Bile duct resection is a complex procedure. It’s often needed for conditions like cholangiocarcinoma and blocked bile duct.
Patients getting bile duct surgery face different issues. This includes cancer that needs the removal of the cancerous part and some healthy tissue around it.
At places like Liv Hospital, patients get help from a dedicated team. They use the latest in patient care to help patients recover well.
Key Takeaways
- Bile duct removal surgery is a complex procedure.
- It’s often required for conditions like cholangiocarcinoma.
- A dedicated multidisciplinary team is key for the best recovery.
- Patients should know about possible complications.
- The surgery removes the affected part and some healthy tissue.
Understanding the Biliary System and Its Function
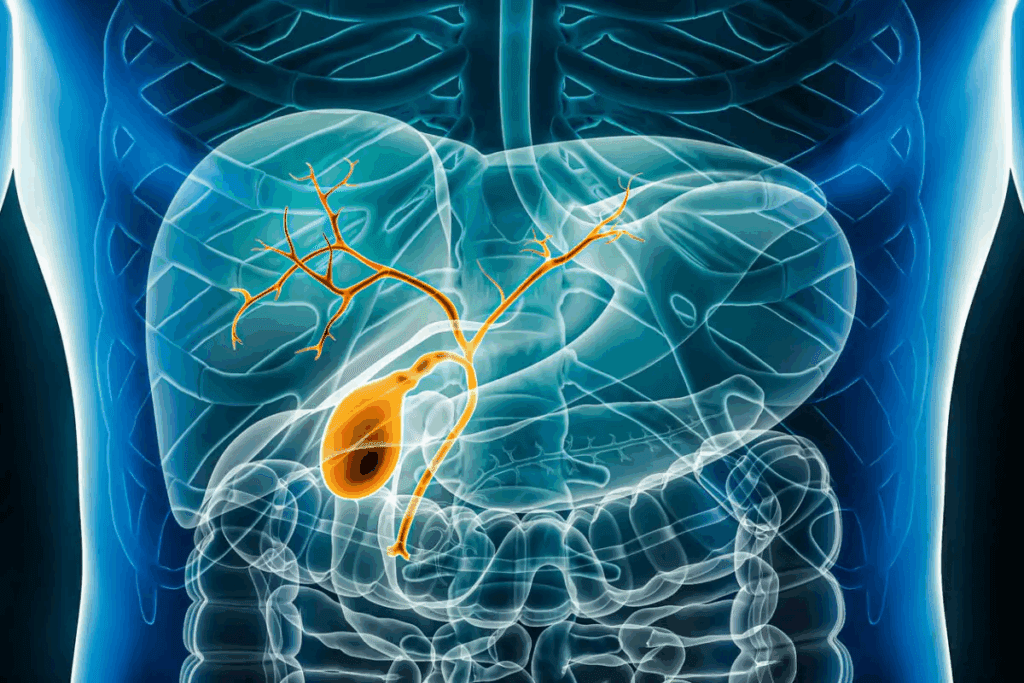
To grasp the details of bile duct removal, knowing the biliary system’s anatomy and its role in digestion is key. The biliary system, which includes the liver, gallbladder, and bile ducts, is vital for digestion.
Anatomy of the Bile Ducts
The bile ducts are a network of thin tubes linking the liver to the gallbladder and small intestine. They carry digestive bile from the liver to the intestine. Here, it helps with fat digestion.
The anatomy of the bile ducts is complex. The right and left hepatic ducts merge to form the common hepatic duct. This duct then joins the cystic duct from the gallbladder to form the common bile duct.
This network can face issues like blockages, strictures, and cancer. These problems might need surgery. Knowing the bile duct anatomy is key for diagnosing and treating these issues.
The Role of Bile in Digestion
Bile is a fluid made by the liver and stored in the gallbladder. It’s essential for digestion, breaking down fats for enzymes to act on. Bile also helps in absorbing fat-soluble vitamins like A, D, E, and K.
The bile duct function is vital for bile to reach the intestine. There, it can do its job in digestion.
Without a working biliary system, digestion problems can arise. This can lead to health issues. So, understanding the biliary system’s role in digestion is key to understanding bile duct removal surgery and its effects on digestive health.
Common Conditions Requiring Bile Duct Surgery
Surgery on the bile ducts is often needed for many biliary disorders. The bile duct system is key for digestion. Several conditions affect it, requiring surgery.
Cholangiocarcinoma (Bile Duct Cancer)
Cholangiocarcinoma, or bile duct cancer, is rare and aggressive. It starts in the bile ducts. Surgery is the main treatment to remove the tumor and affected ducts. But, only about 3 out of 10 people with bile duct cancer can have surgery.
Bile Duct Strictures and Blockages
Bile duct strictures are narrowings due to scar tissue. Blockages stop bile from flowing into the intestine. These cause jaundice, pain, and digestive problems. Endoscopic and surgical treatments are used, based on the issue’s location and severity.
| Condition | Symptoms | Treatment Options |
| Cholangiocarcinoma | Jaundice, weight loss, abdominal pain | Surgery, chemotherapy, radiation therapy |
| Bile Duct Strictures | Jaundice, itching, abdominal pain | Endoscopic dilation, stenting, surgery |
| Bile Duct Blockages | Jaundice, dark urine, pale stools | Endoscopic clearance, stenting, surgical bypass |
Bile Duct Injuries and Congenital Abnormalities
Bile duct injuries can happen during surgery or trauma. Congenital issues like choledochal cysts also affect the ducts. Surgical repair is needed to fix these problems and ensure bile flows right.
The need for bile duct surgery shows how complex biliary disorders are. Accurate diagnosis and treatment planning are key. It’s important for patients and doctors to understand these conditions well.
Types of Bile Duct Removal and Reconstruction Procedures
Bile duct removal surgery comes in many forms, each for different problems. The surgery type depends on the issue’s location and nature. This could be cancer, a stricture, or another problem.
Bile Duct Resection Techniques
Bile duct resection removes the sick part of the bile duct. It’s used for bile duct cancer or severe injuries. The surgery needs careful techniques to remove the sick part and keep the healthy part.
After resection, reconstruction techniques might be used. These help restore bile flow. This could mean reconnecting bile duct segments or making a new path for bile.
Biliary Bypass Surgery Options
Biliary bypass surgery is for when the bile duct is blocked. It can’t be cleared or removed right away. This surgery makes a detour to let bile flow into the intestine again.
- Bilioenteric anastomosis: This connects the bile duct or gallbladder to the small intestine. It lets bile bypass the blockage.
- Roux-en-Y hepaticojejunostomy: A more complex method uses intestine segments for bile drainage.
Partial Liver Resection with Bile Duct Removal
When bile duct cancer or disease hits a liver lobe, a partial liver resection might be needed. This removes the diseased liver part and bile duct.
Choosing partial liver resection depends on the disease’s extent and location. The goal is to remove all sick tissue while keeping enough liver function.
These surgeries show how complex and varied bile duct removal and reconstruction can be. Each patient needs a custom approach. The surgical team must weigh many factors to choose the best method.
Surgical Approaches for Blocked Bile Duct
Understanding the surgical options for blocked bile ducts is key to effective treatment. Blocked bile duct surgery is a complex procedure. It requires careful diagnosis and surgical intervention. The goal is to restore bile flow, alleviate symptoms, and prevent further complications.
Diagnostic Methods for Bile Duct Obstruction
Before surgery, accurate diagnosis of bile duct obstruction is essential. Diagnostic methods include:
- Imaging tests such as ultrasound, CT scans, and MRI
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Percutaneous transhepatic cholangiography (PTC)
Table 1: Diagnostic Methods for Bile Duct Obstruction
| Diagnostic Method | Description | Advantages |
| Ultrasound | Non-invasive imaging technique | Quick, painless, and widely available |
| ERCP | Endoscopic procedure to visualize bile ducts | Allows for simultaneous treatment |
| PTC | Imaging technique involving injection of contrast into bile ducts | Provides detailed images of bile ducts |
Blocked Bile Duct Operation Procedures
Several surgical procedures are available to address blocked bile ducts. These include:
- Biliary bypass surgery
- Bile duct resection
- Liver resection in cases where the blockage affects liver function
In some cases, biliary drainage may be performed before surgery. This can alleviate symptoms and improve liver function. This preliminary step can significantly impact the success of the subsequent surgical intervention.
Blocked Liver Duct Surgical Interventions
Surgical interventions for blocked liver ducts often involve a combination of techniques. The choice of procedure depends on the location and cause of the blockage, as well as the patient’s overall health.
Key Considerations:
- The expertise of the surgical team
- The specific anatomy of the patient’s biliary system
- The presence of any underlying conditions
By carefully evaluating these factors, surgeons can develop an effective treatment plan tailored to the individual patient’s needs.
How Complicated Is Bile Duct Removal Surgery?
The complexity of bile duct removal surgery depends on several factors. This surgery is needed for conditions like bile duct cancer, strictures, or blockages. It’s a major procedure.
Surgical Complexity Factors
Several factors make bile duct removal surgery complex. These include:
- The location and size of the tumor or affected area
- The presence of any anatomical abnormalities
- The patient’s overall health and medical history
- The need for additional procedures, such as liver resection or lymph node removal
The location of the bile duct is key in surgery complexity. Bile ducts are near vital structures like major blood vessels and the liver. This makes the surgery delicate.
Technical Challenges for Surgeons
Surgeons face many technical challenges in bile duct removal surgery. These include:
- Precise dissection to avoid damaging surrounding tissues
- Reconstruction of the bile duct to restore normal bile flow
- Managing possible complications, such as bleeding or bile leaks
A surgical expert notes, “The technical challenges in bile duct surgery are significant, requiring a high level of skill and experience.” (
This complexity highlights the need for specialized training and expertise in hepatobiliary surgery.
)
Case-by-Case Variability in Procedure Difficulty
Every patient’s situation is different, making each surgery unique. Factors like cancer stage, inflammation, or previous surgeries can affect complexity.
Personalized surgical planning is key to tackle each case’s specific challenges. A team of surgeons, radiologists, and oncologists work together. They create a customized surgical plan.
Bile Duct Cancer Surgery: Special Considerations
Bile duct cancer surgery is very specialized. It needs a deep understanding of the biliary system. The surgery for cholangiocarcinoma, or bile duct cancer, changes based on the cancer’s location, size, and stage.
Surgical Approaches for Cholangiocarcinoma
The main goal of surgery is to take out the cancerous part of the bile duct. Surgical resection is the only way to possibly cure bile duct cancer. The surgery type depends on where the tumor is:
- For cancers in the lower bile duct, a Whipple procedure (pancreaticoduodenectomy) might be used.
- For tumors in the upper or middle bile duct, a bile duct resection with or without liver removal might be needed.
Combined Procedures for Advanced Cancer
For advanced bile duct cancer, combined procedures might be needed. This includes removing the tumor and affected tissues. This can include:
| Procedure | Description |
| Bile Duct Resection with Liver Resection | Removing the bile duct and a part of the liver. |
| Liver Lobe Removal | Removing a liver lobe if the cancer has spread to it. |
| Pancreaticoduodenectomy (Whipple Procedure) | Removing the bile duct, gallbladder, part of the pancreas, and sometimes part of the stomach. |
Liver Lobe Removal in Cancer Treatment
Liver lobe removal, or hepatectomy, might be needed if the cancer has spread to the liver. The decision to remove a liver lobe depends on how much of the liver is involved and the patient’s liver function.
The surgical team’s skill in these complex surgeries is key for treating bile duct cancer. Knowing the details of each surgery and the possibility of combined procedures is vital for the best patient outcomes.
Preoperative Assessment and Patient Preparation
Getting ready for bile duct removal surgery is very important. A detailed check-up before surgery helps find any risks. It makes sure the patient is ready for the surgery.
Required Medical Tests and Imaging
Before surgery, patients need to do several tests and imaging studies. These include:
- Blood Tests: To check liver function, blood clotting, and overall health.
- Imaging Studies: Like CT scans, MRI, and ultrasound to see the bile ducts and nearby areas.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): To look at the bile and pancreatic ducts.
These tests give important info about the patient’s health. They help the surgical team plan the best surgery.
Consultation with Surgical Team
Talking to the surgical team is a big part of getting ready for surgery. During this talk, the surgeon will:
- Explain the surgery plan and what to expect during and after.
- Go over the test and imaging study results.
- Answer any questions or worries the patient has.
This talk helps reduce anxiety. It makes sure the patient knows what’s happening.
Physical and Mental Preparation for Surgery
Being physically and mentally ready is key for a good surgery outcome. Patients should:
- Maintain a Healthy Lifestyle: Eat well and exercise right.
- Manage Stress: Try meditation or counseling to help.
- Follow Preoperative Instructions: Fast before surgery and take meds as told by the doctor.
By focusing on these areas, patients can help make their surgery a success.
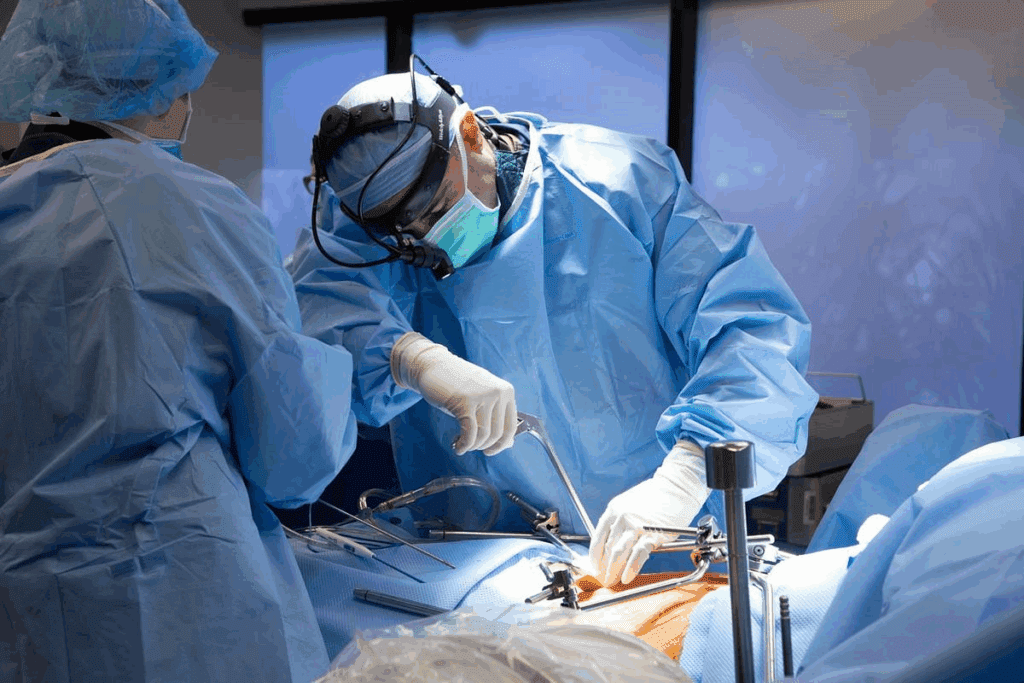
The Surgical Process: What Happens in the Operating Room
Knowing about the surgical process is key for those getting bile duct removal surgery. It helps set realistic hopes and lowers worry about the surgery.
Anesthesia and Surgical Setup
The surgery is done under general anesthesia. This keeps the patient comfortable and pain-free. The team gets the patient ready by giving anesthesia and setting up to watch vital signs.
The operating room has the latest tech. This includes top-notch imaging and precise tools for complex surgeries.
Open vs. Minimally Invasive Approaches
The choice between open surgery and minimally invasive surgery depends on several things. These include the patient’s health, the surgery’s complexity, and the surgeon’s skill. Open surgery needs a big cut to reach the bile ducts. Minimally invasive surgery uses small cuts and special tools.
Minimally invasive methods, like laparoscopic surgery, have benefits. They lead to quicker recovery and less pain after surgery. But, they might not work for all cases, like complex bile duct reconstructions.
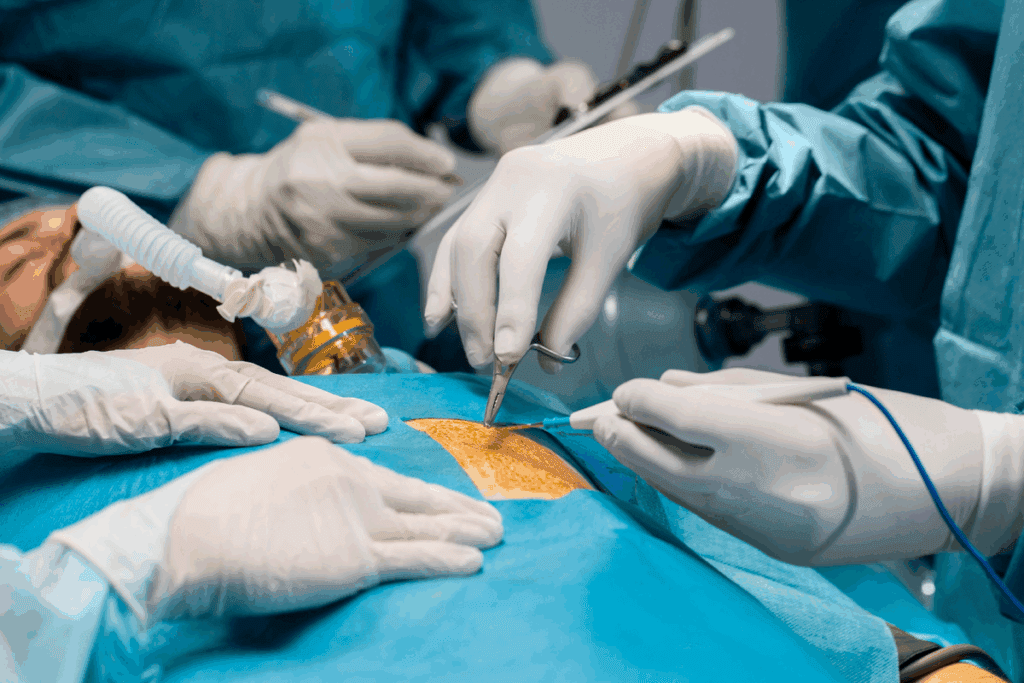
Reconstruction Techniques for Bile Flow
After removing the bile duct, the team works on reconstruction techniques to get bile flowing right again. They might make a new way for bile to go from the liver to the intestine. This is often done with a piece of the intestine to bypass the removed bile duct.
The aim of these reconstruction techniques is to make sure bile drains well and avoid future problems. The team’s skill in picking and using the right method is vital for the patient’s recovery and health in the long run.
In summary, the surgery for bile duct removal is a detailed process. It involves careful planning, precise work, and focusing on getting the digestive system working right again. By understanding these steps, patients can better get ready for the surgery and the healing process.
Potential Complications and Risks
It’s important to know the risks of bile duct removal surgery. This surgery is often needed but comes with big risks. These risks can affect how well a patient does after surgery.
Short-term Complications
Right after surgery, serious problems can happen. These include bile leaks and infections. Bile leaks happen when bile spills into the belly, which can cause infections or other big problems. Infections can come from the surgery or bile leaks.
A study on postoperative complications in biliary surgery shows how common these issues are. It’s key to spot and treat them quickly to manage them well.
| Complication | Description | Management |
| Bile Leaks | Unintended release of bile into the abdominal cavity | Drainage, antibiotics, possible reoperation |
| Infections | Infections arising from surgery or bile leaks | Antibiotics, supportive care |
Long-term Complications
Long-term problems can really affect a patient’s life. These include strictures and digestive issues. Strictures are when the bile ducts get narrower, blocking bile flow. Digestive problems come from changes in the biliary system’s function and anatomy.
Patients might see changes in bowel habits, trouble absorbing fats, and other digestive issues. Dealing with these problems often means ongoing medical care and changes in lifestyle.
Understanding High Complication Rates
It’s important to know that complication rates for biliary duct surgery can be 30 to 60 percent. This high rate is because of the surgery’s complexity, the patient’s health, and the challenges surgeons face.
Knowing these risks helps patients and doctors prepare for and handle complications when they happen.
Recovery Timeline and Post-Surgical Care
After bile duct removal surgery, patients start a critical recovery phase. This phase needs careful monitoring and post-surgical care. The recovery time can change based on the surgery’s complexity and the patient’s health.
Hospital Stay Duration and Intensive Care
The time spent in the hospital after bile duct removal surgery varies. It can be a few days to several weeks. Patients with complex surgeries or health issues might need more time and intensive care.
Key factors influencing hospital stay duration include:
- The extent of the surgery
- Presence of complications
- Patient’s overall health
Pain Management Strategies
Managing pain is key after bile duct removal surgery. Patients may feel different levels of pain. This can be managed with medicines and other methods.
Pain management strategies may include:
- Administration of analgesics
- Use of epidural anesthesia
- Alternative therapies such as acupuncture or relaxation techniques
Follow-up Care Schedule and Monitoring
After leaving the hospital, patients need a follow-up care plan. This plan helps monitor their recovery and catch any complications early. It includes regular check-ups and might include imaging tests.
The follow-up care schedule is designed to:
| Follow-up Care Aspect | Purpose | Frequency |
| Wound Check | Monitor healing and detect infection | Weekly for 2-3 weeks |
| Imaging Tests | Assess bile duct reconstruction and detect complications | At 1, 3, and 6 months post-surgery |
| Liver Function Tests | Evaluate liver health and function | At 1, 3, 6, and 12 months post-surgery |
Understanding the recovery timeline and following the post-surgical care plan helps patients heal better. It also reduces the risk of complications.
Long-term Lifestyle Adjustments After Bile Duct Surgery
After bile duct surgery, recovery is just the start. Patients must make lasting lifestyle changes. These changes affect their daily life in big ways.
Dietary Modifications and Nutritional Support
Diet is a big part of adjusting after surgery. Patients might need to eat differently to handle digestive changes. This could mean:
- Eating smaller, more frequent meals to ease digestion
- Avoiding fatty or greasy foods that can be hard to digest
- Increasing intake of fruits, vegetables, and whole grains
Getting enough nutrients is also key. Some might need supplements. A healthcare provider or nutritionist can help with this.
| Dietary Change | Benefit |
| Smaller, frequent meals | Eases digestion and reduces discomfort |
| Avoiding fatty foods | Reduces risk of digestive issues |
| Increased fiber intake | Improves digestive health |
Activity Restrictions and Gradual Return to Normal Life
Activity levels change after surgery. At first, patients should avoid hard work, heavy lifting, and bending. As they get better, they can start doing more.
It’s important to listen to the doctor about how much to do. Going back to normal slowly helps recovery.
“The key to a successful recovery is not just the surgery itself, but how well patients follow post-operative instructions and make necessary lifestyle adjustments.” – Medical Expert, Surgeon
Managing Digestive Changes and Possible Enzyme Supplements
After bile duct surgery, digestive changes are common. Some might have trouble with bowel movements or absorbing fat. In these cases, enzyme supplements can help.
It’s important for patients to watch their digestive health and tell their doctor about any big changes. Making diet or medication changes can help manage these issues.
By understanding and adapting to these changes, patients can improve their life after surgery. Regular check-ups with doctors are key for managing these long-term changes.
Conclusion: Navigating the Challenges of Bile Duct Surgery
Understanding and preparing for bile duct surgery is key. This surgery is complex and requires careful thought. Patients need to know about possible complications and lifestyle changes after surgery.
The success of bile duct removal surgery depends on several things. These include the condition being treated, the surgery’s extent, and the patient’s health. Knowing these factors and being ready for surgery can greatly improve the outcome and recovery.
Being informed and prepared helps patients face the challenges of bile duct surgery. It’s important for patients to follow their healthcare providers’ advice. They should also be aware of the risks and complications. With the right care, patients can have a good outcome and better their quality of life.
FAQ
What is bile duct removal surgery, and why is it performed?
Bile duct removal surgery is a complex procedure. It treats conditions like cholangiocarcinoma and bile duct blockages. The surgery removes the affected part of the bile duct and rebuilds the biliary system.
How complicated is bile duct removal surgery?
This surgery is complex and challenging. It’s because the biliary system is delicate and complications can happen. The surgery’s complexity depends on the condition, disease extent, and the patient’s health.
What are the different types of bile duct removal and reconstruction procedures?
There are many types of procedures. These include bile duct resection techniques and biliary bypass surgery. The choice depends on the condition and disease extent.
What is biliary bypass surgery, and when is it performed?
Biliary bypass surgery creates a new bile flow path. It’s for patients with blocked or damaged bile ducts. It helps relieve obstruction and restore bile flow.
Can the right lobe of the liver be removed during bile duct surgery?
Yes, sometimes the right lobe of the liver is removed. This is done along with bile duct removal. It’s for the diseased liver lobe.
What are the possible complications of bile duct removal surgery?
Complications can be short-term or long-term. These include bile leaks, infections, strictures, and digestive issues. The risk is high, between 30-60%.
How long does it take to recover from bile duct removal surgery?
Recovery time varies. It depends on the patient and the surgery complexity. Patients need weeks to months to fully recover and may need ongoing care.
What dietary modifications are necessary after bile duct surgery?
Dietary changes are needed after surgery. Patients may need to follow a specific diet and take enzyme supplements. They should also avoid certain foods.
What is cholangiocarcinoma, and how is it treated?
Cholangiocarcinoma is cancer of the bile ducts. Treatment includes surgery, chemotherapy, and radiation. Surgical options include bile duct resection and partial liver resection.
How is blocked bile duct diagnosed and treated?
Blocked bile duct is diagnosed with CT scans, MRI, and ERCP. Treatment involves surgery, like biliary bypass or bile duct resection. It aims to relieve obstruction and restore bile flow
References
- van Keulen, A. M., et al. (2021). Nationwide treatment and outcomes of perihilar cholangiocarcinoma: The importance of regional collaboration. PMC, 12(3), 25-34. https://pmc.ncbi.nlm.nih.gov/articles/PMC8359996/

































