Last Updated on October 21, 2025 by mcelik
Hemophilia affects thousands of people worldwide, causing significant concerns regarding blood donation. Individuals with hemophilia are restricted from donating due to their condition’s impact on blood clotting.
Understanding the basics of hemophilia and its implications on blood donation is crucial. Hemophilia is a genetic disorder that impairs the body’s ability to make blood clots. This is a process needed to stop bleeding.

Key Takeaways
- Hemophiliacs are restricted from donating blood due to their condition affecting blood clotting.
- Blood infusion is a critical process for treating hemophilia.
- Understanding blood donation restrictions is essential for individuals with hemophilia.
- Hemophilia A carriers may have different guidelines for blood donation.
- Von Willebrand disease is another condition that affects blood clotting.
Understanding Hemophilia and Blood Disorders
Hemophilia comes from genetics and affects blood clotting. It’s a disorder that makes it hard for the body to stop bleeding. This is because it can’t make blood clots.
What is Hemophilia?
Hemophilia means you can’t stop bleeding right away. It’s often passed down through families and is more common in males. How bad it is can vary a lot from person to person.
Types of Hemophilia: A, B, and C
There are three main types of hemophilia: A, B, and C. Hemophilia A is the most common and is caused by a lack of factor VIII. Hemophilia B, also known as Christmas disease, is caused by a lack of factor IX. Hemophilia C is a milder form caused by a lack of factor XI.
| Type | Factor Deficiency | Severity |
| Hemophilia A | Factor VIII | Variable |
| Hemophilia B | Factor IX | Variable |
| Hemophilia C | Factor XI | Mild |
Symptoms and Diagnosis
The symptoms of hemophilia can be mild or severe. They include bleeding a lot after injuries, bleeding into joints or muscles, and easy bruising. Doctors use blood tests to find out if someone has hemophilia.
Getting diagnosed early and getting the right treatment can really help people with hemophilia live better lives.
Von Willebrand Disease: A Related Blood Disorder
Hemophilia is a well-known bleeding disorder. But, von Willebrand disease is also a significant condition that affects blood clotting. It is named after a Finnish doctor who first described it. It is the most common inherited bleeding disorder.
Differences Between Hemophilia and Von Willebrand Disease
Hemophilia and von Willebrand disease are both bleeding disorders. But, they have different causes and symptoms. Hemophilia is caused by a lack of factor VIII or IX. Von Willebrand disease is caused by a lack or dysfunction of von Willebrand factor (VWF).
The main differences are:
- Clotting Factor Involved: Hemophilia involves factors VIII or IX, while von Willebrand disease involves VWF.
- Symptoms: Both conditions lead to bleeding. But, von Willebrand disease often has more mucocutaneous bleeding (e.g., nosebleeds, easy bruising).
- Inheritance Pattern: Both are inherited. But, von Willebrand disease can be autosomal dominant. Hemophilia is X-linked.
Von Willebrand Inheritance Patterns
Von Willebrand disease is usually inherited in an autosomal dominant pattern. This means a single copy of the mutated gene in each cell is enough to cause the condition. This pattern is different from hemophilia, which is X-linked recessive and mainly affects males.
The inheritance pattern of von Willebrand disease means that:
- A person with the condition has a 50% chance of passing the mutated gene to each child.
- Both males and females are equally likely to be affected.
Severity Levels and Symptoms
The severity of von Willebrand disease can vary a lot among affected individuals. Symptoms can range from mild to severe. They include:
- Easy bruising
- Nosebleeds
- Heavy menstrual bleeding in women
- Prolonged bleeding after surgery or injury
Understanding the severity and specific symptoms of von Willebrand disease is key to managing it effectively.
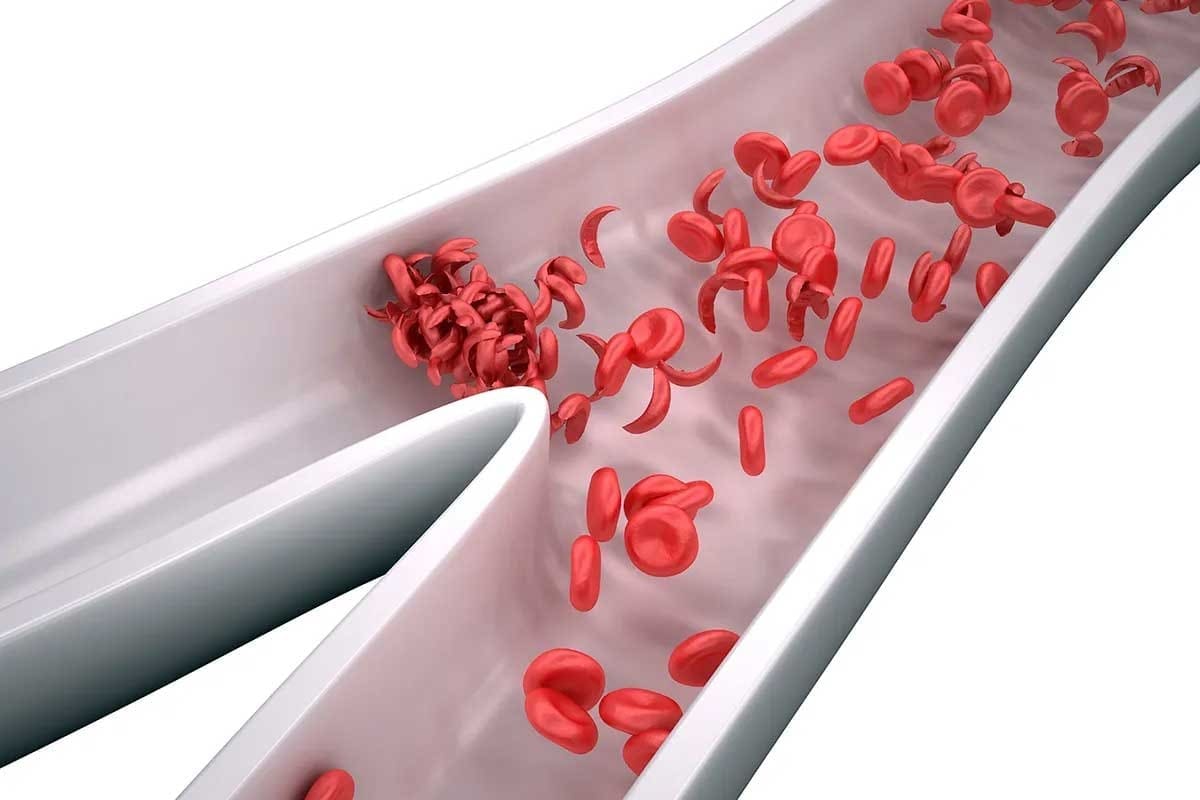
The Science Behind Blood Clotting
It’s important to know how blood clotting works to understand hemophilia. Blood clotting is a complex process. It involves many steps and factors to form a clot and stop bleeding.
Normal Clotting Process
When a blood vessel is damaged, the clotting process starts. This damage exposes the subendothelial tissue. This exposure triggers a series of reactions involving clotting factors, proteins in blood plasma.
The clotting cascade has three main pathways: intrinsic, extrinsic, and common. The intrinsic pathway is for damage inside the blood vessel. The extrinsic pathway is for external trauma. Both merge into the common pathway, leading to a fibrin clot.
How Clotting is Affected in Hemophilia
Hemophilia is a genetic disorder that affects blood clotting. It’s caused by a lack of clotting factors in the coagulation cascade. Hemophilia A lacks factor VIII, while Hemophilia B lacks factor IX.
People with hemophilia have trouble stopping bleeding. Even small injuries can cause a lot of bleeding. They might also bleed without any reason at all. The severity of hemophilia depends on how much clotting factor is in the blood.
Clotting Factor Deficiencies
Clotting factor deficiencies are key in hemophilia. The severity of the condition depends on the level of these factors in the blood. Table 1 shows how different levels of clotting factors affect hemophilia severity.
| Severity | Clotting Factor Level | Clinical Symptoms |
| Mild | 5-40% of normal | Bleeding after surgery or trauma, occasional spontaneous bleeding |
| Moderate | 1-5% of normal | Occasional spontaneous bleeding, prolonged bleeding after minor trauma |
| Severe | Frequent spontaneous bleeding, especially into joints and muscles |
Knowing about these deficiencies is key to managing hemophilia and avoiding its complications.
Blood Donation Basics
Blood donation rules change based on health and travel history. Knowing these rules is key for those who want to donate blood.
Who Can Donate Blood?
To donate blood, you must meet some criteria. You should be healthy, between 17 and 65 years old, and weigh at least 110 pounds. Donors also need to pass a screening test to make sure their blood is safe.
As a hematologist, notes, “The screening process is key. It keeps both the donor and the recipient safe.”
General Eligibility Requirements
To donate blood, you need to:
- Be in good physical and mental health
- Meet age and weight standards
- Not have certain medical conditions or take specific medications
- Not have traveled to areas with high infectious disease risks
The Screening Process
The screening for blood donation includes questions and tests. These check your health and the safety of your blood. This includes:
- A mini-physical exam to check vital signs
- A review of your medical history
- A hemoglobin test to check for anemia
- A questionnaire about disease risks
As the American Red Cross says, “The screening process is crucial. It spots risks and keeps the blood supply safe.”
“The safety of the blood supply is our top priority. We take every precaution to ensure that our donors are healthy and that their blood is safe for transfusion.” –
A, Blood Bank Director
Why Hemophiliacs Are Restricted from Donating Blood
hemophiliacs and blood donation
To understand why hemophiliacs can’t donate blood, we need to look at blood disorders and donation rules. Hemophilia is a genetic issue that makes it hard for the body to clot blood. Clotting is key to stop bleeding.
Medical Rationale
Hemophiliacs can’t donate blood because of their condition. They lack proteins needed for blood to clot. Taking blood out could make their condition worse.
Clotting factor deficiencies in hemophiliacs make donating blood risky. Their bodies can’t stop bleeding after giving blood.
Safety Concerns for Recipients
There are big safety worries for people who get blood from hemophiliacs. Their blood might have abnormal clotting factors or other harmful stuff. This is especially true for those with weak immune systems.
Safety Concerns for Donors with Hemophilia
Donating blood is risky for hemophiliacs. The process can cause bleeding problems. Keeping donors safe is a big part of blood donation rules.
FDA and Red Cross Guidelines
The FDA and the American Red Cross have rules against hemophiliacs donating blood. These rules aim to keep both donors and recipients safe from health risks.
The FDA’s guidelines stress the need to screen donors for health issues like hemophilia. This ensures the blood supply is safe.
What is Blood Infusion?
Blood infusion is a medical treatment that saves lives. It involves putting blood or its parts into a patient’s blood system. This is key for those needing specific blood types due to surgery, injury, or diseases.
The Blood Infusion Process
The process starts with checking the patient’s blood type. This makes sure the infused blood is compatible. The blood is then given through an IV, watched closely by doctors and nurses.
The steps are:
- Checking the patient’s blood type
- Putting in an IV
- Giving the blood or blood parts
- Watching for any bad reactions
Equipment and Procedures
For blood infusion, you need sterile needles, IV lines, and blood bags. Trained doctors and nurses do the job, following strict rules to keep risks low.
Important tools are:
- Sterile needles and IV lines
- Blood bags or containers
- Tools to watch patient health
Medical Settings for Blood Infusions
Blood infusions happen in hospitals, clinics, and sometimes outpatient places. Where it happens depends on the patient’s health, the procedure’s complexity, and the need for quick care.
Hospitals are where most blood infusions take place, especially for surgery or critical care. Outpatient clinics might do infusions for those with ongoing conditions needing regular transfusions.
Knowing about blood infusion is important for both patients and healthcare workers. It helps make sure the treatment is done right, helping patients get better.
Blood Infusion vs. Blood Transfusion: Understanding the Differences
The terms blood infusion and blood transfusion are often mixed up, but they mean different things in medicine. It’s important for doctors and patients to know the difference.
Terminology Clarification
Blood transfusion means moving blood or blood parts into someone’s blood to replace lost blood or boost its work. Blood infusion, however, is a wider term. It includes not just blood but also things like clotting factors or medicines directly into the blood.
When Each Procedure is Used
Blood transfusions are used when there’s a lot of blood loss, like in surgeries or injuries. They also help with anemia or to increase platelets in chemotherapy patients.
Blood infusions are for patients needing specific blood parts or medicines. For example, people with hemophilia get infusions of clotting factors to manage their disease.
Administration Methods
Both procedures use intravenous access. But, the exact methods and tools depend on the substance and the patient’s health.
For blood transfusions, checking the blood type and compatibility is key to avoid bad reactions. Blood infusions, especially clotting factors, need careful preparation and follow specific guidelines.
Knowing the difference between blood infusion and transfusion is key for good treatment and care. Both are vital in medicine, but they’re used in different ways.
Treatment Options for Hemophilia
Hemophilia treatment has evolved, offering various options. These include traditional factor replacement therapy and new gene therapies. The right treatment depends on the severity of hemophilia, the patient’s health, and their lifestyle.
Factor Replacement Therapy
Factor replacement therapy is key in treating hemophilia. It involves giving the missing clotting factor to the patient’s blood. This can be done prophylactically to prevent bleeding or on-demand to stop bleeding.
“Factor replacement therapy has changed how we manage hemophilia,” says a top hematologist. “It greatly reduces bleeding episodes.”
Gene Therapy Developments
Gene therapy is a new hope for hemophilia treatment. It aims to fix the genetic issue causing the condition. By adding a healthy gene to the patient’s cells, it could cure hemophilia.
- Several gene therapy trials are underway, showing promising results.
- The goal is for the patient’s body to make the clotting factor naturally.
Prophylactic vs. On-Demand Treatment
Choosing between prophylactic and on-demand treatment depends on several factors. Prophylactic treatment involves regular infusions to prevent bleeding. On-demand treatment is used when a bleeding episode occurs.
Emerging Treatments
New treatments are being researched, including non-factor therapies. These aim to improve clotting through different methods. These innovations could lead to better treatment outcomes and quality of life for those with hemophilia.
Hemophilia Carriers: What Does It Mean?
“Hemophilia carrier” means someone who has a gene for a bleeding disorder. This disorder makes it hard for blood to clot. Women who carry this gene have it on one of their X chromosomes. They can pass it to their kids.
Carrier Status Explained
A hemophilia carrier isn’t someone who has the disorder themselves. They are people who can pass the gene to their kids. Women have a 50% chance of passing the mutated gene to each son, who might have hemophilia. They also have a 50% chance of passing it to each daughter, who will likely become carriers.
Key Facts About Hemophilia Carriers:
- Female carriers have a 50% chance of passing the mutated gene to each child.
- Sons who inherit the mutated gene are likely to have hemophilia.
- Daughters who inherit the mutated gene typically become carriers.
Symptomatic Carriers of Hemophilia
Many female carriers don’t show symptoms of hemophilia. But, some might have bleeding issues because of how their genes work. These symptoms can be mild, like those in mild hemophilia.
Hemophilia Carrier Pregnancy Considerations
Pregnancy for carriers needs careful planning. They should talk to their doctor about being a carrier. Tests can show if the baby has the gene. Knowing this helps prepare for a child with hemophilia.
| Pregnancy Considerations | Description |
| Prenatal Testing | Testing to determine if the fetus has inherited the mutated gene. |
| Birth Planning | Preparing for the potential delivery of a child with hemophilia. |
| Genetic Counseling | Counseling for families to understand the risks and implications. |
Testing for Carrier Status
Testing for carrier status looks for the gene that causes hemophilia. Blood tests check for genes A and B. Knowing if you’re a carrier helps with family planning and pregnancy risks.
Genetic testing can provide peace of mind and valuable information for family planning.
Famous People with Hemophilia Throughout History
Hemophilia has touched the lives of many famous people. It’s a genetic disorder that makes it hard for the body to stop bleeding. This condition has been found in many royal families over time.
Contemporary Public Figures with Hemophilia
In recent times, many public figures have talked about living with hemophilia. They help raise awareness about the condition.
These modern figures are key in educating people about hemophilia. They help reduce the stigma around it.
Impact on Historical Events
Hemophilia has not just affected individuals but also historical events. It has influenced royal marriages and succession. Sometimes, it even changed the fate of empires.
For example, Tsarevich Alexei’s hemophilia was seen as a sign of divine displeasure. The influence of Rasputin over the royal family, due to his perceived ability to help the young prince, was a major factor leading up to the Russian Revolution.
Benefits and Importance of Blood Infusions
Blood infusions are very important, especially for those with hemophilia. They have changed how we treat many health issues. They give patients a way to manage their health better.
Life-Saving Applications
Blood infusions are key in emergencies when a lot of blood is lost. They are also crucial for patients having surgery or with conditions like hemophilia. Clotting factor infusions can save lives in severe bleeding cases.
Quality of Life Improvements
For many, blood infusions do more than just keep them alive. They make life better. Patients can live more active lives without the fear of bleeding. This is especially true for those with hemophilia, who can avoid bleeds with regular infusions.
Specific Benefits for Hemophilia Patients
Hemophilia patients get a lot from blood infusions, especially those that replace clotting factors. These infusions stop bleeds, reduce pain, and protect joints from damage. Regular infusions are key to managing hemophilia, helping patients live a more normal life.
| Benefit | Description | Impact on Hemophilia Patients |
| Life-Saving | Critical in emergency situations and acute bleeding episodes. | Prevents death from severe bleeding. |
| Quality of Life | Improves daily living by reducing the frequency of bleeds. | Enables patients to lead more active, normal lives. |
| Preventive | Prophylactic infusions prevent bleeds and joint damage. | Reduces long-term disability and pain. |
Risks and Complications of Blood Transfusions
It’s important for doctors and patients to know about the risks of blood transfusions. These transfusions are vital in many medical situations. But, they can also have risks and complications.
Common Transfusion Reactions
Transfusion reactions can vary in severity. Some common ones include:
- Febrile non-hemolytic transfusion reactions (FNHTR), which cause fever and chills.
- Allergic reactions, showing up as hives or itching.
- Acute hemolytic transfusion reactions (AHTR), a severe issue when the wrong blood type is given.
Long-term Risks
There are also long-term risks with blood transfusions. These include:
- Passing on infectious diseases like hepatitis and HIV, though the risk is much lower now due to strict screening.
- Iron overload, happening with regular transfusions.
- Graft-versus-host disease (GVHD), a rare but serious problem.
Minimizing Complications
To reduce risks, blood donors and recipients are carefully checked. This includes:
- Checking if the blood types match.
- Screening for infectious diseases.
- Watching patients closely during and after the transfusion.
Historical Perspective: HIV and Hemophilia
The 1980s saw HIV spread to hemophilia patients through tainted blood products. This was a big wake-up call for blood safety.
Nowadays, thanks to better screening, the chance of getting HIV from a blood transfusion is almost zero.
Blood Compatibility and Testing
Blood compatibility testing is key to avoiding bad reactions during blood transfusions. It’s important to make sure the donor and recipient blood types match. This ensures the transfusion is safe and successful.
Blood Types and Compatibility
Human blood is divided into four main types: A, B, AB, and O. These types are based on specific antigens on red blood cells. The Rh factor is also important, as it can be present (Rh positive) or absent (Rh negative). Knowing these factors helps in blood compatibility testing.
It’s crucial to match blood types to avoid hemolytic reactions. For example, Type A blood can only receive from Type A or O donors. Type AB can receive from AB, A, B, or O donors, making them universal recipients. On the other hand, Type O can donate to all ABO blood types, making them universal donors.
The Role of Blood Banks
Blood banks are essential for collecting, testing, and distributing blood. They make sure all donated blood is tested for blood type, Rh factor, and diseases like HIV and hepatitis. They use advanced tests to check for contaminants.
Key Functions of Blood Banks:
- Collection and processing of blood donations
- Testing for blood type and infectious diseases
- Storage and preservation of blood components
- Distribution of blood to hospitals and healthcare facilities
Screening for Blood-Borne Diseases
Testing donated blood for diseases is a critical step. Advanced tests are used to find viruses and bacteria. This multi-step process helps reduce the risk of infections from blood transfusions.
| Disease | Testing Method |
| HIV | Nucleic Acid Testing (NAT), Serological Tests |
| Hepatitis B | Serological Tests, NAT |
| Hepatitis C | NAT, Serological Tests |
| Syphilis | Serological Tests |
By testing blood thoroughly, blood banks protect public health. They make sure blood transfusions are safe for everyone.
Other Blood Disorders That Affect Donation Eligibility
Many blood disorders, aside from hemophilia, can make it hard to donate blood. These issues can make the blood supply less safe and less reliable. It’s important to know how they affect blood donation.
Factor V Leiden
Factor V Leiden is a genetic disorder that raises the risk of blood clots. It happens when a gene mutation leads to an abnormal protein. This protein doesn’t work right with activated protein C (APC). People with Factor V Leiden usually can’t donate blood because of this risk.
Key aspects of Factor V Leiden include:
- Increased risk of venous thromboembolism
- Genetic inheritance pattern
- Potential for asymptomatic carriers
Other Clotting Disorders
Other clotting disorders, like antithrombin deficiency, protein C deficiency, and protein S deficiency, also affect blood donation. These conditions can increase the risk of blood clots. This is a concern for those who might receive blood.
Common clotting disorders include:
- Antithrombin deficiency
- Protein C deficiency
- Protein S deficiency
- Prothrombin gene mutation
Temporary vs. Permanent Deferral Conditions
Donation eligibility can be impacted by both short-term and long-term conditions. Short-term deferrals might be due to recent travel, certain medications, or temporary health issues. Long-term deferrals often relate to chronic conditions or specific treatments.
It’s key to understand these conditions to keep the blood supply safe. Blood donation centers screen donors carefully. They make sure the blood is safe for transfusions.
Alternative Ways Hemophiliacs Can Contribute
Hemophiliacs can still make a big difference, even if they can’t donate blood. They can share their knowledge and experiences. This helps spread awareness and supports research.
Advocacy and Awareness
Hemophiliacs are key in raising awareness about bleeding disorders. By sharing their stories, they educate others. This helps build understanding.
- Participating in awareness campaigns and events
- Sharing personal stories through media and social platforms
- Supporting organizations dedicated to bleeding disorders
Through advocacy, more funding for research and better support services can be secured.
Research Participation
Getting involved in research is another important way hemophiliacs can help. By joining clinical trials, they aid in finding new treatments for hemophilia.
- Clinical trials for new treatments and therapies
- Genetic studies to understand the inheritance patterns of hemophilia
- Research on the quality of life for individuals with hemophilia
Research participation benefits both the individual and the broader understanding of hemophilia. It could lead to better treatments.
Supporting Blood Drives
Hemophiliacs can also help out at blood donation drives. They can organize events and encourage others to donate.
- Volunteering at blood donation centers
- Organizing community blood drives
- Raising awareness about the importance of blood donation
Supporting blood drives ensures patients get the blood they need.
Conclusion: The Importance of Blood Donation and Awareness
Blood donation is key to healthcare. Knowing about conditions like hemophilia helps raise awareness and encourage donations. This article has looked into hemophilia’s complexities, its effects on people, and blood donation rules.
Blood donation is crucial because it saves lives in many medical situations. It’s important to spread the word about hemophilia and how it affects who can donate blood. This helps build a supportive community.
Learning about blood disorders and how to donate helps us ensure a safe blood supply. It’s vital to promote education and awareness about hemophilia and blood donation. This fosters a culture of support and inclusivity.
FAQ
What is hemophilia?
Hemophilia is a genetic disorder. It makes it hard for the body to make blood clots. Blood clots are needed to stop bleeding.
Can people with hemophilia donate blood?
No, people with hemophilia usually can’t donate blood. This is because they might pass on their clotting disorder or face other problems.
What is the difference between hemophilia A and B?
Hemophilia A is when there’s not enough factor VIII. Hemophilia B is when there’s not enough factor IX.
What is von Willebrand disease?
Von Willebrand disease affects blood clotting like hemophilia. But it’s caused by a problem with the von Willebrand factor.
How is hemophilia diagnosed?
Doctors use blood tests to find out if someone has hemophilia. These tests check the levels of clotting factors in the blood.
What is blood infusion?
Blood infusion is when blood or blood parts are given to someone. It’s used to treat different health issues.
What is the difference between blood infusion and blood transfusion?
Blood infusion means giving specific blood parts. Blood transfusion is when whole blood or big parts of blood are given.
Can hemophilia carriers have symptoms?
Yes, some carriers of hemophilia can have symptoms. This is because of how the X-chromosome works, leading to less clotting factor.
What are the treatment options for hemophilia?
Treatments for hemophilia include factor replacement therapy and gene therapy. Prophylactic treatments also help prevent bleeding.
Can you donate plasma with an injury?
Usually, you can’t donate plasma if you’re injured. It depends on the injury’s type and how serious it is.
Can you donate blood with Factor V Leiden?
People with Factor V Leiden might not be able to donate blood. It depends on the blood bank’s rules.
What are the risks of blood transfusions?
Blood transfusions can cause reactions and spread diseases. They can also lead to iron overload.
How does blood compatibility testing work?
Blood compatibility testing finds your blood type. It makes sure the donated blood is safe to avoid bad reactions.
What is the role of blood banks in ensuring safe blood supplies?
Blood banks collect, test, and store blood. They make sure the blood is safe for use in transfusions.
How can individuals with hemophilia contribute to the community?
People with hemophilia can help by advocating and joining research studies. They can also support blood donation drives.