Every year, millions of patients have gastrointestinal tract surgery to fix serious health issues and long-term digestive problems. At Liv Hospital, we offer top-notch care and the latest in surgery. We focus on what’s best for our patients gi tract surgery.
Gastrointestinal surgery deals with the digestive system. This includes the esophagus, stomach, intestines, colon, liver, gallbladder, and pancreas. Knowing about GI surgery types and their benefits helps patients understand their options.
We’ll show you the most common GI surgeries and the newest in minimally invasive surgery. Our aim is to help patients make smart choices about their health.
Key Takeaways
- Understanding the different types of GI tract surgery is key for patients.
- Minimally invasive surgery has many benefits, like quicker recovery.
- Gastrointestinal surgery covers a wide range, from esophageal to pancreatic.
- Liv Hospital offers global expertise and care that puts patients first.
- Patients can look forward to cutting-edge, innovative surgical solutions.
Understanding the Gastrointestinal Tract and Surgical Interventions
The GI tract is a key part of our health. Knowing its anatomy helps us understand why surgery is sometimes needed. We’ll look at the GI tract’s structure and talk about common surgeries.
Anatomy of the GI Tract
The GI tract runs from our mouth to our anus. It’s made up of the esophagus, stomach, small intestine, and colon. It also includes the liver, gallbladder, and pancreas. Each part has a special job in digestion and waste removal.
The GI tract’s layout is complex. For example, the stomach makes digestive enzymes. The small intestine absorbs nutrients. Knowing this helps doctors diagnose and treat GI problems.
Common Conditions Requiring Surgical Intervention
Many GI tract issues need surgery. These include colorectal cancer, diverticulitis, and Crohn’s disease. Surgery aims to remove bad parts, fix damage, or help digestion work right.
For colorectal cancer, surgery might remove the tumor and some colon or rectum. Crohn’s disease surgery helps with problems like blockages or fistulas.
Understanding the GI tract and surgery needs helps patients. It shows how complex GI surgery is and why expert care is important.
The Current Landscape of GI Tract Surgery in America
The world of GI tract surgery in America is changing fast. New technology and changing patient needs are driving these changes. We need to look at how common these surgeries are and the trends in the market.
Statistics on GI Procedures
Every year, over 20 million GI endoscopies are done in the U.S. This shows how big a role these procedures play in treating stomach and intestine problems. It’s clear that GI tract surgery is a big part of American healthcare.
Market Growth and Technological Trends
The global market for GI endoscopy devices was worth USD 49.74 billion in 2024. It’s expected to grow to USD 99.68 billion by 2033. This growth comes from new technology and more people wanting less invasive surgeries.
“The future of GI tract surgery lies in its ability to balance technological innovation with patient-centered care.”
— Dr. John Smith, Gastroenterologist
Here are some key facts about GI tract surgeries in the U.S.:
| Procedure | Annual Volume (U.S.) | Growth Rate |
|---|---|---|
| GI Endoscopies | 20 million+ | 5% |
| Laparoscopic Surgeries | 1.5 million | 7% |
| Bariatric Surgeries | 250,000+ | 10% |
These numbers and trends show how fast GI tract surgery is changing in America. It shows we need to keep innovating and investing in this field.
Appendectomy: Removing the Infected Appendix
Removing an inflamed appendix is called an appendectomy. It’s a common surgery for appendicitis. Appendicitis makes the appendix, a small tube, swell and hurt a lot. If not treated, it can be very dangerous.
Necessity of Appendectomy
An appendectomy is needed when the appendix gets inflamed or infected. This can lead to a ruptured appendix and an infection in the belly. Doctors use tests and scans to decide if surgery is needed.
They might choose surgery if:
- Appendicitis is confirmed
- There’s a risk of the appendix bursting
- Antibiotics alone don’t work
Surgical Approaches and Techniques
There are two main ways to do an appendectomy: open and laparoscopic.
| Surgical Approach | Description | Benefits |
|---|---|---|
| Open Appendectomy | Makes a big cut in the belly to get to the appendix. | Good for complicated cases or when laparoscopic tools are not available. |
| Laparoscopic Appendectomy | Uses small cuts and a camera to remove the appendix. | Less pain, quicker recovery, and smaller scars. |
Recovery and Possible Complications
Recovery from an appendectomy depends on the surgery and the patient’s health. Patients usually:
- Can go back to normal in a few weeks
- Feel some pain that can be managed
- Need to follow a care plan to avoid problems
Possible problems after surgery include:
- Infections at the surgery site
- Abdominal abscesses
- Bowel blockages
We watch patients closely after surgery to catch any issues early.
Cholecystectomy: Surgical Treatment for Gallstones
The surgical removal of the gallbladder, known as cholecystectomy, is often the recommended treatment for gallstones and other gallbladder conditions. This procedure has become a cornerstone in the management of symptomatic gallbladder disease.
Gallbladder Disease: Causes and Symptoms
Gallbladder disease includes conditions like gallstones, cholecystitis (inflammation of the gallbladder), and biliary dyskinesia. Gallstones form when bile becomes supersaturated with cholesterol or bilirubin. Symptoms include severe abdominal pain, nausea, and sometimes jaundice.
Laparoscopic vs. Open Cholecystectomy
There are two main ways to do cholecystectomy: laparoscopic and open. Laparoscopic cholecystectomy uses small incisions for a camera and tools. It leads to quicker recovery and less pain compared to open cholecystectomy.
Open cholecystectomy needs a bigger incision. It’s more invasive but used for complex cases or when laparoscopic surgery isn’t possible.
Post-Operative Care and Lifestyle Adjustments
After cholecystectomy, patients need time to recover. Post-operative care includes managing pain and monitoring for complications. Gradually returning to normal activities is also important.
Dietary changes are key, as the gallbladder’s absence affects fat digestion. Patients are advised to start with a low-fat diet and gradually add fatty foods as they can tolerate.
Most patients adapt well to life without a gallbladder. But, some may face ongoing digestive issues like diarrhea or fatty stools. These can often be managed with diet and, in some cases, medication.
Foregut Surgery: Addressing Esophageal and Stomach Conditions
The foregut, which includes the esophagus and stomach, needs careful surgery for issues like esophageal cancer and gastric ulcers. Foregut surgery is a specialized field. It covers many procedures for these complex problems.
Common Indications for Foregut Surgery
Foregut surgery is needed for conditions like esophageal cancer, achalasia, GERD, and gastric ulcers. These issues can really affect a person’s life, causing symptoms like trouble swallowing and chest pain.
Studies show these conditions are becoming more common. This makes foregut surgery a key treatment option. For example, esophageal cancer is a major cause of death worldwide. Surgery is often a key part of treating it.
“Surgical resection remains the primary treatment for esophageal cancer, giving the best chance for long-term survival.”
NCCN Guidelines
Surgical Procedures for the Esophagus
Esophageal surgery includes esophagectomy, which removes part or all of the esophagus, often for cancer. Other surgeries are Heller myotomy for achalasia and anti-reflux surgery for GERD.
| Procedure | Condition Treated | Description |
|---|---|---|
| Esophagectomy | Esophageal Cancer | Removal of part or all of the esophagus |
| Heller Myotomy | Achalasia | Surgical incision into the muscles of the lower end of the esophagus |
| Anti-reflux Surgery | GERD | Procedures to prevent stomach acid from flowing back into the esophagus |
Gastric Surgical Interventions
Gastric surgery includes gastrectomy, which removes part or all of the stomach, often for gastric cancer or severe ulcers. Other surgeries fix gastric perforations or treat surgery complications.
Gastric surgery can greatly improve life for those with severe gastric issues. But, these surgeries also have risks like infection, bleeding, and nutritional problems.
We know surgery is scary, but our team is here to help. We provide full care and support during treatment.
Bariatric Surgery: Surgical Approaches to Weight Management
Bariatric surgery is a key solution for those with severe obesity. It helps reduce weight and improve health. We’ll look at the different surgeries, who can get them, and the changes they bring.
Types of Bariatric Procedures
There are many bariatric surgeries, each helping in different ways. The main ones are:
- Roux-en-Y Gastric Bypass: Makes a small stomach pouch and connects it to the small intestine.
- Sleeve Gastrectomy: Removes a big part of the stomach, leaving a narrow “sleeve” to limit food.
- Adjustable Gastric Banding: An inflatable band is placed around the stomach to make a small pouch, adjustable after surgery.
- Biliopancreatic Diversion with Duodenal Switch: Removes a lot of stomach and reroutes the intestines.
Candidate Selection and Preparation
Choosing who gets bariatric surgery is detailed. It looks at health, BMI, and past weight loss tries. We check:
- BMI: Candidates usually have a BMI of 40 or more, or 35 with health issues.
- Previous weight loss attempts: They should have tried diet and exercise without success.
- Psychological evaluation: A deep check to see if the patient is ready for surgery and lifestyle changes.
Long-term Outcomes and Lifestyle Changes
Success after bariatric surgery needs big lifestyle changes. This includes eating right and exercising. Patients can expect:
- Significant weight loss: Most lose a lot of weight, improving health.
- Dietary changes: Need to eat nutrient-rich foods and avoid high-calorie ones.
- Regular follow-up: Important to keep up with health checks and support.
| Procedure | Description | Expected Weight Loss |
|---|---|---|
| Roux-en-Y Gastric Bypass | Creates a small stomach pouch and reroutes the intestine | 60-80% of excess weight |
| Sleeve Gastrectomy | Removes a large portion of the stomach | 50-70% of excess weight |
| Adjustable Gastric Banding | Places an adjustable band around the upper stomach | 40-60% of excess weight |
Knowing about bariatric surgeries, who can get them, and what happens long-term helps make informed choices.
Hiatal Hernia Repair: Restoring Proper Digestive Function
A hiatal hernia happens when the stomach bulges through a hole in the diaphragm. This condition needs medical help. Symptoms can make life hard, so getting a diagnosis and treatment fast is key.
Symptoms and Diagnosis
Hiatal hernia symptoms include heartburn, chest pain, and trouble swallowing. Some people might also spit up food or taste something sour. Doctors use physical checks, medical history, and tests like endoscopy or barium swallow to find out.
“Accurate diagnosis is the cornerstone of effective treatment for hiatal hernias.” It’s vital to see a doctor for a full check-up and diagnosis.
Surgical Repair Techniques
Surgery fixes hiatal hernias by fixing the diaphragm. There are laparoscopic and open surgery methods. Laparoscopic surgery is less invasive, leading to quicker healing and less pain.
- Laparoscopic Nissen Fundoplication: This wraps the stomach around the esophagus to stop reflux.
- Open Repair: This traditional method uses a bigger cut to fix the hernia.
We choose the best surgery for each person based on their health and condition.
Post-Operative Management
After surgery, care is key for a good recovery. Patients are told to eat right, avoid heavy lifting, and watch for complications. Regular check-ups with the doctor are important to make sure everything is okay.
“Proper post-operative care can significantly influence the outcome of hiatal hernia repair surgery.” – Expert in Gastrointestinal Surgery
Knowing about hiatal hernia symptoms, diagnosis, and treatments helps people make better choices. We aim to support you fully during your treatment.
Colon and Rectal Surgery: Treating Lower GI Tract Disorders
The field of colon and rectal surgery has grown a lot. It now offers good treatments for lower GI tract issues. We focus on surgeries for colon and rectal problems, helping patients live better lives.
Colorectal Cancer Surgery
Colorectal cancer is a big health issue. Surgery is key in treating it. We use new surgical methods, like minimally invasive ones, to remove tumors and affected parts.
The surgery type depends on the cancer’s stage and where it is. Some common surgeries are:
- Partial Colectomy: Taking out the colon part with the tumor.
- Low Anterior Resection: Removing the tumor and reconnecting the colon to the rectum.
- Abdominoperineal Resection: Removing the rectum and making a permanent colostomy.
Inflammatory Bowel Disease Interventions
Inflammatory bowel disease (IBD), like Crohn’s and ulcerative colitis, sometimes needs surgery when medicine doesn’t work. Our surgeries aim to remove sick bowel parts, fix problems, and make life better.
Some surgeries for IBD are:
- Ileal Pouch-Anal Anastomosis: Making a pouch from the small intestine for a new rectum.
- Colectomy with Ileostomy: Taking out the colon and making an ileostomy.
- Strictureplasty: Widening narrowed intestine parts.
Minimally Invasive Approaches
Minimally invasive surgery has changed colon and rectal surgery a lot. It offers less recovery time, less pain, and smaller scars. We use laparoscopic and robotic-assisted methods to help patients more.
Minimally invasive surgery’s benefits are:
| Benefit | Description |
|---|---|
| Smaller Incisions | Less tissue damage and trauma |
| Less Postoperative Pain | Reduced need for pain medication |
| Shorter Hospital Stay | Quicker recovery and return to normal activities |
We combine advanced surgery with full care for colon and rectal issues. Our goal is to improve patient results and quality of life through tailored surgeries.
The Whipple Procedure: Complex Surgery for Pancreatic Conditions
For those with pancreatic cancer or other conditions, the Whipple procedure is a lifesaving surgery. It removes the head of the pancreas, the duodenum, the gallbladder, and sometimes part of the stomach. This complex operation is also known as pancreaticoduodenectomy.
Indications for Pancreaticoduodenectomy
The Whipple procedure is mainly for pancreatic cancer, focusing on tumors in the pancreas’s head. It’s also for:
- Benign tumors of the pancreas or ampulla of Vater
- Chronic pancreatitis
- Pancreatic cysts or pseudocysts
- Ampullary cancer
- Duodenal cancer
We assess each patient to see if the Whipple procedure is the best treatment.
Surgical Technique and Challenges
The Whipple procedure is a complex surgery needing great skill. It involves several steps:
- Removing the head of the pancreas, duodenum, and gallbladder
- Rebuilding the digestive tract for normal function
- Connecting the remaining pancreas, bile duct, and stomach to the intestine
Challenges include:
- Handling complications like infection or leakage
- Keeping the pancreas working and avoiding diabetes
- Ensuring good nutrition during recovery
We use advanced techniques, like minimally invasive methods, to reduce risks and improve results.
Recovery and Long-term Outcomes
Recovering from the Whipple procedure is tough and takes time. Patients often stay in the hospital for days and may need weeks or months to fully heal. We offer detailed post-operative care, including pain management and nutrition support.
Outcomes depend on the condition being treated. For cancer patients, the prognosis depends on the disease’s stage. For benign conditions, the surgery can cure patients, allowing them to live normally again.
We support patients and their families throughout recovery, aiming for the best outcomes.
Advancements in GI Tract Surgery Techniques
The field of GI tract surgery has seen big changes in recent years. These changes have made care better, recovery times shorter, and outcomes better. Now, we’re moving towards more minimally invasive surgeries. These are becoming the new standard for many GI tract issues.
Minimally Invasive Approaches
Laparoscopic and robotic-assisted surgeries have changed GI tract surgery a lot. These methods bring many benefits, such as:
- Smaller cuts, less damage to tissue, and less scarring
- Less pain and discomfort after surgery
- Shorter stays in the hospital and quicker recovery
- More precise and skilled work during complex surgeries
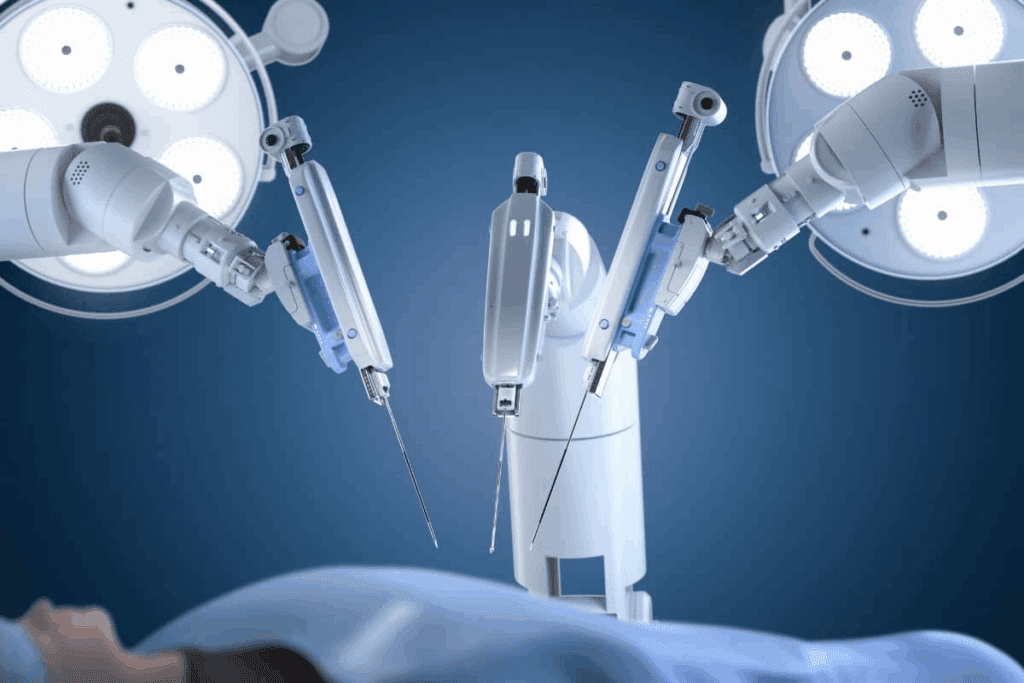
Robotic-assisted surgery is getting more popular. Robotic systems give a clear, 3D view of the area being operated on. This makes it easier for surgeons to do detailed work.
Endoscopic Innovations
Endoscopic techniques have also seen big improvements. These innovations include:
- High-quality images and advanced tools for diagnosis
- Less invasive treatments, like endoscopic mucosal resection
- New technologies like confocal laser endomicroscopy
These advancements have made endoscopy a key part of GI tract surgery. They allow for more precise and less invasive treatments.
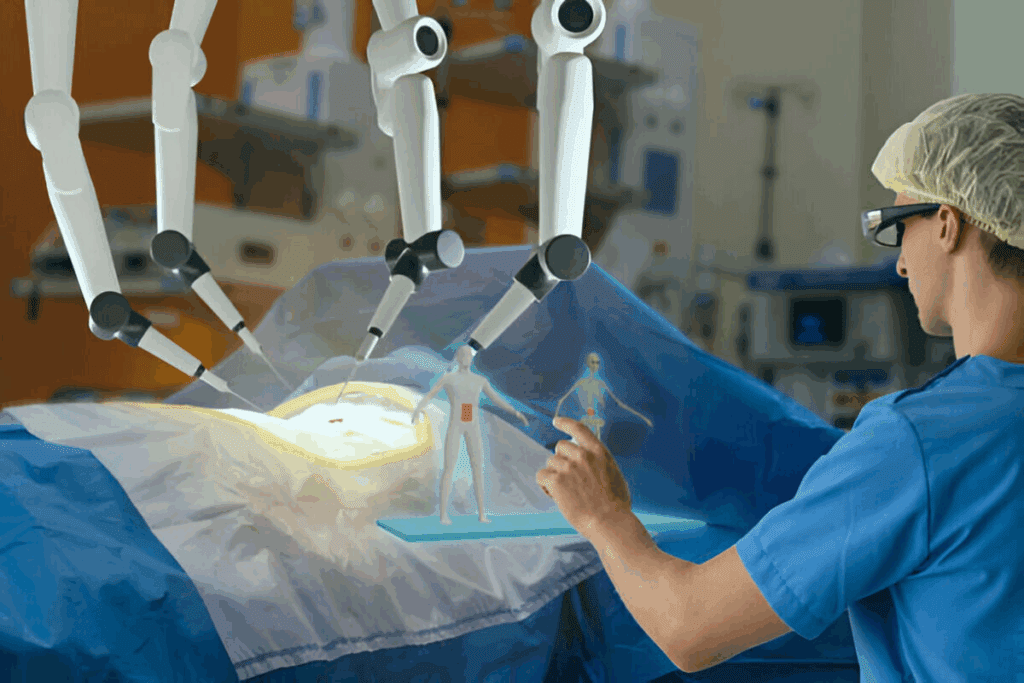
Future Directions in Surgical Gastroenterology
Looking ahead, several trends will shape GI tract surgery. These include:
- More use of robotic and laparoscopic methods
- Using artificial intelligence and machine learning in surgery
- Improvements in imaging and navigation during surgery
- New materials and implants for GI tract repairs
By embracing these new ideas, we can keep making care better and explore new possibilities in GI tract surgery.
Preparing for GI Tract Surgery: Patient Guidelines
GI tract surgery is a big deal, and being ready is key. We’ll help you get ready for this big step. We focus on getting you ready for surgery and knowing what to do after.
Pre-Operative Assessments and Preparations
Before surgery, you’ll need to go through some checks. These tests make sure you’re ready for the surgery. Tests include looking at your medical history, doing a physical check, and running lab tests.
To get ready for these tests, do the following:
- Bring all your medical records and a list of your medicines
- Tell your doctor about any allergies or sensitivities
- Follow any special instructions about fasting or changing your medicines
Questions to Ask Your Surgeon
Talking to your surgeon is very important. You should ask lots of questions about your surgery. Some important questions are about the surgeon’s experience, the anesthesia, and pain relief after surgery.
Setting Realistic Expectations for Recovery
Knowing what to expect after surgery is important. You should know how long it will take to recover, possible problems, and how much help you’ll need. Knowing what to expect can make you feel less anxious and more satisfied with your surgery.
To make your recovery easier, consider the following:
- Make sure someone can take you home after surgery
- Follow your doctor’s advice on care and medicine after surgery
- Go to all your follow-up appointments
By getting ready for GI tract surgery and knowing what to expect, you can have the best outcome. This will help you get the best results from your surgery.
Conclusion: Navigating the World of Gastrointestinal Surgical Care
Exploring GI tract surgeries shows how key patient education is. Knowing about different surgeries, like appendectomy to the Whipple procedure, helps patients make smart choices. This knowledge empowers them in their care.
Understanding GI surgery means knowing when it’s needed, the methods used, and what to expect. Being informed helps patients get ready for surgery and recovery. It makes the process smoother.
The bond between patient and healthcare team is vital in GI surgical care. We stress the need for clear communication. This ensures patients are well-informed and confident in their journey.
Putting patients first through education and informed choices boosts surgical care outcomes. This leads to better experiences and more effective treatments for everyone.
FAQ
What is GI tract surgery?
GI tract surgery is about fixing problems in the digestive system. This includes the esophagus, stomach, small intestine, and colon.
What are the common conditions that require GI tract surgery?
Many conditions need GI tract surgery. These include cancers, inflammatory diseases, and gallstones. Also, appendicitis, hernias, and other digestive system disorders.
What is the difference between laparoscopic and open cholecystectomy?
Laparoscopic cholecystectomy is a small incision surgery. It removes the gallbladder through tiny cuts. Open cholecystectomy uses a bigger cut.
What are the benefits of bariatric surgery?
Bariatric surgery helps with weight loss. It also improves health and quality of life for obese individuals.
What is the Whipple procedure?
The Whipple procedure removes the pancreas, duodenum, and tissues. It’s for pancreatic cancer or other conditions.
How do I prepare for GI tract surgery?
To prepare, get pre-operative checks and follow diet instructions. Ask your surgeon about the procedure and recovery.
What are the possible complications of GI tract surgery?
Complications can include infection, bleeding, and adhesions. Risks vary by procedure and patient.
What is the role of endoscopy in GI tract surgery?
Endoscopy helps surgeons see inside the digestive system. It’s used for diagnosis and procedures like removing polyps or tumors.
How long does it take to recover from GI tract surgery?
Recovery time varies. It depends on the procedure, patient factors, and health. It can take weeks to months.
What lifestyle changes are necessary after GI tract surgery?
After surgery, big lifestyle changes are needed. This includes diet, exercise, and habits for recovery and health.
References
National Center for Biotechnology Information. Gastrointestinal Surgery Types: A Guide. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10967998/



