Last Updated on October 21, 2025 by mcelik
Hemophilia is a genetic disorder that makes it hard for blood to clot. This leads to long-lasting bleeding. Recent gene therapy by uniQure offers hope for treating it.
Knowing the genetic roots of hemophilia prevention is key. It’s a complex issue, but research has made big strides. It has found the causes and possible treatments.
So, how can you prevent hemophilia? It’s a genetic issue, but knowing your family history helps. Genetic counseling is also crucial, especially for hemophilia in females.
Key Takeaways
- Understanding the genetic basis of hemophilia is crucial for prevention.
- Gene therapy has shown promise in treating hemophilia.
- Family history and genetic counseling can help manage the risk.
- Awareness of hemophilia prevention strategies is essential.
- Research continues to advance in identifying causes and treatments.
Understanding Hemophilia: A Blood Clotting Disorder
To understand hemophilia, we need to look at its types, how blood clots, and how these work together in females.
What is Hemophilia?
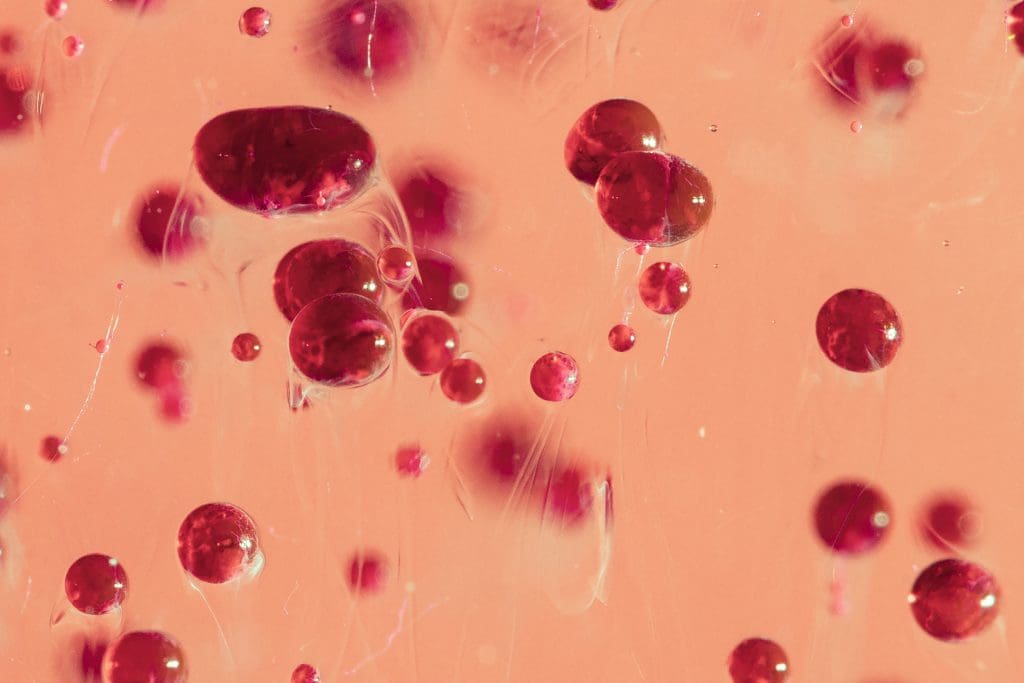
Hemophilia is a genetic disorder that makes it hard for the body to clot blood. This leads to long-lasting bleeding. It’s mainly caused by a lack of clotting factor VIII (Hemophilia A) or clotting factor IX (Hemophilia B).
Key aspects of hemophilia include its genetic basis and the impact on individuals, particularly females who are carriers or affected.
Types of Hemophilia
There are two main types of hemophilia: Hemophilia A and Hemophilia B. Hemophilia A is more common and is caused by a deficiency in factor VIII. Hemophilia B results from a deficiency in factor IX.
The severity of hemophilia can vary. Some people have mild symptoms, while others face severe bleeding episodes.
How Blood Clotting Works
Blood clotting is a complex process involving many clotting factors. In people with hemophilia, a lack of a specific clotting factor disrupts this process. This leads to bleeding problems.
Understanding the clotting mechanism is crucial for appreciating the challenges faced by individuals with hemophilia and the importance of appropriate treatment.
Gene therapy aims to fix the clotting factor deficiency. It introduces healthy copies of the affected gene into the individual’s cells. This could be a long-term solution for managing hemophilia.
Genetic Basis of Hemophilia
Hemophilia is a bleeding disorder caused by specific gene mutations. It is mainly inherited in an X-linked recessive pattern. This means the genes for it are on the X chromosome.
X-Linked Inheritance Pattern
Males are more likely to have hemophilia because they have only one X chromosome. Females can carry the mutated gene but are less likely to have the disorder. They can, however, pass it to their children. Knowing this is key for genetic testing for hemophilia in women who might be carriers.
Female carriers have a 50% chance of passing the mutated gene to each son, who may be affected, and to each daughter, who will likely become carriers. Genetic counseling is recommended for families with hemophilia history to understand risks and implications.
Role of Factor VIII and Factor IX Genes
Hemophilia A and B are caused by mutations in the genes for Factor VIII and Factor IX. These clotting factors are crucial for blood coagulation. Mutations lead to deficient or dysfunctional clotting factors, causing bleeding.
| Type of Hemophilia | Affected Gene | Clotting Factor |
| Hemophilia A | F8 | Factor VIII |
| Hemophilia B | F9 | Factor IX |
Spontaneous Mutations
Not all hemophilia cases are inherited; some come from spontaneous mutations in Factor VIII or IX genes. These mutations can happen in people without a family history of hemophilia, marking the first occurrence in a family.
Genetic testing can find carriers and affected individuals. This information is crucial for family planning and managing the disorder. For women with von willebrand disease or other bleeding disorders, knowing the genetic basis helps in their care and treatment.
Can Hemophilia Be Completely Prevented?
Hemophilia is mostly inherited, but can it be completely stopped? It’s a condition where blood doesn’t clot right, leading to long bleeding. It’s passed down through families because of genetic changes.
Inherited Nature of the Disorder
Hemophilia comes from genes that code for clotting factors VIII or IX. These genes are on the X chromosome. This is why it’s more common in males, who have only one X chromosome. Females can be carriers but rarely have two affected X chromosomes.
The inherited nature of hemophilia makes it hard to prevent. Families with a history of it are more likely to pass it on. Knowing the genetics helps families plan better.
Limitations of Prevention Strategies
There are limited strategies to prevent hemophilia. Genetic counseling helps families understand risks and plan. But, once a child is born with the mutation, there’s no way to stop it with today’s tech.
Gene therapy might offer a future solution. It tries to fix the genetic problem causing hemophilia. But, it’s still in the early stages and faces many challenges.
Realistic Expectations for Prevention
With today’s science, completely preventing hemophilia is not possible for most families. But, families at risk can learn their chances through genetic counseling. This helps them plan their families better.
Even though preventing hemophilia is complex, research and genetic medicine are getting better. Could hemophilia be prevented? Yes, with gene therapy and counseling, it might become more possible.
Genetic Counseling for Hemophilia Prevention
Genetic counseling helps families understand their risk of hemophilia. It’s crucial for those with a family history of the disorder.
When to Seek Genetic Counseling
If you have a family history of hemophilia, you should get genetic counseling. This is especially true for women who might pass the mutated gene to their sons.
Key indicators for seeking genetic counseling include:
- A family history of hemophilia or other bleeding disorders
- A previous child diagnosed with hemophilia
- Known carrier status for hemophilia
What to Expect During Counseling
A healthcare professional will look at your family history during counseling. They’ll talk about the risks of hemophilia and how it’s passed down.
Counselors will provide information on:
- The genetic basis of hemophilia
- Available testing options for carrier status
- Family planning choices, including prenatal testing and preimplantation genetic diagnosis
Making Informed Family Planning Decisions
Genetic counseling helps families make smart choices about their reproductive health. It lets them understand risks and options, guiding them in planning their family.
Options may include:
- Prenatal testing to determine if the fetus is affected
- Preimplantation genetic diagnosis (PGD) during IVF
- Considering alternative reproductive options
Genetic counseling is key in managing and preventing hemophilia. It offers detailed information and support.
Prenatal Testing and Diagnosis
It’s important for expectant parents to know about prenatal testing for hemophilia. This testing can find out if a fetus has hemophilia. This helps parents make choices about their pregnancy.
Chorionic Villus Sampling (CVS)
Chorionic Villus Sampling (CVS) is a test that takes cells from the placenta. It can spot genetic issues like hemophilia early, around 10 to 12 weeks. But, CVS might slightly increase the risk of losing the baby.
Amniocentesis
Amniocentesis is a test that takes fluid from the amniotic sac. It’s done between 15 and 20 weeks. This test can find hemophilia by looking at the DNA in the fluid.
Non-Invasive Prenatal Testing Options
Non-invasive prenatal testing (NIPT) looks at DNA in the mom’s blood. It’s not a sure way to find hemophilia but can show a higher risk. For families with hemophilia history, NIPT might be the first step. Then, CVS or amniocentesis might follow if needed.
Prenatal testing for hemophilia gives families important info. It helps them get ready for a child with a bleeding disorder. It also helps plan for the baby’s birth and care after it’s born, which can lower risks.
Preimplantation Genetic Diagnosis (PGD)
Preimplantation Genetic Diagnosis (PGD) is a new technique. It’s used with IVF to stop hemophilia from being passed on. This method checks embryos for genetic problems before they’re put in the uterus. It’s a big step forward in managing hereditary conditions like hemophilia.
Process with IVF
PGD works with In Vitro Fertilization (IVF) to pick healthy embryos. First, eggs are stimulated to grow, then retrieved and fertilized in a lab. The embryos grow for days, and then a few cells are taken for genetic testing.
This testing finds out if an embryo has the hemophilia gene. Using PGD with IVF means choosing embryos without hemophilia. It also boosts the chances of a successful pregnancy by picking the best embryos.
Success Rates and Considerations
PGD’s success depends on many things. These include the quality of the embryos, how accurate the genetic testing is, and the clinic’s skill. PGD is very good at finding genetic problems. But, it’s not a 100% guarantee against all genetic issues or a successful pregnancy.
- Success rates differ between clinics and depend on age and embryo quality.
- The process needs careful planning and teamwork between fertility experts and geneticists.
- It’s important for couples to have emotional and psychological support during this time.
Couples thinking about PGD should talk to their healthcare providers. This helps them make informed choices.
Women Hemophilia: Unique Challenges and Considerations
Women with hemophilia face many challenges, from health issues to social stigma. They need a lot of support. Hemophilia is often seen as a male disease, but women can be affected too.
Female Carriers vs. Women with Hemophilia
It’s important to know the difference between female carriers and women with hemophilia. Female carriers have one normal and one affected X chromosome. They usually don’t show symptoms but can pass the gene to their kids. But, some carriers might have mild symptoms.
Women with hemophilia are less common. They might have two copies of the hemophilia gene or a special X-chromosome pattern.
Symptoms Specific to Women
Women with hemophilia or carriers have symptoms that are different from men. These include:
- Menorrhagia or heavy menstrual bleeding
- Increased risk of bleeding after childbirth
- Bleeding after surgical procedures
- Easy bruising
These symptoms can really affect their life. They need special care.
Reproductive Health Concerns
Reproductive health is a big worry for women with hemophilia or carriers. Menorrhagia can cause iron deficiency anemia. There’s also a higher risk of bleeding during and after pregnancy.
Working closely with doctors is key. They help plan safe deliveries and care after birth.
Impact on Quality of Life
Hemophilia affects women’s lives in many ways. It can impact their social life, mood, and overall happiness. Stigma and wrong ideas about hemophilia can make them feel alone.
Support from family, doctors, and groups is very important. It helps deal with these challenges.
Understanding women with hemophilia’s challenges helps doctors provide better care. This improves their life quality.
Diagnosing Hemophilia in Females
Females with hemophilia often go undiagnosed because their symptoms are different. Hemophilia is a genetic disorder that affects blood clotting. It’s usually seen in males, but females can be carriers or affected, making diagnosis tricky.
Why Women Are Often Underdiagnosed
Women are often not diagnosed or are misdiagnosed with hemophilia. This is because healthcare providers are not always aware. Symptoms in females can be different from those in males, making it harder to diagnose. For example, females might have mild bleeding or bruising, which can be mistaken for other conditions.
Testing Protocols for Women
To accurately diagnose, specific tests are needed. These include:
- Clotting factor assays to measure the level of factor VIII or IX.
- Genetic testing to identify mutations in the F8 or F9 genes.
- Comprehensive bleeding history to assess the severity and frequency of bleeding episodes.
Interpreting Test Results
Understanding test results for females with hemophilia is complex. A key point is that females can have varying clotting factor levels due to X-chromosome inactivation. This affects how clotting factor assays are interpreted.
| Test Type | Purpose | Significance in Females |
| Clotting Factor Assays | Measure factor VIII or IX levels | Helps diagnose hemophilia A or B; levels can be affected by X-chromosome inactivation |
| Genetic Testing | Identify F8 or F9 gene mutations | Crucial for determining carrier status and potential hemophilia severity |
| Bleeding History | Assess bleeding episode frequency and severity | Essential for understanding the clinical impact of hemophilia |
Advocating for Proper Diagnosis
Advocacy is key for proper diagnosis of females with hemophilia. Raising awareness among healthcare providers and the general public is vital. Support from hemophilia organizations and resources helps ensure access to the right care.
For more information, visit reputable organizations dedicated to hemophilia care and research.
Managing Hemophilia During Pregnancy
Women with hemophilia need careful planning and monitoring during pregnancy. This is to keep them and their baby safe. Managing hemophilia during pregnancy involves several important steps.
Preconception Planning
Planning before getting pregnant is key for women with hemophilia. They need to understand the risk of passing the disorder to their child. Genetic counseling helps a lot, giving insights into the chance of passing hemophilia.
- Understanding the genetic basis of hemophilia
- Assessing the risk of transmission to offspring
- Discussing reproductive options, including preimplantation genetic diagnosis (PGD)
Monitoring Throughout Pregnancy
Women with hemophilia need close monitoring during pregnancy. They should see a hematologist and obstetrician regularly. This helps keep an eye on their clotting factor levels and the baby’s health.
- Regular blood tests to monitor clotting factor levels
- Ultrasound examinations to assess fetal development
- Adjusting treatment plans as necessary to maintain the mother’s health
Delivery Considerations
Choosing the right delivery method is important for women with hemophilia. The decision between vaginal delivery and cesarean section depends on several factors. These include the mother’s clotting factor levels and any complications.
Postpartum Care
Postpartum care is crucial to prevent bleeding. Women with hemophilia might need factor replacement therapy to manage bleeding risks after giving birth.
- Monitoring for postpartum hemorrhage
- Administering factor replacement therapy as needed
- Providing pain management options that are safe for women with hemophilia
Preventing Bleeding Episodes in Diagnosed Patients
Stopping bleeding episodes is a main goal for those with hemophilia. This can be done through different treatments. It’s not just about treating bleeding, but also preventing it.
Prophylactic Treatment Approaches
Prophylactic treatment is key in managing hemophilia. It involves regular infusions of clotting factors. This keeps the blood with enough of the missing factor, stopping bleeding before it starts.
Benefits of Prophylaxis: It greatly cuts down on bleeding, protects joints, and boosts life quality for patients.
Factor Replacement Therapy
Factor replacement therapy is a common method. It uses clotting factor concentrates to replace the missing factor in the blood.
| Therapy Type | Description | Benefits |
| Recombinant Factor Replacement | Produced through genetic engineering, these factors are not derived from human plasma. | Lower risk of transmitting infectious agents, consistent supply. |
| Plasma-Derived Factor Replacement | Derived from human plasma, these factors are purified to reduce the risk of infections. | Long history of use, effective in managing bleeding episodes. |
Non-Factor Replacement Options
New treatments are coming up that don’t use factor replacement. They work in other ways to help stop bleeding.
Examples include: Emicizumab, a special antibody that acts like factor VIII, and gene therapy to fix the genetic problem causing hemophilia.
Treatment Adherence Strategies
Sticking to treatment plans is vital for prophylactic therapy to work. Ways to help include educating patients, making treatment easier, and offering support.
By using these treatments, patients with hemophilia can lower their risk of bleeding. This improves their life quality a lot.
Lifestyle Modifications to Prevent Complications
Making certain lifestyle changes can greatly lower the risk of complications from hemophilia. By making smart choices, people can manage their condition better and live a better life.
Physical Activity Guidelines
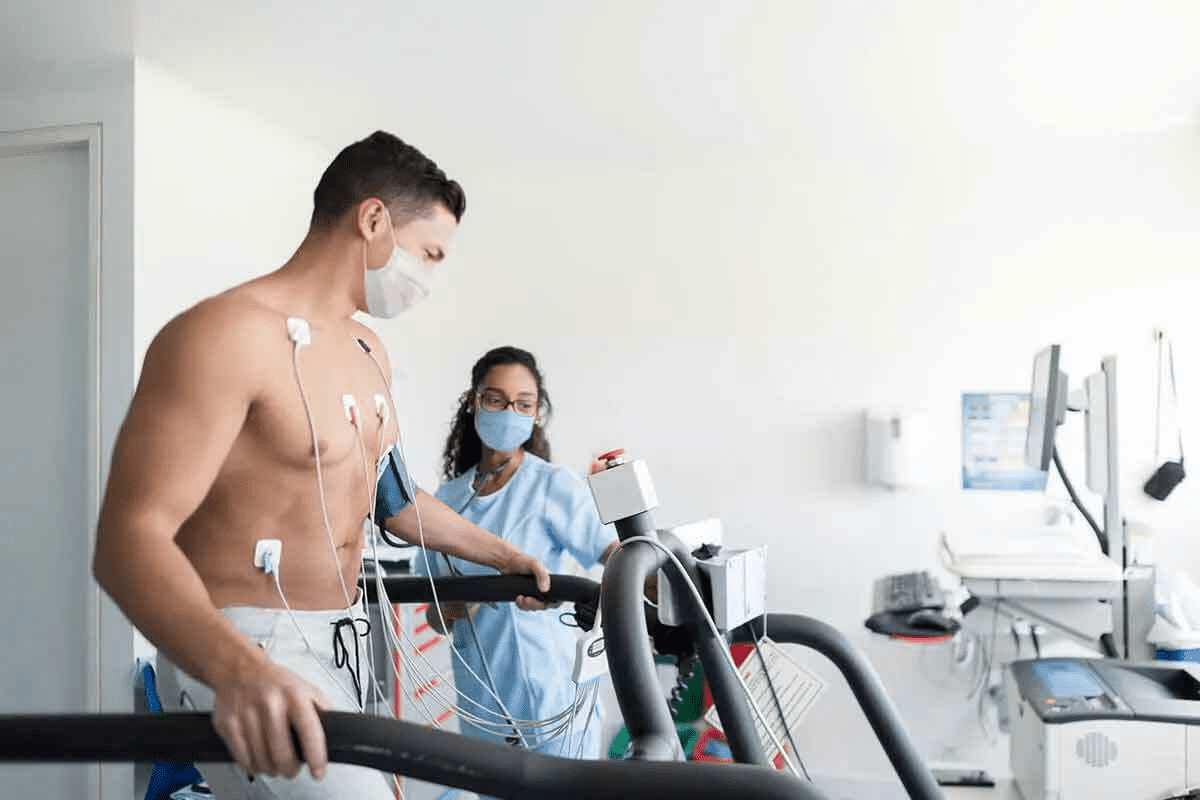
Regular exercise is key for those with hemophilia. It keeps joints healthy and improves physical function. But, it’s important to pick activities that don’t increase the risk of injury.
- Recommended Activities: Swimming, cycling, and gentle stretching are good choices.
- Activities to Avoid: High-impact sports like football, hockey, or wrestling are too risky.
Dietary Considerations
Eating a balanced diet is essential for health. Some nutrients help manage hemophilia.
- Nutritional Needs: Make sure to get enough vitamins and minerals, especially for bone health like calcium and vitamin D.
- Hydration: Drinking enough water is also key for health and managing the condition.
Avoiding Medication Interactions
People with hemophilia must be careful with their medications to avoid bad interactions.
| Medication Type | Potential Interaction | Precaution |
| Blood Thinners | Increased risk of bleeding | Monitor clotting factor levels closely |
| NSAIDs | Increased risk of bleeding | Avoid or use with caution |
| Certain Supplements | Potential to affect clotting | Consult healthcare provider before use |
Home Safety Measures
Keeping your home safe is vital to prevent accidents and injuries that could cause bleeding.
- Remove Tripping Hazards: Keep floors clear and well-lit.
- Use Protective Gear: Use padding on sharp corners or edges.
- Safe Storage: Store sharp objects and medications safely.
By following these lifestyle changes, people with hemophilia can lower their risk of complications and improve their health.
Emerging Treatments and Prevention Strategies
Hemophilia treatment is on the verge of a big change. New gene therapy and clotting factor products are coming. These aim to cut down on bleeding and reduce the need for frequent infusions.
Gene Therapy Advances
Gene therapy is a big hope for hemophilia treatment. It tries to fix the gene that causes the condition. This way, the body can make the clotting factor it needs.
Early trials show promise, with some patients making clotting factor VIII or IX for a long time. This could mean fewer bleeding episodes and less need for infusions. But, we need to watch how it works over time.
Novel Clotting Factor Products
New clotting factor products are also being made. They include clotting factors that last longer, so you don’t need to get them as often. There are also non-factor therapies that help stop bleeding in different ways.
These new products could make treatment easier and better for people with hemophilia.
Research Specifically Addressing Women’s Needs
Most hemophilia research has focused on men. But, women with hemophilia or who carry the gene need attention too. They face unique challenges.
Research is now looking into how to help women. It aims to understand their symptoms, how to diagnose them, and what treatments they need. This way, women can get the care and support they deserve.
Extended Half-Life Products
Extended half-life clotting factor products last longer in the body. This means you don’t need to get them as often. It could make managing hemophilia easier and less of a hassle.
These products could make treatment more manageable. This could lead to better adherence and a better quality of life for those with hemophilia.
Building a Support Network
A strong support network is key for those with hemophilia. It’s not just about medical care. It’s about working together with healthcare teams, family, and community resources.
Healthcare Team Coordination
Working with a healthcare team is crucial for hemophilia management. This team includes hematologists, nurses, and physical therapists. Good communication among them ensures comprehensive care.
A coordinated team can help in many ways:
- Creating personalized treatment plans
- Teaching about managing hemophilia
- Support during bleeding episodes
Family Education and Involvement
Family members are vital in supporting those with hemophilia. Teaching them about the condition and how to handle emergencies is important. It greatly improves the patient’s life.
Family involvement can include:
- Learning about factor replacement therapy
- Understanding how to administer treatments
- Recognizing signs of bleeding episodes
Community Resources and Support Groups
Community resources and support groups add extra support for those with hemophilia and their families. They offer emotional support, practical advice, and connections to others facing similar challenges.
Benefits of these resources include:
| Resource | Description | Benefit |
| Support Groups | Meetings or online forums for individuals and families affected by hemophilia | Emotional support and shared experiences |
| Educational Programs | Workshops and seminars on hemophilia management and treatment | Knowledge and skills for managing hemophilia |
| Advocacy Services | Organizations that advocate for the rights and needs of individuals with hemophilia | Access to care and resources |
Creating a support network involves healthcare coordination, family education, and community resources. With a strong support system, individuals with hemophilia can live more fulfilling lives.
Advocacy and Awareness for Women with Bleeding Disorders
Women with bleeding disorders face unique challenges. They often get diagnosed and treated later than men. This is because there’s still a lot to learn and do to help them.
Addressing Gender Disparities in Diagnosis
Women are often not diagnosed correctly because of a lack of knowledge. Healthcare providers need to be more aware of how bleeding disorders show up in women.
- Educating healthcare professionals about the unique symptoms and diagnostic criteria for women with bleeding disorders.
- Promoting the use of appropriate diagnostic tools and tests for female patients.
- Encouraging a multidisciplinary approach to care that includes hematologists, obstetricians, and other specialists.
Educational Initiatives
Educational efforts are key to spreading the word about bleeding disorders. These efforts should reach both the public and healthcare workers. This way, everyone can understand the condition better.
Public awareness campaigns can help reduce stigma and promote understanding, while professional education can improve diagnosis and treatment.
Policy Changes Needed
| Policy Area | Current Status | Proposed Change |
| Insurance Coverage | Limited coverage for certain treatments | Comprehensive coverage for all necessary treatments |
| Research Funding | Insufficient funding for research on women’s bleeding disorders | Increased funding for targeted research studies |
Participating in Research Studies
Joining research studies is important for improving care for women with bleeding disorders. These studies help find the best ways to treat and manage the condition.
By supporting research and advocacy, we can improve outcomes for women with bleeding disorders.
Conclusion
Hemophilia prevention and treatment have made big steps forward. Yet, women with hemophilia still face special challenges. Knowing the genetic roots of hemophilia and using genetic counseling and prenatal tests can help families make better choices.
Women with hemophilia need the right diagnosis and care. New treatments are giving them hope. By using preventive treatments and making lifestyle changes, their quality of life can improve a lot.
Raising awareness about women with hemophilia is key. We need to fight for fair diagnosis and treatment for them. As research gets better, we must focus on what women with hemophilia need. They should get the care and support they deserve.
Education, community resources, and support groups can help women with hemophilia. They can face their condition with confidence. By supporting women with hemophilia, we make a better world for everyone with this condition.
FAQ
What is hemophilia and how does it affect women?
Hemophilia is a genetic disorder that makes it hard for the body to form blood clots. This is important for stopping bleeding. While it’s more common in men, women can carry the gene or have it themselves. They face unique challenges and considerations.
Can hemophilia be prevented?
Hemophilia is mostly inherited. While there are prevention strategies like genetic counseling and prenatal testing, we can’t prevent it completely yet.
What is the role of genetic counseling in hemophilia prevention?
Genetic counseling helps families understand the risk of passing on hemophilia. It guides them in making choices about family planning. This includes using prenatal testing and preimplantation genetic diagnosis.
How does preimplantation genetic diagnosis (PGD) work in preventing hemophilia?
PGD is used during IVF to screen embryos for genetic disorders like hemophilia. It helps reduce the chance of having a child with the condition.
What are the challenges faced by women with hemophilia?
Women with hemophilia or who carry the gene face special challenges. These include being underdiagnosed, reproductive health issues, and how the condition affects their life quality. They need specialized care and support.
How is hemophilia diagnosed in females?
Diagnosing hemophilia in females is hard because of its X-linked inheritance. Testing, like clotting factor level assessments and genetic testing, is key for accurate diagnosis.
What are the treatment approaches for preventing bleeding episodes in hemophilia patients?
Treatments include regular factor replacement therapy and on-demand treatment for acute bleeds. There are also non-factor replacement therapies. The goal is to prevent bleeding and keep joints healthy.
How can lifestyle modifications help prevent complications in individuals with hemophilia?
Making lifestyle changes, like staying active, avoiding certain meds, and making your home safe, can lower bleeding risks. It helps prevent complications from hemophilia.
What emerging treatments are being developed for hemophilia?
New treatments include gene therapy and clotting factor products with longer half-lives. These innovative therapies aim to improve treatment results and possibly cure hemophilia.
Why is building a support network important for individuals with hemophilia?
A support network, including a healthcare team, family education, and community resources, is crucial. It helps manage hemophilia well, improves life quality, and meets the unique needs of those affected.
How can advocacy and awareness help women with bleeding disorders?
Advocacy and awareness are key for addressing gender disparities in diagnosis. They promote education and drive policy changes to support women with bleeding disorders like hemophilia.