
The inguinal canal is key in the human body, mainly in the reproductive system. Knowing its role helps us see its value in health and disease. It’s a major structure that lets important things move between the belly and the genitals. Our amazing, simple guide to the inguinal canal function. Discover its surprising, critical role in both male and female anatomy.
We’ll look into the anatomical significance of the inguinal canal and its role in keeping us healthy. By grasping its purpose, we can see how important it is to our bodies.
Key Takeaways
- The inguinal canal is a vital anatomical structure.
- It plays a key role in the reproductive system.
- Understanding its function is essential for health.
- The inguinal canal allows for the passage of vital elements.
- Its anatomical significance is vital for overall well-being.
The Inguinal Canal: An Anatomical Overview
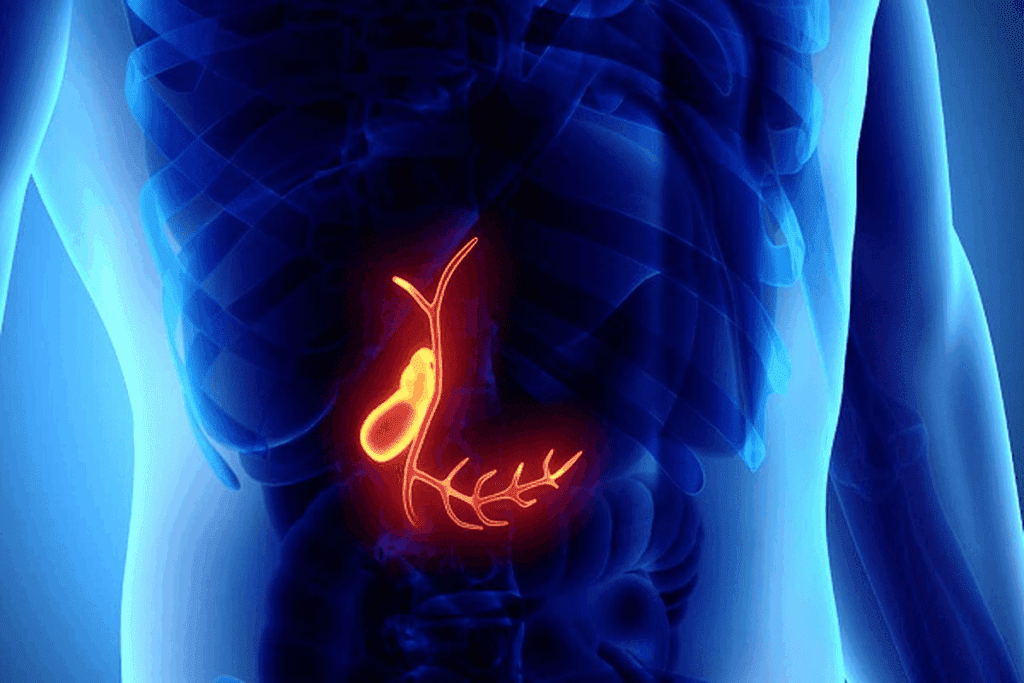
The inguinal canal is a key passage between the belly and the genitals. It’s very important in human anatomy, mainly for reproductive health and surgery.
Definition and Location
The inguinal canal is a path through the lower belly. It goes from the deep inguinal ring to the superficial inguinal ring. This spot is key for its job.
Evolutionary Significance
The inguinal canal is important in human evolution, mainly for males. It helps in the movement of testicles, showing its role in reproductive development.
General Structure
The inguinal canal has an anterior wall, posterior wall, floor, and roof. Knowing its parts helps us understand its role in human health and medical issues.
Our knowledge of the inguinal canal has grown a lot over time. This growth shows how medical science has advanced. The study of this area has been a journey with important milestones.
Early Anatomical Discoveries
For centuries, the inguinal canal has been studied by anatomists. Early findings were key to our modern understanding. At first, they just described where it is and its basic shape.
As methods got better, so did the details. This led to a deeper understanding of its role and importance.
Evolution of Medical Knowledge
Medical knowledge about the inguinal canal has changed a lot. New surgical techniques and tools have given us more insight. This has helped us understand its clinical importance better.
One big area of focus has been inguinal hernias. This has pushed research and treatment forward.
Our growing knowledge of the inguinal canal shows a bigger trend in medicine. It’s towards more specialized and precise treatments. As we learn more, we can handle health issues better.
Embryological Development of the Inguinal Canal
Understanding how the inguinal canal forms is key to knowing its role in the body. It develops in the womb, involving many parts. This process is complex and important.
Formation During Fetal Development
The inguinal canal starts to form around the 12th week of pregnancy. In boys, the testes move down through it. Girls have the round ligament do the same. The gubernaculum, a special ligament, helps guide these structures.
“The development of the inguinal canal is closely linked to the descent of the testes in males and the round ligament in females,” as noted by anatomical studies. This process is critical for the proper formation and function of the inguinal canal.
Developmental Milestones
There are important steps in the inguinal canal’s development. One is the closure of the processus vaginalis. This happens after the testes or round ligament reach their final place. If this doesn’t happen, inguinal hernias can form.
The inguinal canal is fully formed by birth. But, it might change a bit after birth. Knowing these milestones helps us understand the anatomy and problems of the inguinal canal.
Anatomical Boundaries of the Inguinal Canal
The inguinal canal has specific boundaries that are key to its function and health. These boundaries help define its structure and support its roles in the body.
Anterior Wall Components
The front wall of the inguinal canal is mainly made of the external oblique aponeurosis. It also gets some help from the internal oblique muscle. This wall protects and supports the canal well.
Posterior Wall Structure
The back wall of the inguinal canal is made of the transversalis fascia. In some spots, the conjoint tendon adds extra strength. This wall is important for keeping the canal separate from the preperitoneal space.
Floor Formation
The bottom of the inguinal canal is the inguinal ligament. It’s a strong part of the external oblique aponeurosis. The inguinal ligament helps set the canal’s lower edge.
Roof Composition
The top of the inguinal canal is made of the arching fibers of the internal oblique and transversus abdominis muscles. These muscles offer dynamic support to the canal.
Knowing the anatomical boundaries of the inguinal canal is vital. It helps us understand its complex structure and function. Each part works together to support the canal’s role in our bodies.
The Inguinal Canal Function: Primary Purposes
The inguinal canal is a key passageway in our bodies. It helps with many reproductive processes. Its main roles are vital for the reproductive system to work right.
Passage for Reproductive Structures
The inguinal canal lets reproductive structures move between the belly and the genitals. In guys, it’s where the spermatic cord goes. This cord has important parts for the testicles to work.
This journey through the canal is complex. It needs many parts working together. The canal’s design helps keep the spermatic cord safe and working well.
Communication Between Abdomen and External Genitalia
The inguinal canal connects the belly and the genitals. It lets structures move back and forth. This is key for the reproductive system to function.
Knowing how the inguinal canal works is important. It helps doctors diagnose and treat reproductive issues. Here’s a quick look at its role in communication:
Function | Description | Clinical Significance |
Passage for Spermatic Cord | Allows for the transit of the spermatic cord between the abdomen and external genitalia | Critical for testicular development and function |
Communication Between Cavities | Facilitates exchange between abdominal cavity and external genitalia | Influences the spread of infection or disease |
In conclusion, the inguinal canal’s main jobs are closely tied to our reproductive system. Knowing about these roles is key for both learning about the body and for medical practice.
The Inguinal Canal in Males
In males, the inguinal canal is key for the testes to move down. It also holds important parts of the reproductive system. This path lets the spermatic cord go from the belly to the scrotum, which is vital for male fertility.
Testicular Descent Pathway
The inguinal canal helps the testes move down during fetal development. They usually move into the scrotum between the 28th and 35th weeks. The gubernaculum, a fibrous cord, guides them through this canal.
Spermatic Cord Components and Function
The spermatic cord goes through the inguinal canal. It has important parts like the vas deferens, testicular arteries, and veins. These parts help with sperm production and transport. The cord is also protected by cremasteric fascia and internal spermatic fascia.
Gubernaculum Role
The gubernaculum is very important for guiding the testes down. It’s a fibrous structure that links the testes to the scrotum. Problems with it can cause undescended testes or cryptorchidism.
Structure | Function | Clinical Significance |
Spermatic Cord | Contains vas deferens, testicular arteries, and veins | Critical for spermatogenesis and sperm transport |
Gubernaculum | Guides testes through inguinal canal during descent | Abnormalities can lead to undescended testes |
Inguinal Canal | Passageway for spermatic cord and testicular descent | Weakness can lead to inguinal hernias |
The Inguinal Canal in Females
In females, the inguinal canal is key for the reproductive system. It’s a vital structure that connects the abdominal cavity to the external genitalia. This connection is essential for the passage of important elements.
Round Ligament Function
The round ligament of the uterus is a fibromuscular tissue in the inguinal canal. It starts from the uterine horns, goes through the canal, and ends in the labia majora. Its main job is to support the uterus, keeping it in the right position in the pelvic cavity.
Even though it doesn’t directly support the uterus, it helps keep the uterus in its anteverted position.
Structure | Function |
Round Ligament | Supports the uterus, maintaining its position |
Inguinal Canal | Allows passage of the round ligament |
Anatomical Differences from Males
There are big differences between males and females in the inguinal canal. In males, the canal carries the spermatic cord, which has the vas deferens, blood vessels, and nerves. Females have a smaller canal that mainly carries the round ligament. These differences come from the different reproductive roles and structures in each sex.
Knowing these differences is key for diagnosing and treating inguinal canal issues. We’ll look deeper into these differences to understand the unique female inguinal canal better.
Contents of the Inguinal Canal
The inguinal canal holds a mix of important structures. These help with reproduction and keeping the body healthy.
Spermatic Cord Structure
In males, the spermatic cord is key. It’s a bundle of vas deferens, blood vessels, nerves, and lymphatic vessels in the inguinal canal. It’s vital for testicular function and making sperm.
Vas Deferens Pathway
The vas deferens is a muscular tube in the spermatic cord. It goes through the inguinal canal and into the pelvic area. There, it joins the seminal vesicles to form the ejaculatory ducts. It’s important for storing and moving sperm.
Blood Vessels
The inguinal canal has blood vessels for the testes and nearby areas. These include the testicular arteries, cremasteric arteries, and vasal arteries. They bring oxygen and nutrients to the reproductive organs.
Nerves
The inguinal canal also has nerves like the ilioinguinal nerve and the genital branch of the genitofemoral nerve. These nerves help with feeling in the inguinal area and controlling the cremaster muscle around the spermatic cord.
In summary, the inguinal canal is filled with vital structures for reproduction and health. Knowing about these is key to understanding human anatomy and solving health problems.
Muscular Components and Their Role
It’s important to know about the muscles around the inguinal canal. This area is more than just a passageway; it is supported by a complex set of muscles essential for its function.
The muscles around the inguinal canal are the external oblique, internal oblique, and transversus abdominis. Each muscle has a big role in how the inguinal canal works and stays strong.
External Oblique Muscle
The external oblique muscle is the biggest and outermost of the three. It makes the external ring of the inguinal canal and offers important protection. The external oblique aponeurosis is a tough part that helps make the front wall of the inguinal canal.
Internal Oblique Muscle
The internal oblique muscle is under the external oblique and is part of the conjoint tendon. It helps make the back wall of the inguinal canal strong. In men, its fibers also protect the spermatic cord.
Transversus Abdominis Muscle
The transversus abdominis muscle is the deepest abdominal muscle. It works with the internal oblique to make the conjoint tendon, strengthening the back wall of the inguinal canal. This muscle is key to keeping the inguinal canal strong and supporting it.
In summary, the muscles around the inguinal canal are essential for its structure and function. The external oblique, internal oblique, and transversus abdominis muscles work together. They provide a strong support system, making sure the inguinal canal works well.
The Inguinal Ligament: Structure and Function
Understanding the inguinal ligament is key to knowing the inguinal region’s structure and function. It’s a major anatomical part that makes up the floor of the inguinal canal. It’s important for support and marks the boundary between the abdominal cavity and the thigh.
Anatomical Relationships
The inguinal ligament is made from the external oblique aponeurosis and connects with the thigh’s fascia lata. It runs from the anterior superior iliac spine (ASIS) to the pubic tubercle, setting a clear boundary. It’s closely related to the spermatic cord in males and the round ligament in females.
The inguinal ligament’s role in the inguinal canal is vital. It has key relationships, including:
- Attachment to the pubic bone
- Proximity to the femoral vessels
- Association with the spermatic cord or round ligament
Supportive Role in the Inguinal Region
The inguinal ligament is essential for supporting the inguinal region. It acts as a fibrous boundary to stop abdominal contents from herniating into the inguinal canal. It works with other structures like the external and internal oblique muscles to keep the inguinal region intact.
The inguinal ligament’s role can be summed up as follows:
- Provides a strong fibrous boundary
- Prevents herniation of abdominal contents
- Works in conjunction with other muscles to maintain regional integrity
In conclusion, the inguinal ligament is a critical anatomical structure. It offers vital support to the inguinal region. Its relationships and role are essential for keeping the inguinal canal intact and preventing diseases.
Vascular and Lymphatic Drainage
Understanding the vascular supply and lymphatic drainage of the inguinal canal is key. It shows us how it works and why it’s important. The inguinal canal is a passage through the abdominal wall. It needs a complex network of blood vessels and lymphatic channels to function well.
Arterial Supply
The arterial supply comes from branches of the external iliac artery, mainly the inferior epigastric artery. This artery helps the anterior abdominal wall and is vital for the inguinal canal. The cremasteric artery, a branch of the inferior epigastric artery, also supplies the spermatic cord in males.
Venous Drainage
The venous drainage works with the arterial supply. Blood is drained through the inferior epigastric veins into the external iliac veins. In males, the pampiniform plexus of veins around the testicular arteries drains into the testicular veins. These veins then go to the inferior vena cava on the right and the renal vein on the left.
Lymphatic System
The lymphatic drainage goes to the inguinal lymph nodes. These nodes are in the inguinal region. They get lymph from the lower abdominal wall, external genitalia (except the testes), and the lower limbs. The lymph then moves to the external iliac lymph nodes and then to the para-aortic lymph nodes.
System | Description | Key Structures Involved |
Arterial Supply | Derived from branches of the external iliac artery | Inferior Epigastric Artery, Cremasteric Artery |
Venous Drainage | Accompanies arterial supply, draining into external iliac veins | Inferior Epigastric Veins, Pampiniform Plexus, Testicular Veins |
Lymphatic Drainage | Drains into inguinal lymph nodes | Inguinal Lymph Nodes, External Iliac Lymph Nodes, Para-aortic Lymph Nodes |
Nerve Supply to the Inguinal Region
Understanding the nerve supply to the inguinal region is key. It helps us grasp its importance in both anatomy and medicine. The nerves in this area are vital for our body’s functions.
Ilioinguinal Nerve
The ilioinguinal nerve comes from the lumbar plexus. It sends signals to the inguinal area, genitalia, and upper thigh. It goes through the inguinal canal and comes out at the superficial inguinal ring.
It covers the upper thigh skin and the penis or scrotum in men. In women, it affects the mons pubis and labia majora.
Iliohypogastric Nerve
The iliohypogastric nerve also starts in the lumbar plexus. It helps with the sensation in the inguinal area. It splits into two branches, covering the lower abdomen and hip.
This nerve is important for feeling in the abdominal wall.
Genital Branch of Genitofemoral Nerve
The genital branch of the genitofemoral nerve innervates the cremaster muscle. It also sends signals to the spermatic cord, testicles, and nearby areas. In men, it’s involved in the cremasteric reflex.
In women, it connects with the round ligament of the uterus.
Clinical Significance: Inguinal Hernias
Inguinal hernias are important to understand. They happen when tissue, like part of the intestine, bulges through a weak spot in the abdominal muscles. The inguinal canal is a key area where these hernias often occur.
Direct vs. Indirect Hernias
Inguinal hernias are mainly two types: direct and indirect. Indirect inguinal hernias happen when tissue goes through the internal inguinal ring. This is a natural weak spot in the abdominal wall. Then, it goes through the inguinal canal. On the other hand, direct inguinal hernias occur when tissue bulges through the abdominal wall in the inguinal canal’s back wall, but not through the internal inguinal ring.
Indirect hernias follow the path of the spermatic cord (in males) or the round ligament (in females). Direct hernias bulge directly through the abdominal wall.
Characteristics | Indirect Inguinal Hernia | Direct Inguinal Hernia |
Pathway | Through internal inguinal ring | Through posterior wall of inguinal canal |
Common Cause | Congenital or acquired weakness | Acquired weakness due to strain |
Risk Factors and Prevalence
Several factors can lead to inguinal hernias. These include age, gender, family history, and conditions that increase abdominal pressure. Heavy lifting, chronic coughing, or obesity are examples. Males are more likely to get inguinal hernias because of the natural weakness in the abdominal wall where the testes descend.
“The lifetime risk of developing an inguinal hernia is approximately 27% in men and 3% in women.”
NHS Choices
Symptoms and Diagnosis
Symptoms of inguinal hernias vary. They often include a bulge in the groin area, discomfort or pain, and a feeling of heaviness or aching. A healthcare provider may ask the patient to cough or strain to diagnose a hernia during a physical examination.
It’s important to seek medical attention if symptoms don’t go away or get worse. Untreated hernias can lead to serious complications like incarceration or strangulation.
Surgical Approaches to the Inguinal Canal
Effective treatment of inguinal canal disorders depends on the surgeon’s knowledge of different methods. We will look at the main surgical techniques used for inguinal canal problems.
Open Repair Techniques
Open repair is a traditional method for treating inguinal hernias and other issues. It involves making an incision in the groin to directly access the inguinal canal. Open repair techniques are often chosen for their simplicity and effectiveness in some cases.
Laparoscopic Approaches
Laparoscopic surgery is a less invasive option compared to open repair. It uses small incisions for a laparoscope and surgical tools to fix the inguinal canal. Laparoscopic approaches are known for quicker recovery times and less scarring.
Postoperative Considerations
Postoperative care is key for patients after inguinal canal surgery. It includes managing pain, watching for complications, and advice on returning to normal activities. Comparing open repair and laparoscopic approaches helps understand their differences.
Criteria | Open Repair | Laparoscopic Repair |
Invasiveness | More invasive | Less invasive |
Recovery Time | Generally longer | Typically shorter |
Pain | Often more painful | Usually less painful |
Scarring | Larger scar | Smaller scars |
Cost | Generally less expensive | Can be more expensive |
It’s important to understand these surgical methods and postoperative care for effective treatment and patient care.
Other Pathologies Related to the Inguinal Canal
The inguinal canal can face other serious issues aside from hernias. These problems affect health and need careful medical attention. It’s key to know about these conditions for proper diagnosis and treatment.
Hydrocele Formation
A hydrocele is a fluid sac around a testicle, causing swelling. It happens when fluid production and absorption are out of balance. Hydroceles can be present at birth or develop later due to inflammation, trauma, or blocked lymphatic drainage. Treatment depends on the cause and symptoms, ranging from waiting and watching to surgery.
Varicocele Development
A varicocele is like varicose veins in the scrotum. It’s more common on the left side because of how the body is built. Varicoceles can cause pain, infertility, and shrinkage of the testicles if not treated. Doctors use embolization or surgery to fix it and help with fertility.
Cryptorchidism and the Inguinal Canal
Cryptorchidism, or undescended testes, happens when testes don’t move down into the scrotum. The inguinal canal is the usual path for this movement. Cryptorchidism raises the risk of infertility, testicular cancer, and other issues. Early treatment, often surgery, is vital to avoid these problems.
These conditions show how vital the inguinal canal is in health issues. Getting the right diagnosis and treatment is key to managing these problems well.
Conclusion
We’ve looked closely at the inguinal canal, its parts, and how it works. This important part of our body helps with reproduction and connects the abdomen to the genitals. It’s a key passage for many bodily functions.
The way the inguinal canal develops in the womb and its structure are key to its role. Knowing about it helps doctors diagnose and treat problems like hernias and varicoceles. This knowledge is also important for keeping our bodies healthy.
In summary, our detailed look at the inguinal canal shows its vital role in our bodies. It’s essential for both medical professionals and anyone interested in health. Understanding the inguinal canal helps us appreciate its importance in our overall well-being.
FAQ
What is the primary function of the inguinal canal?
The inguinal canal is a passageway. It connects the abdomen to the external genitalia. It also helps with the movement of reproductive structures.
What is the difference between the inguinal canal in males and females?
In males, the canal carries the spermatic cord. Females have the round ligament of the uterus. The canal’s structure and function differ due to reproductive anatomy.
What is the role of the gubernaculum in testicular descent?
The gubernaculum guides the testes through the inguinal canal. It helps them move into the scrotum during fetal development.
What are the boundaries of the inguinal canal?
The canal is defined by its boundaries. These include the anterior, posterior walls, floor, and roof. Each part has specific structures that help with its function.
What is an inguinal hernia, and how is it related to the inguinal canal?
An inguinal hernia happens when tissue bulges through a weak spot. This often occurs through the inguinal canal. It can cause pain and discomfort.
What are the different types of inguinal hernias?
There are direct and indirect hernias. Direct hernias push through a weak spot. Indirect hernias go through a natural opening in the canal.
What are the symptoms of an inguinal hernia?
Symptoms include a bulge in the groin and pain. This pain is often worse when coughing, lifting, or bending.
How is an inguinal hernia diagnosed?
Doctors use a physical exam and medical history to diagnose. Imaging tests like ultrasounds or CT scans may also be used.
What are the treatment options for inguinal hernias?
Treatment options include watchful waiting, open repair, and laparoscopic surgery. The choice depends on the hernia’s size and the patient’s health.
What is the significance of the inguinal ligament?
The inguinal ligament supports the inguinal region. It helps form the canal’s floor, contributing to its stability.
What are the muscular components surrounding the inguinal canal?
The canal is surrounded by muscles. These include the external oblique, internal oblique, and transversus abdominis. They provide support and help with function.
What is the role of the ilioinguinal nerve in the inguinal region?
The ilioinguinal nerve supplies sensory innervation. It covers the upper medial thigh and parts of the genitalia.
What is cryptorchidism, and how is it related to the inguinal canal?
Cryptorchidism is when testes don’t descend into the scrotum. This can happen during fetal development or early childhood.
What is a hydrocele, and how is it related to the inguinal canal?
A hydrocele is a fluid-filled sac around a testicle. It’s often related to the processus vaginalis, a peritoneal extension through the canal during fetal development.
What is a varicocele, and how is it related to the inguinal canal?
A varicocele is an enlarged vein in the spermatic cord. It passes through the canal and can affect fertility and testicular function.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470204/








