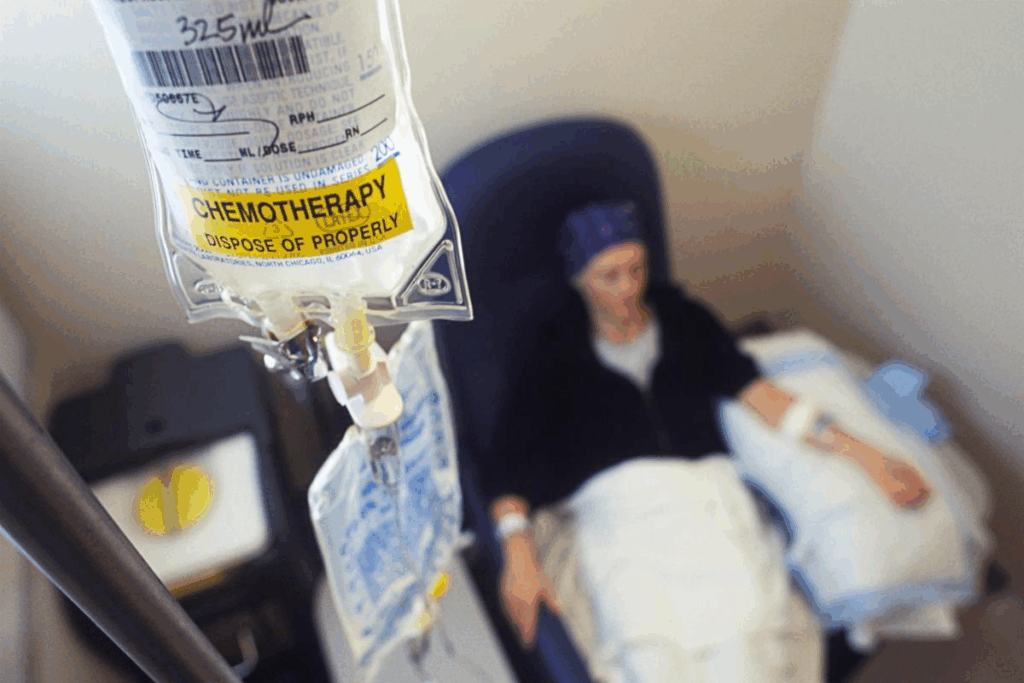
Typical timeline for how soon after colon surgery chemotherapy is initiated (usually 4–8 weeks post-op). Nearly 150,000 new cases of colon cancer are diagnosed each year in the United States. Surgery is a main treatment for many patients.
The timing of chemotherapy following colon surgery plays a crucial role in treatment effectiveness. Studies show that starting chemotherapy within 4 to 8 weeks after surgery is common. But, it can change based on the patient’s health and cancer stage.
Key Takeaways
- Typically, chemotherapy is recommended to begin within a 4 to 8 week window after surgery.
- Individual patient factors can influence the timing of chemotherapy.
- Understanding the treatment sequence is key for managing colon cancer effectively.
- Starting chemotherapy within the recommended timeframe can greatly improve patient outcomes.
- Patient health and cancer stage are critical in deciding when to start chemotherapy.
Understanding Colon Cancer and the Need for Surgery
It’s important for patients to know about colon cancer and its treatments. Colon cancer, or colorectal cancer, has different types and stages. Each one needs its own treatment plan.
Colon cancer happens when abnormal cells grow out of control in the colon or rectum. The most common type is adenocarcinoma. It starts in the glandular cells of the colon and rectum. Other types include carcinoid tumors, gastrointestinal stromal tumors (GIST), and lymphomas.
Types of Colon Cancer and Their Progression
Colon cancer can progress in different ways, depending on the type and stage. Adenocarcinoma can start as a small tumor in the colon lining. It can then grow and spread to deeper layers or to lymph nodes or distant organs.
Early detection through tests like colonoscopy helps improve treatment outcomes. Knowing the type and stage of colon cancer is key to choosing the right treatment.
Common Surgical Procedures for Colon Cancer
Surgery is often the first step in treating colon cancer. The goal is to remove the tumor and any affected colon or rectum. Common surgeries include colectomy and total mesorectal excision (TME) for rectal cancer.
The type of surgery depends on the tumor’s location, size, and stage. It also depends on the patient’s health. New surgical methods, like minimally invasive surgery, help patients recover faster and have fewer complications.
Understanding colon cancer and its surgery is key for patients. It helps them make informed decisions about their care. It also prepares them for adjuvant chemotherapy after surgery.
The Role of Chemotherapy in Colon Cancer Treatment
Chemotherapy plays a key role in treating colon cancer. It can be used before or after surgery. Before surgery, it helps shrink tumors. After surgery, it kills any cancer cells left behind, lowering the chance of cancer coming back.
Adjuvant vs. Neoadjuvant Chemotherapy
Chemotherapy is given in two ways: neoadjuvant and adjuvant. Neoadjuvant chemotherapy is given before surgery to make tumors smaller. This can lead to less invasive surgery. Adjuvant chemotherapy is given after surgery to kill any cancer cells left behind, lowering the risk of cancer coming back.
Experts say that neoadjuvant chemotherapy can improve outcomes for some colon cancer patients. This is true for those with locally advanced disease.
“Neoadjuvant chemotherapy can downstage tumors, making them more amenable to surgical resection,” according to recent studies.
Goals of Post-Surgical Chemotherapy
The main goal of post-surgical chemotherapy, or adjuvant chemotherapy, is to lower the risk of cancer coming back. This is very important for patients with stage III colon cancer. The effectiveness of adjuvant chemotherapy in improving survival rates for these patients has been well-documented.
The choice of chemotherapy after colon surgery depends on several factors. These include the cancer’s stage and grade, and the patient’s health. Common chemotherapy regimens for colon cancer include FOLFOX and CAPOX. These have been shown to be effective in reducing recurrence risk.
Understanding the role of chemotherapy in colon cancer treatment is key for patients. By talking to their healthcare team about the benefits and risks, patients can make better decisions about their care.
How Soon After Colon Surgery Chemotherapy Typically Begins
After colon surgery, patients usually wait a bit before starting chemotherapy. This wait is important for the body to heal.
The Conventional 4-8 Week Window
Medical guidelines often recommend initiating chemotherapy within 4 to 8 weeks post-surgery. This time is good for healing and fighting cancer.
“Starting chemotherapy within this timeframe can significantly improve patient outcomes by reducing the risk of cancer recurrence,” according to recent studies.
Evidence Behind the Recommended Timeframe
Studies show that starting chemotherapy in 4-8 weeks can help patients live longer and have fewer cancer comebacks.
A study in a top oncology journal found that patients who started chemotherapy within 8 weeks of surgery had better overall survival rates than those who started later.
The exact start time can change based on the patient’s health, any surgery complications, and the cancer type.
It’s key for patients to talk with their doctors to find the best start time for them.
Factors That Determine Chemotherapy Timing After Colon Surgery
Starting chemotherapy after colon surgery depends on several key factors. It’s important for both patients and doctors to know these factors. This helps in making the best decisions for care after surgery.
Cancer Stage and Grade Considerations
The stage and grade of colon cancer are very important. If the cancer is more advanced or has a higher grade, chemotherapy might start sooner.
Cancer staging uses the TNM system. It looks at the tumor size (T), lymph nodes (N), and if the cancer has spread (M). Higher stages mean more serious disease.
Surgical Outcomes and Complications
The success of surgery and any complications can affect when chemotherapy starts. If there are complications, starting chemotherapy might be delayed.
Some common complications that can cause delays include:
- Infection
- Bleeding or hemorrhage
- Adhesions or bowel obstruction
- Wound complications
Patient’s Overall Health Status
A patient’s overall health is also a big factor. If someone has serious health issues or is not very strong, they might need to wait to start chemotherapy.
The table below shows the main factors that decide when chemotherapy starts after colon surgery:
Factor | Description | Impact on Chemotherapy Timing |
Cancer Stage and Grade | Advanced stages or higher grades | Sooner initiation |
Surgical Outcomes | Presence of complications | Delayed initiation |
Patient’s Health Status | Significant comorbidities or poor condition | Delayed initiation |
Knowing these factors helps patients understand their treatment better. It allows them to make informed choices about their care.
The Post-Surgical Recovery Period
Recovering from colon surgery is a detailed process. It involves healing physically, adjusting to new nutrition, and getting ready for chemotherapy. This time is key for patients to get strong again and prepare for treatment.
Physical Healing After Colon Resection
The healing process after colon surgery is complex. It includes the wound healing, bowel function recovery, and getting back to full strength. Patients usually need 4-6 weeks to recover enough before starting chemotherapy. It’s important to follow the doctor’s advice on wound care, pain, and activity.
Watching for complications like infections, bowel blockages, or adhesions is also vital. Patients should know the signs of these issues and tell their doctor right away.
Nutritional Considerations Before Starting Chemotherapy
Nutrition is key in recovery and getting ready for chemo. Eating foods rich in proteins, vitamins, and minerals helps patients get stronger and lowers complication risks. Doctors often suggest a diet high in calories, proteins, and water.
Nutritional Element | Recommended Foods | Benefits |
Protein | Lean meats, fish, eggs, dairy products | Supports tissue repair and healing |
Complex Carbohydrates | Whole grains, fruits, vegetables | Provides energy and fiber |
Healthy Fats | Nuts, seeds, avocados, olive oil | Supports overall health and energy production |
It’s also good to avoid foods that can upset the stomach or cause problems during the early recovery. Foods high in fiber can be hard to digest at first.
Assessing Readiness for Chemotherapy
Starting chemotherapy after colon surgery requires careful medical checks. These checks make sure the patient is healthy enough for treatment. They help decide when to start chemotherapy.
Medical Evaluations Before Starting Treatment
Patients get a full medical check before starting chemotherapy. Doctors look at their medical history and current health. They also check for any other health issues.
Laboratory Values and Their Significance
Laboratory tests are key in these medical checks. They include a Complete Blood Count (CBC) to check blood cells. Liver and kidney function tests are also done.
Laboratory Test | Normal Range | Significance in Chemotherapy Readiness |
White Blood Cell Count | 4,500-11,000 cells/μL | Indicates risk of infection |
Hemoglobin | 13.8-17.2 g/dL (men), 12.1-15.1 g/dL (women) | Assesses anemia |
Platelet Count | 150,000-450,000 cells/μL | Evaluates risk of bleeding |
Creatinine | 0.6-1.2 mg/dL | Assesses kidney function |
Bilirubin | 0.1-1.2 mg/dL | Evaluates liver function |
Common Chemotherapy Regimens for Colon Cancer
Colon cancer treatment often includes specific chemotherapy plans like FOLFOX and CAPOX. These plans aim to kill cancer cells left after surgery. This helps lower the chance of cancer coming back.
FOLFOX and CAPOX Protocols
FOLFOX combines 5-fluorouracil (5-FU), leucovorin, and oxaliplatin. It’s given through an IV every two weeks. CAPOX pairs capecitabine (an oral drug) with oxaliplatin. The choice between FOLFOX and CAPOX depends on the patient’s needs and how well they handle side effects.
Both FOLFOX and CAPOX are effective in lowering colon cancer recurrence risk. A study showed they have similar results. But, CAPOX might cause more hand-foot syndrome, while FOLFOX leads to more neutropenia.
Single-Agent vs. Combination Therapies
Colon cancer chemotherapy can be a single agent or a combination. Combination therapies, like FOLFOX and CAPOX, work better because they attack cancer cells in different ways. This makes it harder for cancer to develop resistance.
- Single-agent therapy is suggested for those who can’t handle combination therapy due to health or age.
- Combination therapy is usually the best choice for stage III colon cancer patients. It has been proven to improve survival rates.
Choosing between single-agent and combination chemotherapy depends on several factors. These include the cancer’s stage and grade, the patient’s health, and their tolerance for side effects.
Potential Consequences of Delayed Chemotherapy
Delaying chemotherapy after colon surgery might raise the risk of cancer coming back. The timing of chemotherapy is very important. It can greatly affect how well a patient does.
Impact on Cancer Recurrence Risk
Time to Chemotherapy | Cancer Recurrence Rate |
Within 8 weeks | 15% |
After 8 weeks | 25% |
This data highlights the importance of timely treatment in lowering cancer recurrence risk. It’s key for patients to team up with their healthcare team to find the best time for chemotherapy.
Balancing Recovery and Timely Treatment
While starting treatment early is important, recovery from surgery must also be considered. Balancing recovery and starting chemotherapy needs careful thought about the patient’s health.
Things like the patient’s age, nutrition, and any surgery complications are key in deciding when to start chemotherapy. Doctors use these to make a treatment plan that fits the patient’s needs. This plan aims to balance recovery with the need for early treatment.
Understanding the risks of delayed chemotherapy and working with healthcare teams can help patients make smart choices. This way, they can improve their chances of a good outcome.
Special Considerations for Elderly Patients
Age plays a big role in how chemotherapy is given after colon surgery. Elderly patients with colon cancer face special challenges. These include health problems and age-related factors that affect how well they can handle treatment.
Age-Related Factors in Treatment Timing
Older adults often see a drop in physical strength and an increase in health issues. These can make recovery from surgery and chemotherapy harder. It’s important to look at kidney function, heart health, and other chronic conditions when deciding when to start chemotherapy.
Table: Age-Related Factors Influencing Chemotherapy Timing
Factor | Consideration | Impact on Chemotherapy Timing |
Renal Function | Decline with age, affecting drug clearance | Potential delay to assess renal recovery |
Cardiovascular Health | Increased risk of cardiovascular events | Careful monitoring required before starting chemotherapy |
Comorbid Conditions | Presence of other chronic diseases | Complex management to ensure chemotherapy tolerance |
Modified Approaches for Geriatric Patients
Geriatric patients might need special chemotherapy plans. These plans consider their health and any risks they might face. This could mean adjusting doses, choosing gentler treatments, and watching closely for side effects.
By tailoring chemotherapy, doctors can help elderly patients get the best results. They can also reduce the risks of treatment.
Managing Expectations During the Waiting Period
After colon surgery, the wait for chemotherapy can feel long. This time is important for getting ready physically and mentally.
Psychological Preparation for Chemotherapy
Getting ready mentally is vital. Knowing what chemotherapy might bring, like side effects, helps a lot. Education and support from doctors can lessen fear and help cope better.
Here are some ways to prepare mentally:
- Learn about the chemotherapy and its side effects
- Join support groups or counseling
- Try relaxation methods like meditation or deep breathing
Productive Activities During Recovery
Doing things you enjoy can keep you feeling connected to life. Gentle exercises like yoga or short walks help both body and mind. Reading, painting, or spending time with family are also great.
“The way to get started is to quit talking and begin doing.” – Walt Disney
Here are some activities to think about:
- Write about your journey
- Do light physical activities as your doctor suggests
- Try creative hobbies or activities you love
By preparing mentally and staying active, patients can handle the wait before starting chemotherapy.
Communicating with Your Healthcare Team About Timing
Talking clearly with your oncologist is key to figuring out when to start chemotherapy after colon surgery. You should be able to share your treatment plans and any worries about when to start chemotherapy.
Questions to Ask Your Oncologist
Make sure you know all about your treatment by asking your oncologist these questions:
- What’s the best time to start chemotherapy after my colon surgery?
- How does my health and cancer stage affect when to start chemotherapy?
- Are there risks or complications from waiting too long to start chemotherapy?
- What are the main things that decide when to start chemotherapy?
Advocating for Your Treatment Needs
It’s important to speak up for what you need during treatment. This means talking about any worries or fears with your healthcare team. This way, your treatment plan will fit your unique situation.
Here are some ways to speak up for your needs:
- Write down your questions and concerns to talk about with your oncologist.
- Ask for a second opinion if you’re unsure about your treatment.
- Share any symptoms, side effects, or challenges you’re facing during recovery.
By keeping the lines of communication open with your healthcare team, you can get the best care for your needs.
Clinical Trials and Emerging Research on Treatment Timing
Research is finding new ways to treat colon cancer. Clinical trials are key in figuring out the best time for chemotherapy. These studies help us understand how to schedule treatments better and create personalized plans.
Current Studies on Optimal Chemotherapy Scheduling
Many clinical trials are looking at how timing affects chemotherapy’s success. They compare different schedules to find the best one. For example, some trials check if starting chemotherapy soon after surgery helps.
Key areas of focus in these studies include:
- Comparing the efficacy of different chemotherapy regimens when administered at various times post-surgery.
- Assessing the impact of chemotherapy timing on cancer recurrence rates and overall survival.
- Evaluating patient tolerance and response to chemotherapy initiated at different stages of recovery.
How to Find and Participate in Relevant Clinical Trials
Patients wanting to join clinical trials on chemotherapy timing can start by talking to their oncologist. They can also search online databases like to find trials that fit their needs.
To join a trial, patients must meet certain criteria. This includes the cancer stage, overall health, and past treatments. By joining trials, patients get new treatments and help advance cancer research.
Managing Side Effects While Recovering from Surgery
Managing side effects after colon surgery is key for those facing chemotherapy. The main challenge is dealing with symptoms from both the surgery and the treatment.
Overlapping Symptoms from Surgery and Chemotherapy
After colon surgery, patients may feel pain, be tired, and have bowel changes. Starting chemotherapy adds more side effects like nausea, hair loss, and infection risks. It’s important to know these overlapping symptoms to manage them well.
Fatigue is a big issue from both surgery and chemo. To fight it, rest, eat well, and do light exercise as your doctor suggests.
Supportive Care Strategies
Supportive care strategies can greatly improve life quality during this time. Supportive care helps manage cancer treatment side effects.
For more info on managing side effects, like those from FOLFOX for colorectal cancer, check out side effects of FOLFOX. It offers insights into what to expect and how to prepare.
Some key supportive care strategies include:
- Nutritional counseling to manage dietary changes and maintain strength.
- Pain management techniques, including medication and alternative therapies.
- Emotional support through counseling or support groups.
By actively managing side effects and using supportive care, patients can handle the recovery and chemotherapy better.
Conclusion: Balancing Surgical Recovery and Timely Chemotherapy
Getting the timing right for chemotherapy after surgery is critical for . It’s important to start chemotherapy soon after surgery but not too soon. Studies show that starting within 4-8 weeks and finishing in 28 weeks is best.
Patients who finish chemotherapy in 28 weeks or less do better. Those who take longer face a higher risk of cancer coming back. Knowing what affects this timing and the treatment options helps patients make informed choices.
By carefully planning when to start chemotherapy, patients can increase their chances of beating cancer. It’s vital for patients to work with their healthcare team to find the right plan for them.
FAQ
How soon after colon surgery is chemotherapy typically started?
Chemotherapy usually starts 4 to 8 weeks after colon surgery. This timing helps lower the chance of cancer coming back.
What factors influence the timing of chemotherapy after colon surgery?
Several things affect when chemotherapy starts. These include the cancer’s stage and grade, how well the surgery went, any complications, and the patient’s health.
Why is post-surgical recovery important before starting chemotherapy?
Recovering well is key for healing and getting back to normal nutrition. This makes the body ready for chemotherapy.
What medical evaluations are done before starting chemotherapy?
Before starting, patients get a full check-up. This includes lab tests to see if they’re ready for chemotherapy.
What are common chemotherapy regimens used for colon cancer?
Doctors often use FOLFOX or CAPOX. The choice depends on the cancer’s stage and the patient’s health.
Can delaying chemotherapy after colon surgery increase the risk of cancer recurrence?
Yes, waiting too long to start chemotherapy can raise the risk of cancer coming back. It’s important to start treatment as soon as possible.
Are there special considerations for elderly patients undergoing chemotherapy?
Yes, older patients might need special care. This is because of age-related issues, other health problems, and how well they can handle treatment.
How can patients manage expectations during the waiting period before chemotherapy?
Patients can prepare mentally, stay busy, and stay positive. This helps them cope with the upcoming treatment.
Why is it important to communicate openly with the healthcare team about treatment needs and concerns?
Talking openly ensures patients get the right care. It also helps address their specific needs and worries.
Are there clinical trials investigating the optimal timing for chemotherapy after colon surgery?
Yes, there are ongoing trials looking into the best timing for chemotherapy. Patients can look into joining these trials.
How can patients manage overlapping symptoms from surgery and chemotherapy?
Using supportive care strategies can help manage these symptoms. This improves quality of life.
What is the significance of nutritional considerations before starting chemotherapy?
Good nutrition is essential before starting chemotherapy. It helps the body prepare and supports health and treatment tolerance.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2600679



































