Last Updated on December 2, 2025 by Bilal Hasdemir
Did you know that accurate surgical diagnosis during operations can greatly improve patient outcomes? Intraoperative diagnosis is a key technique used during surgeries. It lets surgeons assess patients in real-time, helping them make better decisions. Learn what is an intraoperative diagnosis. Understand a diagnosis made during the course of a surgical procedure clearly.
This method checks tissue samples or other tests during surgery. It gives surgeons immediate insights. This helps them perform more precise surgeries, leading to better care for patients.
The importance of intraoperative diagnosis is clear. It offers real-time diagnostic info. This directly affects the success of surgeries.
Intraoperative diagnosis is about figuring out a disease or condition while a patient is being operated on. It’s key for making the right surgical choices and getting the best results for the patient.
This method is great because it gives doctors real-time info. They can change their plan right away. This is super important in complex surgeries where quick decisions are needed.
To get intraoperative diagnosis, you need to know some important terms. Intraoperative findings are the info doctors get during surgery. This can be what they see, biopsy results, and more.
Some key terms for intraoperative diagnosis are:
|
Term |
Description |
|---|---|
|
Frozen Section Analysis |
A quick histopathological check used during surgery. |
|
Cytological Examination |
Examining cells to diagnose conditions. |
|
Rapid Immunohistochemistry |
A fast method for identifying specific proteins in tissues. |
Intraoperative diagnosis has changed a lot over time. At first, doctors just looked and used simple tools. But new tech and pathology have made it much better.
Things like frozen section analysis have really helped. They make intraoperative diagnosis more accurate and reliable. This leads to better care for patients by allowing for more precise and timely surgeries.

Intraoperative diagnosis is key to the success of modern surgery. It gives surgeons real-time info during surgery. This helps them make quick, informed decisions that greatly affect patient outcomes.
Being able to diagnose during surgery is crucial for making timely and accurate decisions. Intraoperative diagnosis lets surgeons change their plans as needed. This can prevent complications and improve the surgery’s outcome.
In oncological surgery, it helps decide how much tumor to remove. This ensures all cancer is taken out while keeping healthy tissue. This precision is key for the surgery’s success and the patient’s long-term health.
Intraoperative diagnosis has led to better patient outcomes. It allows for real-time adjustments during surgery. This can lower the risk of complications and make surgeries more accurate.
It also makes patients safer by letting surgeons quickly address issues. This proactive approach can lead to faster recovery and lower morbidity rates.
In conclusion, intraoperative diagnosis is essential in modern surgery. It offers big benefits in decision-making, patient outcomes, and safety. Its ongoing development will continue to improve surgical care quality.
Surgical decisions get better with intraoperative diagnostic techniques. These methods let doctors check and change plans during surgery. This helps patients get better results.
Frozen section analysis is a key tool in surgery. It gives quick info on tissue samples. This is very helpful in cancer surgery to check if all cancer is removed.
Key steps in frozen section analysis include:
Cytological examination looks at single cells or small groups. It’s great for spotting cancer or infections. Methods like fine-needle aspiration cytology (FNAC) and touch imprint cytology are used.
Cytological examination is beneficial due to its:
Rapid immunohistochemistry (IHC) finds specific proteins in tissues during surgery. It’s key for finding cancer markers and where tumors come from.
The table below summarizes the primary characteristics of the discussed intraoperative diagnostic procedures:
|
Diagnostic Procedure |
Key Features |
Applications |
|---|---|---|
|
Frozen Section Analysis |
Rapid histopathological examination |
Tumor surgery, margin assessment |
|
Cytological Examination |
Minimally invasive, rapid diagnosis |
Malignancy assessment, infection diagnosis |
|
Rapid Immunohistochemistry |
Specific antigen detection |
Tumor marker identification, metastatic tumor origin |
In conclusion, intraoperative diagnostic procedures like frozen section analysis, cytological examination, and rapid immunohistochemistry are vital. They help doctors make better decisions during surgery. Knowing these methods is key for better patient care and outcomes.
In surgical pathology, frozen section diagnosis is the top choice for quick diagnosis during surgery. It gives surgeons the info they need right away. This helps them make smart choices while they operate.
The process of frozen section diagnosis is detailed. First, a sample is taken from the patient and frozen quickly. Then, it’s cut into thin slices and stained with special dyes.
A pathologist looks at these slices under a microscope. They make a diagnosis based on what they see.
The method needs skill and precision. Pathologists must be good at reading these frozen slices. This can be hard because of the freezing and cutting process.
Key steps in the technical process include:
Frozen section diagnosis has many benefits. It gives doctors the info they need right away. This is very important for making decisions during surgery.
It’s very useful in cancer surgery. It helps check if all cancer cells are removed and if there are any spread.
But, it also has some downsides. The quality of the frozen slices can be bad because of freezing issues. It also takes a lot of resources and trained people.
The main strengths and limitations are summarized as follows:
|
Strengths |
Limitations |
|---|---|
|
Real-time diagnostic information |
Freezing artifacts complicating diagnosis |
|
Critical for surgical decision-making |
Resource-intensive, requiring specialized equipment |
|
Valuable in oncological surgery |
Need for trained personnel |
Intraoperative pathology services are key in today’s surgery. They give vital info that helps surgeons make decisions.
Pathologists are vital to the surgical team. They work with surgeons and others to get accurate and quick diagnoses.
Pathologists do many important jobs in the operating room. They include:
Good communication is key for intraoperative pathology services. It’s between pathologists, surgeons, and other healthcare pros.
This means clear reports of findings and teamwork. Everyone needs to be informed and on the same page.
The perks of good intraoperative pathology services are:
Pathologists and surgeons working together and talking well can give patients the best care during surgery.
New technologies are changing how we diagnose during surgery. These advancements make diagnoses more accurate, faster, and reliable.
Digital pathology uses digital slides to analyze tissue samples. It allows for remote diagnosis, improving intraoperative pathology services. Telepathology lets pathologists give expert opinions in real-time, even if they’re not in the room.
Key benefits of digital pathology and telepathology include:
Artificial intelligence (AI) and machine learning (ML) are being used more in intraoperative diagnosis. They quickly analyze data, find patterns, and suggest diagnoses. AI helps pathologists spot abnormalities and make more accurate diagnoses.
Some possible uses of AI and ML in intraoperative diagnosis include:
Advanced imaging like fluorescence and optical coherence tomography (OCT) are improving intraoperative diagnosis. These methods give real-time info on tissue, helping surgeons make better decisions.
Examples of advanced imaging modalities include:
As these technologies improve, they will greatly impact intraoperative diagnosis. This will lead to better patient outcomes and more efficient surgeries.
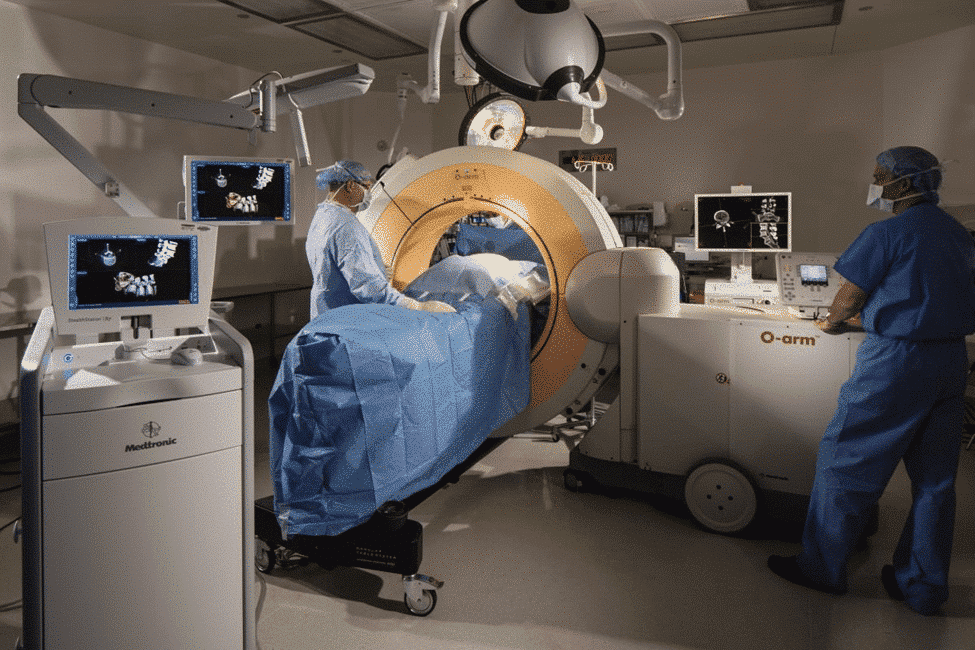
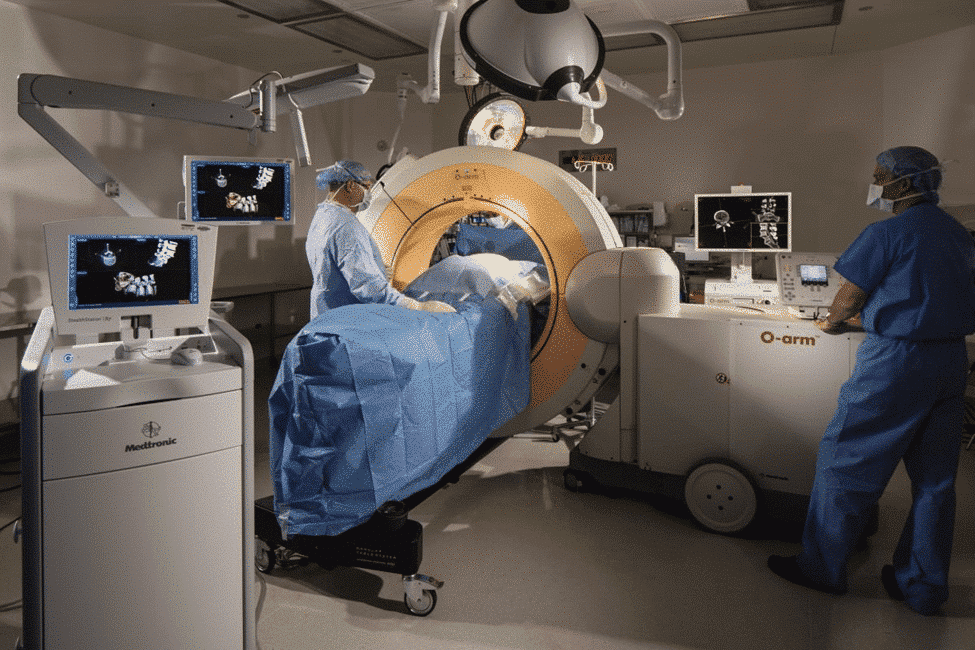
Advanced intraoperative monitoring systems have changed surgery for the better. They make surgeries safer and more successful. These systems use cutting-edge tech to watch important body functions as they happen during surgery.
Neurophysiological monitoring is key in surgeries that touch the nervous system. It uses electroencephalography (EEG), electromyography (EMG), and somatosensory evoked potentials (SSEP) to keep an eye on the brain and nerves. It helps spot any problems or damage.
Keeping an eye on the heart and blood flow is vital during surgery. Tools like invasive blood pressure monitoring, cardiac output measurement, and transesophageal echocardiography (TEE) help. They let doctors and surgeons make smart choices about fluids and heart support.
These monitoring tools make surgeries safer and more effective. They help improve how well patients do after surgery.
Effective intraoperative tissue diagnosis needs advanced biopsy techniques and rapid tissue processing protocols. These are key for quick and accurate diagnoses during surgery.
Intraoperative tissue diagnosis uses many techniques for fast and accurate results. Key parts are biopsy methods and the best ways to sample tissues.
Biopsy techniques are very important in intraoperative tissue diagnosis. The right biopsy method depends on the tissue type, where it is, and the situation.
Choosing the best sampling strategy is key to get a tissue sample that truly shows the condition. This needs careful planning and doing by the surgical team.
Rapid tissue processing protocols aim to give quick diagnostic info without losing accuracy. These steps are part of the process:
By using advanced biopsy techniques and quick tissue processing, intraoperative tissue diagnosis can greatly improve surgical decisions and patient results.
Intraoperative diagnosis is key in many surgical fields. It makes surgeries more precise and effective. Each specialty has its own needs and challenges.
In oncology, knowing how much tumor to remove is vital. Frozen section analysis helps check if all tumor is gone.
This method is essential for removing tumors fully. It also helps save important body parts, improving patient results.
Neurosurgery faces special challenges in diagnosing tumors. Advanced imaging and intraoperative MRI help a lot.
Tools like intraoperative neurophysiological monitoring are also key. They help keep brain function safe during surgery.
In transplant surgery, checking the donor organ’s health is critical. This includes looking at its condition and spotting any problems.
Quickly examining biopsy samples gives surgeons important info. It helps them decide if the organ is good for transplant.
Intraoperative diagnostic assessment is key but faces many hurdles. The complexity of surgeries and the need for quick decisions make it high-stakes. Getting the diagnosis right is critical.
Pathologists and surgeons work under time pressure during surgeries. They need to make quick diagnoses. But, they often face resource constraints due to limited skilled staff and tools.
Managing these issues well is vital. It ensures fast, accurate diagnoses. A coordinated team and the latest tech are essential.
Accuracy concerns are a big challenge. Any mistake in diagnosis can have serious consequences. Diagnostic pitfalls like sampling errors or misreading data can lead to wrong diagnoses.
To avoid these, quality control is key. Diagnostic teams must be well-trained to handle intraoperative diagnosis complexities.
Intraoperative diagnosis needs strong quality assurance to keep results accurate. These steps help make sure what’s found during surgery is right.
Quality assurance in intraoperative diagnosis has several parts. Validation and verification are key to checking if results are correct. Validation checks if a test always gives the same results. Verification makes sure the test is done right.
Validation and verification are key to accurate intraoperative results. They check if diagnostic tools and methods work right. This is done by testing and reviewing them often.
|
Methodology |
Description |
Frequency |
|---|---|---|
|
Equipment Calibration |
Regular calibration of diagnostic equipment to ensure accuracy |
Daily/Weekly |
|
Proficiency Testing |
Evaluation of diagnostic personnel to ensure proficiency |
Quarterly |
|
Quality Control Checks |
Regular checks to ensure diagnostic equipment is functioning correctly |
Daily |
Stopping systematic errors is also important for intraoperative diagnosis. These strategies find and fix error sources before they happen.
Some ways to prevent systematic errors include:
With these quality assurance steps, healthcare can make sure intraoperative results are accurate. This helps improve patient care.
Professional training is key to making intraoperative diagnostic procedures better. These procedures are complex and critical, needing thorough training. This ensures pathologists and surgical teams can make accurate and timely diagnoses.
Pathologists’ education and training are the base for good intraoperative diagnosis. They must study and train a lot to be experts. Each country has its own rules for certification, but it usually involves education and a professional exam.
In the U.S., pathologists need to finish a residency in pathology. They might also get extra training through fellowships. The American Board of Pathology offers a certification in anatomic pathology, which is vital for intraoperative diagnosis.
The whole surgical team must be trained for intraoperative diagnostic procedures. This includes surgeons, nurses, and others who are key in diagnosis. Multidisciplinary team training programs help improve teamwork and decision-making in surgery.
Simulation training is a great tool for team training. It lets teams practice in a safe space. This training helps teams work better together during real surgeries.
Good intraoperative diagnostic procedures come from a well-trained team. With strong training programs, healthcare can improve patient care and quality.
Surgical technology is getting better, making the ethics of real-time diagnosis more important. This immediacy brings up complex ethical issues. These issues affect how we care for patients and make surgical decisions.
One big ethical worry is informed consent. Patients need to know the risks and benefits of real-time diagnosis during surgery. But, the fast pace of intraoperative diagnosis makes it hard to fully inform patients beforehand.
Healthcare providers must find a way to balance quick diagnosis with respecting patient rights. This might mean talking to patients before surgery about possible intraoperative diagnosis. They should explain the risks and benefits.
Another key ethical issue is dealing with diagnostic uncertainty and error. Intraoperative diagnosis isn’t perfect, and mistakes can happen. Surgeons and pathologists must handle these situations carefully to avoid harming patients.
Managing uncertainty means being open with patients and their families about possible errors. It’s also about having a clear plan to check diagnostic results and adjust surgery plans if needed.
Handling uncertainty and error ethically is vital for keeping patient trust. It shows the importance of a team effort. This team should include surgeons, pathologists, ethicists, and patient advocates.
The field of intraoperative diagnostic technologies is changing fast. This is thanks to new molecular and genetic testing methods. These changes are making it easier for doctors and pathologists to diagnose and treat patients during surgery.
New molecular and genetic testing methods are changing how we diagnose in the operating room. Techniques like rapid PCR and next-generation sequencing are now used during surgery. They allow for quick genetic analysis of tumor samples.
This helps doctors make more precise treatment plans. For example, genetic tests can show specific mutations. This information helps doctors choose the best treatments for each patient.
There’s a big trend of combining intraoperative diagnostic technologies with precision medicine. Precision medicine means treatments are tailored to each patient’s needs. This combination helps doctors make better decisions during surgery.
In cancer surgery, knowing the tumor’s genetics is key. It helps doctors decide how much to remove. Precision medicine lets them balance removing the tumor with saving healthy tissue.
Research and clinical trials are always improving intraoperative diagnostic technologies. Scientists are looking into using artificial intelligence and machine learning to improve diagnosis. These tools can quickly analyze complex data, helping doctors make decisions.
There are also trials on new diagnostic biomarkers and advanced imaging in surgery. These studies are important for making sure new tech is safe and works well in real-world settings.
Intraoperative diagnosis is changing healthcare. It’s important for providers to know its economic side. This approach affects how care is given and patient results.
Doing a cost-benefit analysis is key for intraoperative diagnosis. It looks at costs and benefits. Costs include setting up services, while benefits are better patient care and lower costs later.
Intraoperative diagnosis adds a lot of value, mainly in complex surgeries. It helps make better decisions and care plans. This can lead to fewer surgeries and shorter hospital stays, saving money.
Integration Challenges in Various Healthcare Systems
Adding intraoperative diagnosis to healthcare systems is tough. It needs special gear, trained people, and changes to how things work. These issues differ a lot, from big hospitals to small ones.
To integrate well, planning is needed. This includes checking current setup, finding problems, and solving them. It might mean buying new tech, training staff, and setting clear rules for using intraoperative diagnosis.
Understanding intraoperative diagnosis’s economic side helps healthcare providers. They can tackle integration challenges and make it work for patients and the system.
Intraoperative diagnosis is a key tool that helps surgeons make better decisions during surgery. It uses methods like frozen section analysis and rapid immunohistochemistry. This way, surgeons can make informed choices during procedures.
This technique is important because it allows for quick diagnosis during surgery. It helps surgeons adjust their plans as needed. This can make surgery safer and reduce complications.
As we move forward, new technologies like digital pathology and artificial intelligence will play a big role. These advancements will help improve surgical outcomes and patient care.
In summary, intraoperative diagnosis is vital in today’s surgery. Its growth will be essential for the future of surgical diagnosis and real-time diagnosis.
It’s key in modern surgery because it lets surgeons make smart choices right away. This can lead to better results and fewer extra surgeries.
Main types include frozen section analysis, cytological examination, and rapid immunohistochemistry. Each has its own uses and benefits.
Frozen section diagnosis quickly freezes a tissue sample. Then, it’s cut and examined under a microscope for a fast diagnosis during surgery.
Pathologists are vital in intraoperative diagnosis. They interpret tissue samples and share their findings with the surgical team quickly.
New tech like digital pathology, telepathology, AI, and advanced imaging makes intraoperative diagnosis more accurate and efficient.
Challenges include time pressure, limited resources, accuracy worries, and pitfalls. These can affect the reliability of the diagnosis.
Quality is ensured through validation, verification, and error prevention strategies. This keeps the diagnosis accurate and reliable.
Pathologists need specialized training, including education and certification. The surgical team also needs training for effective procedures.
New trends include molecular and genetic testing, integration with precision medicine, and ongoing research and trials.
Costs and benefits need to be weighed, along with healthcare value. Integration challenges also play a role in different healthcare systems.
It can greatly improve patient outcomes by allowing surgeons to make quick, informed decisions. This can make surgeries more effective and reduce the need for more procedures.
It’s significant because it allows for quick tissue sample examination during surgery. This gives vital information for making surgical decisions.
It helps in oncological surgery by quickly checking tumor margins and identifying cancerous tissues. This can lead to better surgical outcomes.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8570863/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!