Last Updated on November 27, 2025 by Bilal Hasdemir

When brain bleeding happens, quick medical help is key to avoid lasting brain damage. At Liv Hospital, we are committed to providing state-of-the-art, patient-focused care for international patients. They come to us for top-notch treatments for subdural hematoma.
Prompt recognition of symptoms is crucial for the best results. Our team of experts is here to offer comprehensive healthcare with care and understanding.
Treating subdural hematoma needs a team effort, and our hospital is ready to help. In this article, we’ll cover the basics of brain bleeding operations and the treatment options available.
Key Takeaways
- Timely medical intervention is crucial in treating subdural hematoma.
- Liv Hospital provides state-of-the-art, patient-focused care for international patients.
- Prompt recognition of symptoms is vital to prevent permanent neurological damage.
- A multidisciplinary approach is necessary for effective treatment.
- Our team of experts delivers comprehensive healthcare services with empathy and understanding.
Understanding Subdural Hematoma: Definition and Pathophysiology
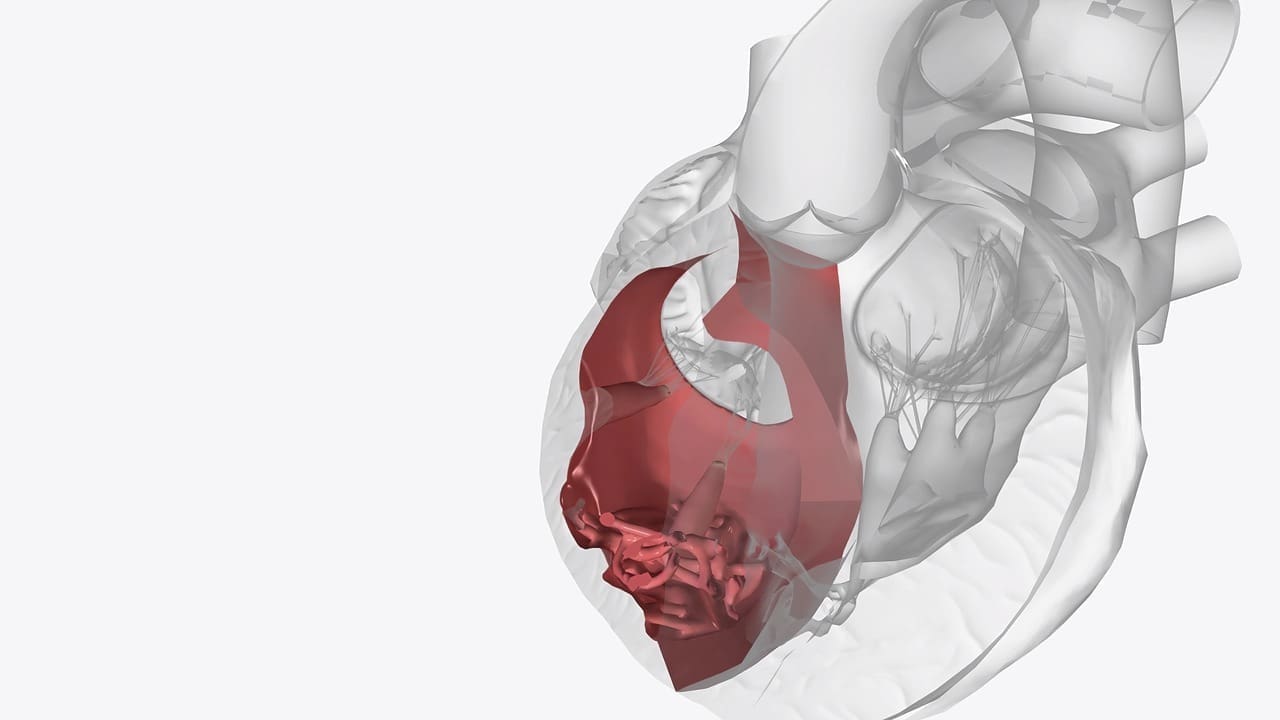
It’s important for both patients and healthcare providers to know about subdural hematoma. This condition happens when blood builds up between the brain and the dura mater. The dura mater is the outermost layer covering the brain.
A subdural hematoma usually results from a severe head injury. This injury causes the bridging veins to rupture. These veins connect the brain to the dura. The blood that leaks can put pressure on the brain, leading to damage or even death if not treated quickly.
Causes of Blood Collection Between Brain and Dura
Head trauma is the main reason for subdural hematoma. This trauma can come from falls, car accidents, or physical attacks. The force of the injury can stretch and tear the bridging veins.
Other things can also lead to subdural hematoma:
- Getting older, as the brain shrinks and the veins become more fragile
- Being on anticoagulant therapy, which increases bleeding risk
- Having had a subdural hematoma before
Types of Subdural Hematomas: Acute, Subacute, and Chronic
Subdural hematomas are divided into three types based on when symptoms start and the hematoma’s characteristics.
| Type | Time to Symptom Onset | Characteristics |
|---|---|---|
| Acute | Within 72 hours | Often linked to severe trauma; symptoms appear quickly |
| Subacute | 3 to 7 days | Symptoms develop more slowly than in acute cases |
| Chronic | More than 7 days, often weeks or months | More common in the elderly or those on anticoagulants; symptoms can be mild and change |
Knowing the type of subdural hematoma is key to choosing the right treatment. Treatments can range from watching and waiting to surgery.
Recognizing Subdural Hematoma Symptoms and Warning Signs

It’s key to spot the signs of subdural hematoma early to avoid serious brain harm. The symptoms can differ from person to person. Knowing the common signs and when to get medical help is vital.
Common Manifestations of Brain Bleeding
Subdural hematoma symptoms often start slowly. They can include various neurological problems. Here are some common signs:
- Headache: A severe headache is a common symptom. It feels like a pressure or pain in the head.
- Confusion and Disorientation: As the hematoma grows, it can cause confusion, disorientation, and trouble focusing.
- Weakness or Numbness: Patients may feel weakness or numbness in different body parts, depending on where the hematoma is.
- Vision Changes: Blurred vision, double vision, or loss of vision can happen due to brain pressure.
- Seizures: Subdural hematoma can cause seizures. This is a sign of increased brain pressure.
When Symptoms Indicate a Medical Emergency
It’s important to know when subdural hematoma symptoms mean you need to get medical help fast. If you or someone else is experiencing any of these, call for emergency care:
- Rapid Deterioration: Sudden worsening of symptoms, like increased confusion, severe headache, or loss of consciousness.
- Severe Neurological Deficits: Sudden severe weakness, numbness, or paralysis.
- Seizure Activity: If someone has a seizure or has had seizures before, get emergency care right away.
Knowing these symptoms and when to act can greatly help those with subdural hematoma. Quick medical help can prevent long-term brain damage and improve recovery chances.
Diagnostic Procedures for Subdural Hematoma
We use different tools to find and measure subdural hematoma. It’s key to get it right to choose the best treatment and help patients get better.
Imaging Techniques: CT Scans and MRIs
Imaging is crucial for spotting subdural hematoma. Computed Tomography (CT) scans are often first because they’re quick and good at finding fresh blood. They show where and how big the hematoma is, helping plan surgery if needed.
Magnetic Resonance Imaging (MRI) is also vital, especially for older hematomas. MRI shows more detail and helps figure out how old the hematoma is. This info is key for picking the right treatment.
Clinical Assessment and Neurological Examination
Checking the patient and doing a neurological exam are also important. Doctors look for signs like headaches, confusion, and weakness. This helps understand how bad the hematoma is and how it affects the brain.
Doctors also look at the patient’s past to see if anything might have caused the hematoma. This includes things like past head injuries or medicines. By combining what they see on scans with what they learn from the patient, doctors can make a good plan to help them.
Conservative Management Approaches
For some patients, conservative management approaches can handle subdural hematoma without surgery. This is especially true for those with small hematomas and mild symptoms.
When Surgery May Not Be Necessary
Not every subdural hematoma needs surgery. The choice to go for conservative management depends on several things. These include the hematoma’s size, the patient’s brain health, and any symptoms they have.
Research shows that small to moderate-sized hematomas with no or mild symptoms can be managed without surgery. This approach is safe for these patients.
- Patients with small hematomas (
- Those who are asymptomatic or have mild symptoms may also be managed without surgery.
- Close monitoring with regular imaging studies is crucial in these cases.
Medication and Monitoring Protocols
Conservative management uses medication and monitoring protocols to manage symptoms and prevent complications. Anticonvulsants may be given to prevent seizures. Medications to control blood pressure and intracranial pressure are also used.
Monitoring includes regular brain checks and imaging studies. These help track the hematoma’s size and the patient’s brain health. This close watch allows for quick action if the patient’s condition worsens.
In conclusion, conservative management is a good option for some patients with subdural hematoma. By carefully deciding when surgery is needed and using the right medications and monitoring, doctors can help patients get better.
Subdural Hematoma Operation: Surgical Intervention Overview
Deciding to operate on a subdural hematoma is complex. It depends on the patient’s health and the hematoma’s details. Surgery is key, but we must decide when it’s needed.
We look at many factors for surgery. These include the hematoma’s size and where it is, the patient’s brain function, and any other health issues. Prompt surgery is often needed for big hematomas or those causing serious symptoms.
Determining When Surgery Is Necessary
To decide on surgery, we check a few things:
- The size and thickness of the hematoma
- The patient’s level of consciousness and brain function
- Signs of increased brain pressure, like midline shift
- The patient’s overall health and surgery risks
Preoperative Preparation and Considerations
After deciding to operate, we prepare the patient well. This includes:
- Improving the patient’s health to lower surgery risks
- Doing imaging studies to plan the surgery
- Choosing the right anesthesia for comfort during surgery
By carefully planning surgery and preparing the patient, we can help improve outcomes. This is crucial for those undergoing a subdural hematoma operation.
Burr Hole Drainage Procedure for Subdural Hematoma
For those with subdural hematoma, burr hole drainage is a less invasive treatment. It involves making small holes in the skull to remove blood. This helps reduce pressure on the brain.
Technique and Implementation
The procedure is done under general or local anesthesia with sedation. A small incision is made in the scalp. Then, one or more burr holes are drilled.
A catheter is inserted to drain the blood. The blood is watched closely. Sometimes, the catheter stays in for a few days to make sure all blood is drained.
Key steps in the procedure include:
- Preoperative imaging to locate the hematoma accurately
- Creation of burr holes in the appropriate location
- Insertion of a catheter for hematoma drainage
- Postoperative monitoring of drainage and intracranial pressure
Ideal Candidates for Burr Hole Surgery
Not every patient with subdural hematoma is right for burr hole surgery. We look at the hematoma’s size and location, the patient’s age, and health. Those with chronic hematomas or who can’t handle big surgeries might benefit.
The benefits of burr hole drainage include:
- It’s minimally invasive, lowering the risk of problems
- Recovery is quicker than with bigger surgeries
- It helps lower brain pressure and ease symptoms
We choose patients carefully and tailor the procedure to fit their needs. This way, we get good results with burr hole drainage for subdural hematoma.
Craniotomy for Complex and Bilateral Subdural Hematomas
Craniotomy is a key surgery for complex and bilateral subdural hematomas. It needs a lot of skill and precision. This surgery lets neurosurgeons remove the hematoma directly, which helps prevent more brain damage.
Surgical Approach and Methodology
Craniotomy for subdural hematoma has several steps. First, the patient is made ready for surgery with the right anesthesia and position. Then, a scalp incision is made, and a bone flap is created to get to the brain.
The dura mater is then opened carefully to see the hematoma.
Key steps in craniotomy for subdural hematoma include:
- Evacuation of the hematoma
- Control of bleeding sources
- Decompression of the brain
- Closure of the dura mater and replacement of the bone flap
Special Considerations for Bilateral Cases
Bilateral subdural hematomas are more complex because they affect both sides of the brain. Special considerations include:
- Careful preoperative planning to assess the extent of hematoma on both sides
- Potential need for bilateral craniotomies or a more extensive surgical approach
- Monitoring for signs of increased intracranial pressure during and after surgery
A study in the Journal of Medical Case Reports found that timely and well-managed craniotomy greatly improves outcomes for these patients. It’s crucial to have a team of neurosurgeons, radiologists, and critical care specialists working together.
Emerging Minimally Invasive Techniques
Minimally invasive techniques are changing how we treat subdural hematoma. They offer safer options than traditional surgery. These new methods are thanks to better technology and a deeper understanding of the condition.
These new ways aim to lower risks like infection and brain damage. They also aim to improve patient outcomes and recovery times. Middle meningeal artery embolization and endoscopic hematoma evacuation are two promising techniques.
Middle Meningeal Artery Embolization
Middle meningeal artery embolization blocks the blood supply to the hematoma. This lets it dissolve naturally. It’s a minimally invasive method that shows promise in reducing surgery needs and complications.
- Benefits: Reduced risk of rebleeding, less invasive than traditional surgery
- Procedure: Embolization is done through a small incision in the groin. A catheter is guided to the middle meningeal artery under imaging.
Research shows this method works well for chronic subdural hematoma. It’s a good alternative to burr hole drainage or craniotomy.
Endoscopic Approaches to Hematoma Evacuation
Endoscopic hematoma evacuation uses a small endoscope to see and remove the hematoma. It’s a precise method that minimizes damage to the brain.
Key advantages of endoscopic approaches include:
- Reduced risk of brain damage due to minimal invasiveness
- Improved visualization of the hematoma during evacuation
- Potential for faster recovery times compared to open surgery
As research grows, these techniques will likely become more important in treating subdural hematoma. They offer patients more options and better outcomes.
Complications and Risks of Hematoma Head Surgery
Subdural hematoma surgery is a critical procedure for many patients. It can save lives but comes with risks. It’s important for patients and doctors to know about these risks and long-term effects.
Potential Surgical Complications
Subdural hematoma surgery has risks like infection, bleeding, and anesthesia reactions. These can happen during or after surgery. They might need extra medical care.
- Infection: As with any surgery, there is a risk of infection with subdural hematoma surgery.
- Bleeding: The risk of bleeding is inherent in any surgery, and subdural hematoma operations are no exception.
- Anesthesia Complications: Reactions to anesthesia can occur and may range from mild to severe.
Long-term Neurological Concerns
Patients may face long-term neurological issues after surgery. These can include cognitive problems, seizures, and other neurological deficits.
| Long-term Concern | Description | Potential Intervention |
|---|---|---|
| Cognitive Impairments | Patients may experience difficulties with memory, concentration, and other cognitive functions. | Rehabilitation therapy, cognitive training |
| Seizures | Some patients may develop seizure disorders following subdural hematoma surgery. | Anticonvulsant medication, seizure management protocols |
| Neurological Deficits | Depending on the location and severity of the hematoma, patients may experience various neurological deficits. | Physical therapy, occupational therapy, speech therapy as needed |
It’s key to know about these complications and risks. This helps manage patient expectations and improve care after surgery. Healthcare providers can offer better support by addressing these concerns.
Conclusion: Advances in Subdural Hematoma Treatment
We’ve looked into the challenges of subdural hematoma, a serious issue needing quick and right care. New ways to treat subdural hematoma have greatly helped patients, offering many options.
Liv Hospital leads in treating subdural hematoma, with plans made just for each patient. Our team offers everything from simple care to complex surgeries. We aim to give top-notch care.
The future of treating subdural hematoma is bright, with new, less invasive methods and ongoing research. We’re always looking to improve, aiming for the best results for our patients.
We mix the latest medical skills with caring for our patients. Our goal is to really help those with subdural hematoma.
FAQ
What is a subdural hematoma?
A subdural hematoma is when blood gathers between the brain and the dura. The dura is the outermost brain membrane. It can happen from head injuries, falls, or trauma. This puts pressure on the brain and can lead to serious issues if not treated quickly.
What are the symptoms of a subdural hematoma?
Symptoms can vary but often include headaches, confusion, and dizziness. You might also feel nauseous or vomit. In severe cases, you could lose consciousness or have seizures. It’s important to notice these symptoms early for timely medical help.
How is a subdural hematoma diagnosed?
Diagnosis usually involves CT scans or MRIs to see the hematoma. These tests help determine its size and location. Doctors also do clinical assessments and neurological exams to evaluate the patient’s condition.
What are the treatment options for a subdural hematoma?
Treatment options range from medication and monitoring for smaller hematomas to surgery. For larger or more complex cases, surgery like burr hole drainage or craniotomy might be needed. The choice depends on the hematoma’s size, location, and severity, along with the patient’s health.
What is burr hole drainage?
Burr hole drainage is a surgical procedure where small holes are drilled into the skull. It’s used to drain blood from subdural hematomas. This method is often chosen for patients who can be treated less invasively.
When is surgery necessary for a subdural hematoma?
Surgery is needed for large hematomas causing brain pressure or when other treatments fail. The decision to operate is based on the patient’s condition, imaging results, and neurological status.
What are the risks associated with subdural hematoma surgery?
Risks include infection, bleeding, and neurological issues. However, these risks are managed with careful preparation, surgical technique, and postoperative care.
What are emerging treatments for subdural hematoma?
New treatments include minimally invasive methods like middle meningeal artery embolization and endoscopic evacuation. These aim to reduce treatment invasiveness and improve results.
How can Liv Hospital support international patients with subdural hematoma?
Liv Hospital offers comprehensive care for international patients, including advanced treatments for subdural hematoma. Our team focuses on personalized, high-quality care, ensuring patient comfort and the best outcomes.
Why is timely intervention important for subdural hematoma?
Timely intervention is key to avoiding permanent brain damage and improving outcomes. Quick recognition of symptoms and proper treatment can greatly impact recovery and quality of life.
FAQ
What is a subdural hematoma?
A subdural hematoma is when blood gathers between the brain and the dura. The dura is the outermost brain membrane. It can happen from head injuries, falls, or trauma. This puts pressure on the brain and can lead to serious issues if not treated quickly.
What are the symptoms of a subdural hematoma?
Symptoms can vary but often include headaches, confusion, and dizziness. You might also feel nauseous or vomit. In severe cases, you could lose consciousness or have seizures. It’s important to notice these symptoms early for timely medical help.
How is a subdural hematoma diagnosed?
Diagnosis usually involves CT scans or MRIs to see the hematoma. These tests help determine its size and location. Doctors also do clinical assessments and neurological exams to evaluate the patient’s condition.
What are the treatment options for a subdural hematoma?
Treatment options range from medication and monitoring for smaller hematomas to surgery. For larger or more complex cases, surgery like burr hole drainage or craniotomy might be needed. The choice depends on the hematoma’s size, location, and severity, along with the patient’s health.
What is burr hole drainage?
Burr hole drainage is a surgical procedure where small holes are drilled into the skull. It’s used to drain blood from subdural hematomas. This method is often chosen for patients who can be treated less invasively.
When is surgery necessary for a subdural hematoma?
Surgery is needed for large hematomas causing brain pressure or when other treatments fail. The decision to operate is based on the patient’s condition, imaging results, and neurological status.
What are the risks associated with subdural hematoma surgery?
Risks include infection, bleeding, and neurological issues. However, these risks are managed with careful preparation, surgical technique, and postoperative care.
What are emerging treatments for subdural hematoma?
New treatments include minimally invasive methods like middle meningeal artery embolization and endoscopic evacuation. These aim to reduce treatment invasiveness and improve results.
How can Liv Hospital support international patients with subdural hematoma?
Liv Hospital offers comprehensive care for international patients, including advanced treatments for subdural hematoma. Our team focuses on personalized, high-quality care, ensuring patient comfort and the best outcomes.
Why is timely intervention important for subdural hematoma?
Timely intervention is key to avoiding permanent brain damage and improving outcomes. Quick recognition of symptoms and proper treatment can greatly impact recovery and quality of life.
References
- Subdural Hematoma. Retrieved from: https://www.nhs.uk/conditions/subdural-haematoma/
- New Treatment Combination for Subdural Hematoma Reduces Risk of Recurrence. Retrieved from: https://news.weill.cornell.edu/news/2024/11/new-treatment-combination-for-subdural-hematoma-reduces-risk-of-recurrence
- Subdural Hematoma. Retrieved from: https://healthcare.utah.edu/neurosciences/neurosurgery/subdural-hematoma