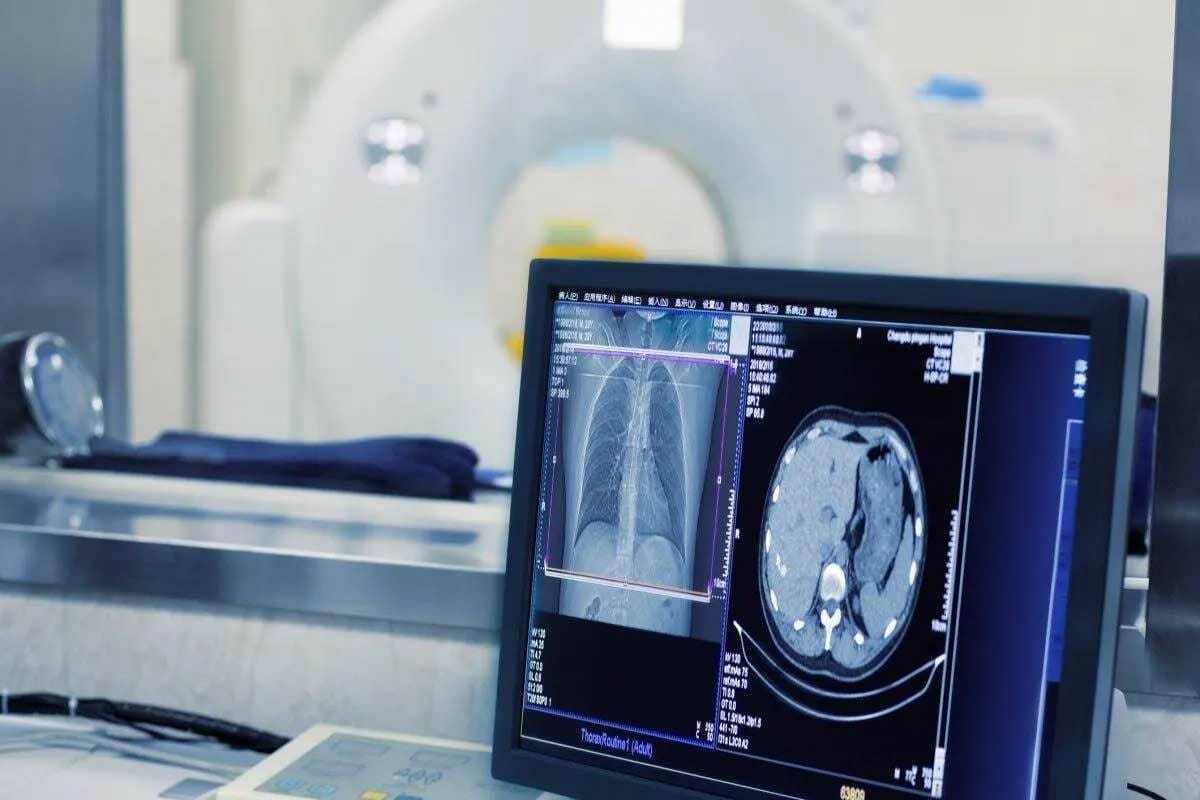
GBM symptoms start subtly, like headaches, seizures, or changes in thinking. As symptoms grow, patients get tested with MRI scans and biopsies. This confirms GBM. Early diagnosis is key to managing the disease well.
Early diagnosis helps doctors create a treatment plan that fits the patient. Research shows early action can greatly improve GBM patients’ lives.
Active Treatment Period
After diagnosis, patients start active treatment. This may include surgery, radiation, and chemotherapy. We help choose the best treatment based on the tumor and patient’s health.
The aim of active treatment is to slow the disease and improve outcomes. It’s important to keep monitoring and adjust the plan as needed.
Disease Progression Indicators
As GBM advances, knowing signs of change is important. These include more symptoms, cognitive decline, or physical worsening. We teach patients to spot these signs for timely action.
Recognizing these signs helps move to supportive care. We help patients and families understand these changes and adjust care plans.
Transition to Supportive Care
The move to supportive care is a big step in the GBM timeline. Now, the focus is on improving life quality, not just treating the disease. We offer supportive care to manage symptoms, pain, and emotional needs.
Supportive care is personalized for each patient. Our goal is to make patients comfortable and support their families emotionally.
Early Warning Signs and Symptoms of GBM Progression
GBM progression shows up in many ways, affecting the brain, body, and mind. It’s important to spot these signs early. This helps doctors act fast and make treatment plans better.
Neurological Changes to Monitor
As GBM gets worse, patients might notice big changes in their brain. They could feel seizures, weakness, or numbness in certain areas. It’s key to watch these changes and tell doctors right away.
Some common brain symptoms to look out for are:
- Changes in vision or hearing
- Difficulty with speech or understanding language
- Weakness or paralysis in the face, arm, or leg
- Seizures or convulsions
Physical Symptoms Throughout Disease Course
Physical symptoms can really affect a patient’s life. They might feel fatigue, headaches, and nausea. It’s important to manage these symptoms well to keep patients comfortable.
| Symptom | Possible Causes | Management Strategies |
|---|---|---|
| Fatigue | Tumor growth, treatment side effects | Rest, physical therapy, medication |
| Headaches | Increased intracranial pressure | Corticosteroids, pain management |
| Nausea | Treatment side effects, tumor growth | Anti-nausea medication, dietary changes |
Cognitive and Behavioral Changes
Cognitive and behavioral changes can be tough for patients and their families. These might include mood swings, memory loss, and trouble focusing. It’s important to understand these changes to help support patients.
Here are some ways to manage these changes:
- Keeping a symptom journal to track changes
- Engaging in cognitive rehabilitation therapy
- Using memory aids and reminders
When Treatment Stops Working: The Shift to Comfort Care
When glioblastoma multiforme (GBM) treatment stops working, patients and families hit a tough spot. At this point, the focus moves from trying to cure or extend life to comfort care. This care focuses on improving the patient’s quality of life.
Recognizing Treatment Failure
It’s hard to know when GBM treatment is no longer working. The healthcare team closely watches the patient’s condition and does regular checks. Signs that treatment might not be working include getting worse symptoms, tumors growing, and overall health declining.
Healthcare providers work with patients and families to spot these changes. They talk about what it means for their care plan. This teamwork makes sure everyone is on the same page.
The Decision-Making Process
Choosing to stop active treatment and move to comfort care is a tough choice. It’s about weighing the good and bad of more treatment against the patient’s quality of life.
We help patients and families make this choice. We give them info on hospice care and other support services. Places like Casey House offer care that covers physical, emotional, and spiritual needs.
Setting New Goals of Care
When the focus is on comfort care, setting new goals is key. These goals often include managing symptoms, keeping dignity, and making the patient’s time left as comfortable and meaningful as possible.
Our team works with patients and families to create a care plan that fits these goals. We focus on comfort, pain control, and emotional support. This way, patients can live their remaining days with the best possible quality of life.
Brain Cancer Hospice Care: Special Considerations
Brain cancer hospice care has its own set of challenges. It needs a special approach to help patients. We know that caring for those with brain tumors requires a detailed and caring plan.
Unique Challenges of Brain Tumor Hospice
Patients with brain tumors face many complex symptoms. These include seizures, headaches, and changes in thinking. We manage these symptoms carefully to keep patients comfortable and improve their quality of life.
Managing seizures is a big part of brain tumor hospice care. We create a plan with patients and their families to reduce seizure risks. Home care is key to this plan, keeping patients in a place they feel safe and comfortable.
The Interdisciplinary Team Approach
An interdisciplinary team is essential for brain tumor patients. Our team includes doctors, nurses, social workers, and spiritual care providers. They work together to meet the patient’s physical, emotional, and spiritual needs.
This teamwork helps us create a care plan that fits the patient’s needs and wishes. The plan might include managing pain, emotional support, and help with daily tasks. Our aim is to improve the patient’s life and support their loved ones during this time.
Home vs. Inpatient Hospice Options
Patients and their families can choose between home and inpatient hospice care. Home care lets patients stay in a familiar place with loved ones. Inpatient care offers 24/7 support in a dedicated facility.
We help patients and families decide the best care setting for them. Whether at home or in a facility, our goal is to provide caring and complete care that improves the patient’s life.
The Hospice Timeline for GBM Patients
Families dealing with GBM hospice care need to know what’s coming. The hospice timeline helps them prepare for this journey.
Average Duration of Hospice Care
Research shows that GBM patients usually stay in hospice for about a month. This short time makes it critical to make every moment count. Care should be tailored to the patient’s needs.
Every patient’s path is different. The time in hospice can vary a lot. Health, disease progress, and support levels all affect how long a patient stays.
Factors Affecting Length of Hospice Stay
Several things can change how long a GBM patient stays in hospice. These include:
- Age and overall health of the patient
- Rate of disease progression
- Level of family and caregiver support
- Availability of appropriate care settings (home, inpatient, etc.)
Knowing these factors helps families and healthcare teams make better care choices.
| Factor | Impact on Hospice Stay |
|---|---|
| Age | Older patients may have shorter hospice stays due to comorbidities. |
| Disease Progression | Rapid progression may result in shorter hospice stays. |
| Caregiver Support | Strong support can lead to longer hospice stays at home. |
What Families Can Expect Week by Week
Every patient’s journey is different, but there are common changes families see. Here’s a general guide:
- Week 1-2: Patients may feel more tired and have changes in sleep.
- Week 3-4: The disease’s effects on the brain may become clearer.
These changes can be tough for families. Our care team is here to support and guide you through this tough time.
Knowing the hospice timeline helps families better handle this hard time. It lets them focus on giving the best care to their loved ones.
7 Key Stages of the GBM End-of-Life Timeline
The end-of-life timeline for GBM patients has seven critical stages. Healthcare providers and families need to know these stages. It’s key for giving the right care and support during this tough time.
Stage 1: Increased Fatigue and Sleep Changes
GBM’s early sign is more fatigue and sleep pattern changes. Patients get very tired and need more rest. It’s important for caregivers to adjust their support to meet these new needs.
Stage 2: Progressive Neurological Decline
As GBM gets worse, neurological decline is a big sign. Symptoms include weakness, numbness, or paralysis. Caregivers must adapt their care to handle these changing symptoms.
Stage 3: Communication and Swallowing Difficulties
Patients face communication and swallowing problems as GBM advances. Speech therapy and diet changes can help. These steps improve the patient’s life quality.
Stage 4: Mobility and Independence Loss
Loss of mobility and independence is a big stage. Patients need help with daily tasks. Caregivers should support them while keeping their dignity.
Knowing these stages helps healthcare providers and families prepare. Recognizing signs of progression lets caregivers offer better support. This improves the quality of life for GBM patients.
| Stage | Common Symptoms | Care Considerations |
|---|---|---|
| 1 | Increased fatigue, sleep changes | Adjust rest and sleep support |
| 2 | Neurological decline | Adapt care for neurological symptoms |
| 3 | Communication and swallowing difficulties | Speech therapy, dietary adjustments |
| 4 | Loss of mobility and independence | Assistance with daily activities |
“Understanding the progression of GBM and its end-of-life stages is key for compassionate care. It helps patients and their families.”
Knowing the 7 stages of the GBM end-of-life timeline helps us support patients and families. We can ensure they get the care and compassion they need during this tough journey.
Managing Symptoms During Final Stages
As GBM reaches its final stages, managing symptoms is key for comfort. We move from trying to cure to focusing on making life better. It’s tough, but with the right steps, we can help a lot.
Controlling Seizures and Headaches
Seizures and headaches are big issues in advanced GBM. Seizure control is vital and often done with special medicines. We adjust these medicines based on how well they work.
For headaches, we use a mix of medicines and relaxation methods. This helps lessen the pain.
Addressing Swelling and Pressure Symptoms
Swelling and pressure can really hurt. Corticosteroids help shrink swelling around the tumor. This eases some of the pressure.
We watch for side effects and change treatments as needed.
Pain Management Approaches
Pain relief is a big part of care in GBM’s final stages. We use medicines and also try things like meditation and gentle massage. This helps manage pain well.
Comfort Measures for Respiratory Changes
Respiratory changes are common in GBM’s final stages. We offer comfort like oxygen therapy and special positions to help breathing. Opioids might also be used to ease breathing trouble.
By focusing on these areas, we can greatly improve life for GBM patients in their final stages. Good symptom management needs a caring and all-around approach. We’re dedicated to giving the best care possible.
Understanding Sudden Decline in GBM Patients
It’s important to know about sudden decline in GBM patients. Glioblastoma multiforme (GBM) is a tough brain tumor. It can make patients get worse fast. We’ll look at why this happens and how to handle it.
Factors Contributing to Rapid Deterioration
GBM tumors can make patients get worse quickly. This is because they press on brain tissue. GBM’s aggressive nature means patients can see big changes fast.
Where the tumor is in the brain matters a lot. Tumors in key areas can make things worse faster. This is because they affect important brain functions.
Preparing for Unexpected Changes
It’s key for families and caregivers to be ready for sudden changes. Knowing the patient’s condition well is important. Talking openly with doctors helps families get ready for anything.
Learning the signs of getting worse is important. This includes confusion, seizures, or trouble swallowing. Having a plan for emergencies can help. It makes sure the patient gets the right care.
| Signs of Rapid Deterioration | Actions to Take |
|---|---|
| Increased confusion or disorientation | Contact healthcare provider immediately |
| Seizures or convulsions | Administer rescue medication if prescribed; seek emergency help |
| Difficulty swallowing or speaking | Consult with healthcare provider for guidance on managing symptoms |
Emergency Symptom Management
Managing symptoms quickly is key for GBM patients. Doctors teach families how to handle symptoms and when to call for help. Having a plan helps make sure patients get the right care fast.
In short, knowing about sudden decline in GBM patients is vital. Being ready for changes helps give the best care. By knowing the signs and having a plan, families and caregivers can help patients the most.
Conclusion: Supporting Patients and Families Through the GBM Journey
Dealing with Glioblastoma Multiforme (GBM) shows us how important it is to support patients and their families. Programs that offer complete care, like hospice, are key. They help a lot with patient and family support.
We’ve looked at the GBM timeline, from first symptoms to the end stages. It’s clear that full care is essential for managing symptoms and better outcomes. Knowing the GBM journey helps healthcare teams give better support. They can meet the special needs of patients and their families.
Our aim is to offer top-notch healthcare with full support for patients from around the world. By focusing on complete care, we can really help those dealing with GBM.
FAQ
What is the typical survival trajectory for a patient diagnosed with glioblastoma multiforme (GBM)?
Patients with GBM usually live about 12-15 months. But, this time can change a lot. It depends on things like age, health, and how well they respond to treatment.
What are the early warning signs of GBM progression?
Signs of GBM getting worse include seizures, headaches, and weakness. You might also notice changes in thinking and behavior, like confusion and mood shifts.
How long does a patient typically stay in hospice care for GBM?
Patients with GBM usually stay in hospice for about a month. But, this can vary. It depends on how fast the disease gets worse and what the patient needs.
What are the key stages of the GBM end-of-life timeline?
The 7 key stages include getting tired more easily, losing brain function, and having trouble talking and swallowing. You’ll also lose mobility and independence. Each stage needs special care.
How can symptoms be managed during the final stages of GBM?
Managing symptoms in the final stages means controlling seizures and headaches. You also need to address swelling, manage pain, and help with breathing changes.
Why do GBM patients sometimes experience sudden decline?
GBM patients can get worse quickly because of the tumor’s location in the brain. It’s important to be ready for sudden changes and have plans for managing symptoms.
What is the difference between active treatment and comfort care for GBM patients?
Active treatment tries to cure or control the cancer. Comfort care focuses on managing symptoms and improving life quality when treatment doesn’t work anymore.
What are the unique challenges of brain tumor hospice care?
Brain tumor hospice care is special because of the complex symptoms and fast disease progression. It needs a team of experts for full support.
Can GBM patients receive hospice care at home?
Yes, GBM patients can get hospice care at home. Many prefer this. But, inpatient hospice options are also available based on what each patient needs.
How can families prepare for the GBM end-of-life timeline?
Families can prepare by learning about GBM’s typical course and recognizing signs of worsening. Working closely with healthcare providers is key to managing symptoms and getting the right support.
References
Brain Hospice. (n.d.). Brain cancer hospice symptom timeline. Retrieved from https://www.brainhospice.org/brain-cancer-hospice-symptom-timeline
Glioblastoma Support. (n.d.). End-state symptoms of brain tumor patients. Retrieved from https://glioblastomasupport.org/end-of-life-resources/end-state-symptoms-of-brain-tumor-patients