Last Updated on October 21, 2025 by mcelik
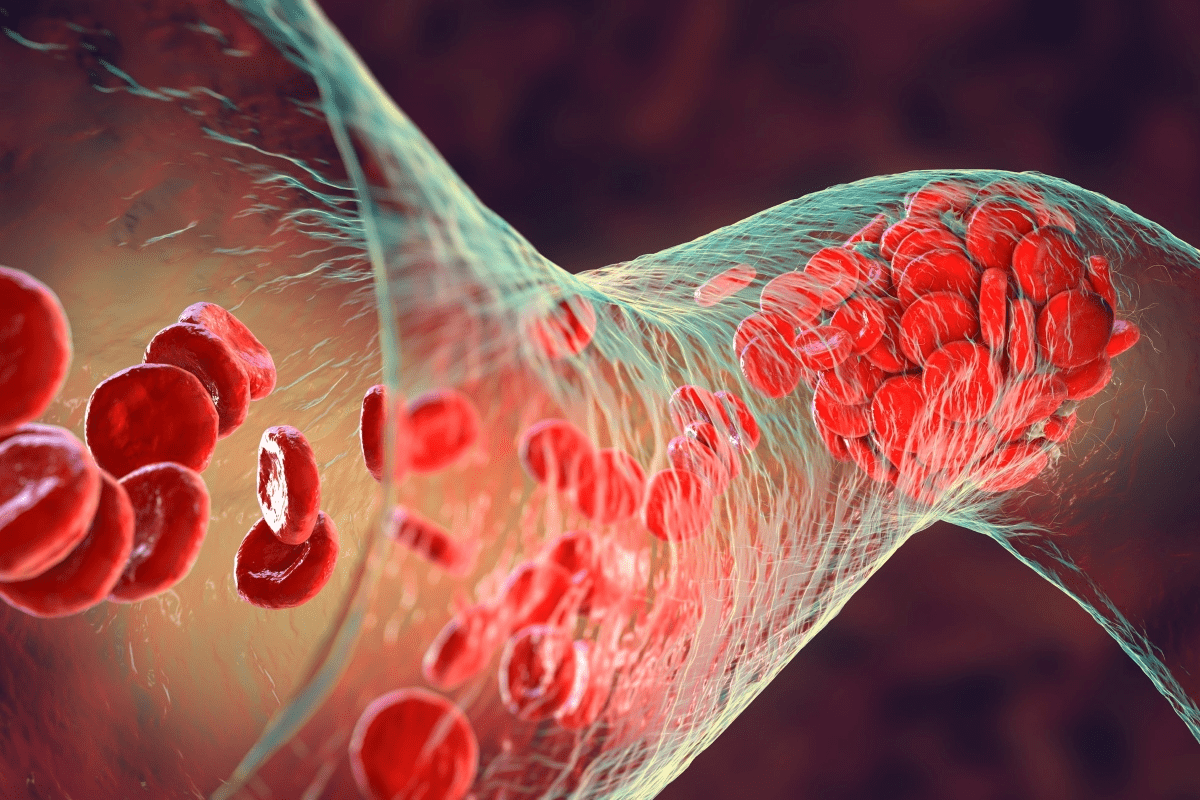
Did you know millions of people worldwide live with incurable blood disorders? These conditions greatly affect their daily lives. Sadly, some hematological conditions can’t be cured with today’s medicine.
Blood diseases can target red blood cells, white blood cells, or platelets. Each condition is complex, leading to different treatments and outcomes. The severity of the disorder plays a big role in how it’s managed.
We’ll dive into the details of these conditions, focusing on the ones without a cure. It’s important to understand these diseases. This knowledge helps us find new ways to treat them and improve patient care.
Key Takeaways
- Millions worldwide are affected by incurable hematological conditions.
- Blood diseases impact various blood components differently.
- Treatment outcomes vary based on the disorder’s severity.
- Understanding incurable blood diseases is key to advancing treatments.
- Research is ongoing to improve outcomes for patients with these conditions.
The Landscape of Blood Disorders

A detailed, photorealistic image of a person’s hand with various blood disorders and abnormalities, such as bruises, petechiae, and other visible signs of hematological conditions. The hand should be the focal point, occupying the center of the frame, with a soft, warm lighting that accentuates the textures and discolorations of the skin. The background should be slightly blurred and muted, creating a sense of focus on the hand. The overall mood should be somber and contemplative, conveying the gravity and complexity of blood disorders.
Blood disorders are complex because blood is essential for our health. It does many important jobs. Problems with blood can cause big issues.
How Blood Functions in the Body
Blood has several parts, each with its own job. Red blood cells carry oxygen, white blood cells fight germs, and platelets help blood clot. Together, they keep our body healthy.
Blood’s work is key for delivering oxygen and nutrients. It also removes waste. Any problem with this can lead to health issues. This shows why we need to know about blood disorders.
When Blood Components Malfunction
When blood parts don’t work right, it can cause many problems. For example, issues with red blood cells can lead to anemia. This makes you tired and weak because your body doesn’t get enough oxygen.
Problems with white blood cells can weaken your immune system. This makes you more likely to get sick.
- Anemia: A condition often caused by a deficiency in red blood cells or hemoglobin.
- Leukemia: A type of cancer that affects white blood cells.
- Hemophilia: A disorder that impairs the blood’s ability to clot due to a deficiency in clotting factors.
These examples show how blood disorders can affect us in different ways. It’s important to diagnose and treat them well.
Impact on Overall Health
Blood disorders can really affect your health. They can harm not just the blood but other parts of your body too. For instance, long-term anemia can strain your heart because it has to work harder to get oxygen to your body.
Living with a blood disorder can also affect your mind. Conditions like hematologic disorders can cause anxiety, depression, and lower your quality of life. This shows we need care that helps both your body and mind.
It’s key to understand blood disorders to find better ways to manage them. This can improve life for those affected.
Treatable vs. Incurable Blood Disorders
A detailed, close-up view of an human hand holding a petri dish filled with various blood cells, showcasing the complexity and diversity of incurable blood disorders. The image has a , diagnostic feel, with a neutral, slightly muted color palette and crisp, high-resolution details. The lighting is bright and even, highlighting the intricate structures and textures of the blood cells. The composition places the petri dish in the foreground, with a blurred background that suggests a medical or scientific laboratory setting. The overall mood is one of somber contemplation, conveying the gravity and difficulty of treating these challenging blood conditions.
Blood disorders range from curable to incurable conditions. It’s important for patients and healthcare providers to understand this.
Defining “Cure” in Hematology
In hematology, “cure” means a patient is treated and no longer shows signs of the disease. They can live a normal life. But, what a cure means can vary based on the disease and treatments.
Some blood cancers are considered cured if the patient stays disease-free for a while. Others, like chronic blood disorders, can’t be cured but managed with treatment.
“The goal of treatment for many blood disorders is not just to cure the disease but to manage it effectively, improving the patient’s quality of life.”
Factors That Make Blood Diseases Incurable
Several factors make a blood disease incurable. These include:
- Genetic mutations that are not easily reversible
- Complexity of the disease pathology
- Lack of effective treatment options
- Presence of comorbidities that complicate treatment
For example, Sickle Cell Disease is incurable because of its complex genetic mutation.
Management vs. Cure: Important Distinctions
Managing an incurable blood disorder is different from curing one. Cure aims to remove the disease. Management focuses on controlling symptoms and improving life quality.
| Aspect | Cure | Management |
| Goal | Eliminate the disease | Control symptoms and prevent complications |
| Treatment Approach | Aggressive treatment to achieve remission | Ongoing treatment to maintain quality of life |
| Patient Outcome | Normal life expectancy | Improved quality of life despite the disease |
Knowing these differences is key for setting realistic goals and making informed care choices.
Diagnosing Blood Disorders
A close-up view of a hands examining blood samples under a microscope, illuminated by warm, focused lighting. The laboratory setting is clean and , with test tubes, beakers, and medical equipment in the background. The focus is on the diagnostic process, with a sense of concentration and attention to detail. The mood is one of scientific inquiry and the pursuit of understanding blood disorders.
It’s key for both patients and to know about blood disorder diagnosis. Accurate diagnosis is vital for good treatment and management.
Common Diagnostic Tests
There are several tests used to diagnose blood disorders. These include:
- Complete Blood Count (CBC): Checks blood components like red and white cells, hemoglobin, and hematocrit.
- Bone Marrow Biopsy: Takes a small bone marrow sample for study.
- Blood Smear: Examines blood cell shapes in a lab test.
These tests help spot blood cell issues and diagnose specific disorders.
The Role of Genetic Testing
Genetic testing is crucial for diagnosing some blood disorders. It finds genetic mutations that cause diseases like sickle cell or thalassemia.
It also tells families about the risk of passing these conditions to their kids. This helps with family planning.
When to Seek Medical Attention
If you have symptoms that might mean a blood disorder, see a . Common signs include:
- Fatigue or weakness
- Pale skin
- Frequent infections
- Easy bruising or bleeding
Getting a diagnosis and treatment early can greatly improve outcomes for blood disorder patients.
| Diagnostic Test | Purpose | Examples of Conditions Diagnosed |
| Complete Blood Count (CBC) | Measures various blood components | Anemia, Leukemia |
| Bone Marrow Biopsy | Examines bone marrow for abnormalities | Leukemia, Lymphoma, Myelodysplastic Syndromes |
| Genetic Testing | Identifies genetic mutations | Sickle Cell Disease, Thalassemia |
Sickle Cell Disease: A Lifelong Genetic Blood Disorder
A detailed illustration of sickle-shaped red blood cells, their distorted morphology, and how they congest capillaries, causing vaso-occlusive crises. The scene is illuminated by warm, soft lighting that casts gentle shadows, creating a somber, contemplative mood. The background is hazy, out-of-focus, suggesting the complex, chronic, and systemic nature of this genetic blood disorder. The composition emphasizes the abnormal red blood cells, their sharp, crescent shapes, and the resulting blockages, conveying the debilitating impact of sickle cell disease.
Sickle cell disease is a genetic condition that affects red blood cells. It makes them misshapen. This is a big health problem worldwide, especially in areas where it’s common.
Pathophysiology and Genetic Basis
This disease comes from a gene mutation in the HBB gene. It codes for a part of hemoglobin. The mutation leads to sickle hemoglobin (HbS), which changes red blood cells into a sickle shape.
It’s inherited in an autosomal recessive pattern. This means you need two copies of the mutated gene to have the disease. Carriers have one copy and don’t show symptoms.
Symptoms and Complications
Symptoms of sickle cell disease vary. They often include pain crises from sickled red blood cells. Other issues include anemia, infections, and splenic sequestration.
Acute chest syndrome is a serious problem. It causes chest pain, fever, and lung issues seen on X-rays.
Current Management Approaches
Managing sickle cell disease involves several steps. These include prevention, treating acute problems, and long-term care.
Hydroxyurea helps reduce pain crises and may lower the risk of other issues. Blood transfusions help with severe anemia and prevent complications.
| Complication | Description | Management |
| Pain Crises | Episodes of pain due to vaso-occlusion | Hydration, pain management, hydroxyurea |
| Acute Chest Syndrome | Chest pain, fever, pulmonary infiltrates | Antibiotics, blood transfusions, supportive care |
| Anemia | Low red blood cell count or hemoglobin | Iron chelation, blood transfusions |
Hemophilia and Other Blood Clotting Disorders
A dimly lit hospital room, the soft glow of medical equipment casting a warm light across a patient’s face. In the foreground, a nurse gently administers an intravenous drip, their hands steady and experienced. The middle ground features a chart displaying the patient’s clotting factors, a testament to the complexities of hemophilia management. In the background, a window offers a glimpse of the city skyline, a reminder of the world beyond the confines of the hospital. The scene conveys a sense of care, dedication, and the ongoing challenges faced by those living with this lifelong blood disorder.
Blood clotting disorders, like hemophilia and von Willebrand disease, make it hard for the body to form blood clots. This leads to prolonged bleeding.
Types of Hemophilia
Hemophilia is mainly split into two types: Hemophilia A and Hemophilia B. Hemophilia A is due to a lack of factor VIII. Hemophilia B is caused by a lack of factor IX. The severity depends on how much clotting factor is in the blood.
We will explore each type and its impact on patient care.
| Type of Hemophilia | Clotting Factor Deficiency | Severity Levels |
| Hemophilia A | Factor VIII | Mild, Moderate, Severe |
| Hemophilia B | Factor IX | Mild, Moderate, Severe |
Von Willebrand Disease
Von Willebrand disease is a bleeding disorder that affects clotting. It’s caused by a lack or mutation of von Willebrand factor (VWF), a key protein for clotting.
Symptoms include easy bruising, nosebleeds, and heavy menstrual bleeding. Diagnosis involves tests to check VWF levels and activity.
Treatment Options and Limitations
Treatment for these disorders often involves replacing the missing clotting factor. For Hemophilia A, factor VIII concentrate is infused. For von Willebrand disease, desmopressin is used to release VWF.
But, there are challenges like the risk of developing inhibitors against clotting factors and the high of treatment.
Living with Clotting Disorders
Managing clotting disorders requires careful planning and lifestyle changes. Patients must avoid injuries, manage bleeding, and follow treatment plans.
Support from healthcare, family, and support groups is key to coping with these disorders.
Chronic Myeloid Leukemia (CML)
A detailed close-up view of chronic myeloid leukemia (CML) cells under a microscope. The image should capture the abnormal proliferation of myeloid cells, with their distinct shapes and sizes, set against a stark black background. Utilize a shallow depth of field to keep the foreground cells in sharp focus while the background fades into a deep, dark void, creating a sense of detachment. Employ cool, neutral lighting to convey the and scientific nature of the subject matter, with a slight vignette to draw the viewer’s attention to the center of the frame. The overall impression should be one of a meticulous, high-resolution medical illustration that clearly depicts the hallmarks of this blood disease.
Understanding CML has led to new treatments. Yet, it still poses a big challenge for patients and . CML is marked by the Philadelphia chromosome, a genetic mix-up between chromosomes 9 and 22. This mix-up creates a BCR-ABL gene, key to CML’s growth and spread.
The Philadelphia Chromosome
The Philadelphia chromosome is a key sign of CML, found in over 90% of cases. It leads to a BCR-ABL gene that makes cells grow out of control. Knowing this has helped in creating targeted treatments.
Tyrosine Kinase Inhibitors: Treatment Not Cure
Tyrosine kinase inhibitors (TKIs) have changed CML treatment. Drugs like imatinib, dasatinib, and nilotinib have greatly improved outcomes. Yet, CML is still a chronic disease, as TKIs don’t get rid of it completely.
TKI therapy offers many benefits:
- Improved survival rates
- Reduced risk of disease progression
- Management of symptoms
But, there are still hurdles like resistance to TKIs and side effects. These require constant monitoring and sometimes changes in treatment.
Long-term Prognosis and Challenges
Thanks to TKIs, CML’s outlook has greatly improved. Many patients now live active lives, managing CML as a chronic condition. But, challenges remain, like the need for lifelong treatment and the risk of TKI resistance or intolerance.
To tackle these issues, research is ongoing. It aims to develop new treatments and improve existing ones. Efforts include:
- Exploring combination therapies to boost effectiveness
- Creating next-generation TKIs with better safety
- Looking into curative options, like stem cell transplants, for some patients
By deepening our knowledge of CML and its treatment, we aim to better the lives of those with this complex disease.
Multiple Myeloma: An Incurable Blood Cancer
A detailed, photorealistic depiction of various treatment approaches for multiple myeloma, a type of incurable blood cancer. In the foreground, a molecular model of a chemotherapy drug interacts with a cancerous plasma cell. In the middle ground, a healthcare worker administers an intravenous infusion to a patient. In the background, a 3D rendering of a PET scan shows the distribution of myeloma lesions throughout the body. Subtle, warm lighting illuminates the scene, conveying a sense of medical expertise and scientific inquiry. Captured with a high-resolution DSLR camera, this image aims to educate and inform about the complex, multifaceted nature of treating this challenging disease.
Multiple myeloma is a tough blood cancer that harms plasma cells, key to our immune system. Plasma cells make antibodies to fight off infections. But in multiple myeloma, these cells turn bad, causing many problems.
Impact on Plasma Cells
Multiple myeloma makes plasma cells grow too much. This can damage bones, cause anemia, and raise the risk of infections. It also messes up antibody production, making patients more likely to get sick.
Symptoms and Progression
Symptoms of multiple myeloma vary but often include bone pain, tiredness from anemia, and frequent infections. As it gets worse, it can cause kidney failure and high calcium levels. Knowing how the disease progresses helps in managing it better.
Treatment Approaches
Even though multiple myeloma can’t be cured, there are ways to manage it. Treatments include targeted therapies, immunotherapies, and stem cell transplants. The right treatment depends on the patient’s health, age, and myeloma type.
Here’s a look at common treatments for multiple myeloma:
| Treatment Type | Description | Benefits |
| Targeted Therapy | Drugs that target specific aspects of myeloma cells | Can be more effective with fewer side effects |
| Immunotherapy | Treatments that enhance the body’s immune response against myeloma cells | Offers potential for improved outcomes |
| Stem Cell Transplant | Replacing damaged bone marrow with healthy stem cells | Can lead to significant remission periods |
Living with multiple myeloma is tough. But with the right treatment and support, many patients can manage their symptoms and live well. New research gives hope for better treatments in the future.
Myelodysplastic Syndromes (MDS)
Myelodysplastic syndromes (MDS) are a group of blood disorders. They happen when the bone marrow can’t make healthy blood cells. This can really affect a person’s life, so it’s important to know about them.
Classification and Risk Stratification
MDS is divided into types based on the blood cells affected and how severe it is. The World Health Organization (WHO) and the International Prognostic Scoring System (IPSS) help figure out how likely it is to get better. They also help decide the best treatment.
The IPSS is a tool used to group patients by risk. It looks at things like how many blood cells are missing, the bone marrow’s look, and how many cancer cells are there. Knowing the risk group is key to choosing the right treatment.
| IPSS Risk Category | Score | Prognosis |
| Low | 0 | Favorable |
| Intermediate-1 | 0.5-1.0 | Intermediate |
| Intermediate-2 | 1.5-2.0 | Poor |
| High | ≥2.5 | Very Poor |
Treatment Strategies Based on Risk
Treatment for MDS varies a lot. It depends on the patient’s risk level, age, and health. For those at lower risk, the goal is to improve life quality and manage symptoms. This might include blood transfusions and growth factors.
For those at higher risk, the aim is to change the disease’s course. This might involve stronger treatments like hypomethylating agents or stem cell transplants. Choosing the right treatment is a big decision that needs careful thought.
Transformation to Acute Myeloid Leukemia
One big worry for MDS patients is turning into acute myeloid leukemia (AML). This is a worse situation and needs a different treatment plan. This might include stronger treatments like chemotherapy or stem cell transplants.
It’s important to watch for signs of AML and adjust treatment plans as needed. Regular check-ups and changes to treatment are key to helping patients do better.
Thalassemia Major: Managing a Genetic Blood Disorder
Managing thalassemia major is complex. It affects patients’ lives deeply. This genetic blood disorder, also known as beta-thalassemia, severely impacts the body’s ability to make hemoglobin. This leads to severe anemia and other serious issues.
Alpha vs. Beta Thalassemia
Thalassemia is divided into alpha and beta types. Beta thalassemia major, or Cooley’s anemia, is very severe. It needs lifelong care. Alpha thalassemia can be mild or severe, based on how many genes are affected.
Transfusion Dependency and Iron Overload
Patients with thalassemia major often need regular blood transfusions. These transfusions save lives but can cause iron overload. This is when too much iron builds up in the body, harming organs like the heart and liver. To manage this, iron chelation therapy is used to remove excess iron.
Quality of Life Considerations
Improving life for thalassemia major patients goes beyond treating physical symptoms. It also involves addressing mental health. Supportive care, like counseling and education, is key. New treatments, like gene therapy, bring hope for better futures.
Rare Incurable Blood Disorders
The world of rare blood disorders is vast and varied. Conditions like PNH, polycythemia vera, and primary myelofibrosis are big challenges.
These disorders are different but share a common problem. They are incurable and need constant care.
Paroxysmal Nocturnal Hemoglobinuria (PNH)
PNH is a rare, life-threatening blood disease. It causes red blood cell destruction, bone marrow failure, and blood clots.
Symptoms of PNH include fatigue, shortness of breath, and abdominal pain. These are due to the destruction of red blood cells.
As a leading hematologist notes,
“PNH is a complex disorder. It needs a detailed treatment plan, often with several medications and supportive care.”
Polycythemia Vera
Polycythemia vera is a blood cancer. It makes too many red blood cells, white blood cells, and platelets.
Key symptoms include headache, dizziness, and itching. These happen especially after a warm bath or shower.
Managing polycythemia vera involves reducing red blood cells through phlebotomy. Medications are used to lower blood clot risk.
Primary Myelofibrosis
Primary myelofibrosis is a serious bone marrow disorder. It disrupts blood cell production, causing bone marrow scarring.
Common complications include anemia, fatigue, and spleen enlargement.
Treatment for primary myelofibrosis aims to manage symptoms and improve life quality. It often includes medications and, sometimes, bone marrow transplantation.
In conclusion, rare incurable blood disorders like PNH, polycythemia vera, and primary myelofibrosis are big challenges. They affect both patients and healthcare providers.
Living with Incurable Blood Disorders
People with incurable blood disorders face many challenges. They deal with physical symptoms, emotional distress, and financial worries. It’s important to tackle these issues in a holistic way.
Physical Challenges and Management
Managing the physical symptoms of incurable blood disorders is key. This means sticking to treatments and making lifestyle changes. Regular medical check-ups and adherence to prescribed treatments are crucial.
Patients often have to change their diet and avoid certain activities. For example, those with blood clotting disorders might avoid sports to prevent injuries.
Psychological Impact
The mental toll of living with an incurable blood disorder is huge. Managing symptoms and dealing with the unknown can cause anxiety and depression.
It’s vital for patients to get psychological support. This includes counseling, support groups, and therapy to handle the emotional strain.
Support Systems and Resources
A strong support system is essential for those with incurable blood disorders. This includes family, friends, and healthcare professionals. They offer emotional support and practical help.
- Support groups, whether in-person or online, provide a sense of community and understanding.
- Access to resources like counseling services and patient education programs is also crucial.
Financial Considerations
The financial impact of managing incurable blood disorders is huge. The of medical care, treatments, and hospital stays can be very high.
Patients and their families must deal with healthcare financing. This includes insurance and financial aid programs. Financial counseling can help reduce the financial stress.
Research and Future Treatments for Blood Disorders
The future of treating blood disorders is looking up. Medical research has made big strides. New therapies are showing great promise.
Gene Therapy Approaches
Gene therapy could be a big change in treating blood disorders. It aims to fix or replace faulty genes. This could lead to better treatments for genetic blood disorders.
“Gene therapy is a game-changer for genetic blood disorders,” says a . “It offers hope for a cure where there was none before.”
CRISPR and Genetic Editing
CRISPR-Cas9 technology has changed genetic editing. It lets us make precise changes to the human genome. This could be key in treating blood disorders by fixing genetic problems at their source.
Immunotherapy Advances
Immunotherapy uses the immune system to fight disease. It’s a big area of research for blood disorder treatments. CAR-T cell therapy, for example, has shown great results in some blood cancers.
trials are key in finding new treatments for blood disorders. They test new therapies in a safe way. Patients’ involvement is crucial for these trials.
We urge patients and families to look into trials. They are a big step towards new treatments.
Conclusion
We’ve looked into the complex world of blood disorders. We’ve seen how tough conditions like sickle cell disease, hemophilia, and some leukemias are. It’s key to understand these diseases well to find good ways to manage them.
Looking at how we manage blood diseases, we see some can be treated, but others need constant care. Research is vital in finding new treatments. Gene therapy, CRISPR, and immunotherapy are showing great promise.
As we go on, we must keep supporting those with these conditions. We need to give them the best care and the newest treatments. This way, we can make life better for those dealing with incurable blood disorders.
FAQ
What are blood disorders, and how do they affect the body?
Blood disorders affect how blood works. They can mess with red, white blood cells, and platelets. This can cause problems like anemia, infections, and issues with bleeding or clotting.
What is the difference between treatable and incurable blood disorders?
Treatable blood disorders can be fixed with today’s medicine. Incurable ones can’t be cured but can be managed to improve life quality.
What are some common diagnostic tests used to diagnose blood disorders?
Tests for blood disorders include CBC, blood smears, and bone marrow biopsies. Genetic testing and imaging like X-rays and CT scans are also used.
What is sickle cell disease, and how is it managed?
Sickle cell disease is a genetic issue that makes red blood cells break down. It’s managed with pain relief, blood transfusions, and medicines to prevent complications.
What is hemophilia, and how is it treated?
Hemophilia is a bleeding disorder due to missing clotting factors. It’s treated with clotting factor infusions. Sometimes, gene therapy is an option.
What is chronic myeloid leukemia (CML), and what are the treatment options?
CML is a cancer that affects white blood cells. It’s treated with tyrosine kinase inhibitors. These can manage the disease but can’t cure it.
What is multiple myeloma, and how is it treated?
Multiple myeloma is a cancer of plasma cells in the bone marrow. Treatment includes chemotherapy, targeted therapy, and stem cell transplants. Supportive care helps manage symptoms.
What are myelodysplastic syndromes (MDS), and how are they treated?
MDS affect blood cell production in the bone marrow. Treatment varies based on risk and may include supportive care, immunosuppressive therapy, and stem cell transplants.
What is thalassemia major, and how is it managed?
Thalassemia major is a genetic disorder that requires regular blood transfusions. Iron chelation therapy is also used to manage iron overload.
What are some rare incurable blood disorders?
Rare incurable blood disorders include PNH, polycythemia vera, and primary myelofibrosis. They need specialized care and support.
What are the challenges faced by individuals living with incurable blood disorders?
People with incurable blood disorders face physical and mental challenges. They need support systems and financial help to manage their condition.
How can individuals with blood disorders access support and resources?
People with blood disorders can find support through patient groups, online resources, and healthcare providers. These offer information, emotional support, and guidance.