Did you know that nearly 80% of surgical complications can be avoided with advanced imaging during operations? Intraoperative MRI (iMRI) is changing surgery by giving real-time images. This makes complex surgeries more precise and successful. Learn what is an intraoperative MRI scan. Understand the purpose of imaging done during surgery clearly.
Magnetic Resonance Imaging (MRI) used during surgery lets surgeons check their work and adjust as needed. This is very helpful in brain surgeries and removing tumors, where being exact is key.
Key Takeaways
- Intraoperative MRI enhances surgical precision.
- Real-time imaging improves surgical outcomes.
- iMRI is very useful in brain surgery.
- The technology lets surgeons make changes right away during surgery.
- It helps lower the chance of problems during surgery.
Understanding Intraoperative MRI Technology
Intraoperative MRI (iMRI) is a key tool in today’s surgery. It gives surgeons real-time images, making operations more precise. This tech combines MRI’s power with the urgency of the operating room.
Definition and Basic Principles
Intraoperative MRI uses MRI tech during surgery to show images of the brain or other areas. It works like regular MRI, but it’s made for the operating room. It uses a strong magnetic field and radio waves to create detailed images.
The key to iMRI’s effectiveness is its ability to give surgeons instant feedback. This is very important in neurosurgery. The brain’s complex anatomy needs precise navigation to avoid damage.
How Intraoperative MRI Differs from Standard MRI
Standard MRI machines are for diagnosis in a controlled setting. But iMRI systems work in the operating room’s dynamic environment. They need specialized surgical instruments and changes to the MRI machine for better access and efficiency.
iMRI also works with other surgical tools and navigation systems. This lets surgeons make real-time decisions. They can adjust their techniques based on the latest images.
Intraoperative MRI is a big step forward in surgery. It could lead to better results by making surgeries more precise and effective.
The Evolution of Intraoperative MRI Systems
Intraoperative MRI technology has seen big changes over the years. From its start to today’s advanced systems, it’s a story of constant innovation and growth.
Historical Development
The idea of using MRI in surgery came from the growth of MRI in medicine. The first intraoperative MRI systems came out in the late 1990s. They were the start of a new time in surgery.
These early systems were low-field, showing the tech limits of the time. But as MRI tech got better, so did iMRI systems. The early 2000s brought higher field strength systems. These improved image quality and opened up more uses for iMRI in surgery.
Key Technological Milestones
Several key tech milestones have shaped iMRI systems. A big step was moving from low-field to high-field iMRI systems. High-field systems, at 1.5 Tesla or higher, give better image quality. This helps with more precise surgery.
Improvements in magnetic field generation and image tech have also been key. Today’s iMRI systems can make high-quality images in real-time. This lets surgeons make better choices during complex surgeries.
Adding iMRI to other surgical tools, like neuronavigation systems, has also helped. This mix makes surgeries more accurate and efficient.
|
Technological Advancement |
Impact on iMRI |
Year Introduced |
|---|---|---|
|
High-Field iMRI Systems |
Improved image quality and expanded surgical applications |
Early 2000s |
|
Advanced Magnetic Field Generation |
Enhanced real-time imaging capabilities |
Mid-2000s |
|
Integration with Neuronavigation Systems |
Increased precision and efficiency in surgical procedures |
Late 2000s |
The evolution of intraoperative MRI systems shows how fast medical tech is moving. As iMRI keeps getting better, it will play a bigger role in surgery. This will help patients and change surgery’s future.
How Intraoperative MRI Works
Intraoperative MRI combines advanced magnetic field generation with top-notch imaging software. This combo creates high-quality images right as they happen. It lets surgeons make key decisions during complex surgeries.
Technical Components of iMRI Systems
iMRI systems have several important parts for real-time imaging. These include a high-field magnet, gradient coils, radiofrequency coils, and advanced computers for image processing.
The high-field magnet is key. It creates the strong magnetic field needed for MRI imaging. The field strength can vary, with some systems stronger than others.
Magnetic Field Generation and Image Production
The magnetic field generation is at the heart of MRI tech. When a patient is in the MRI machine, the strong magnetic field lines up hydrogen nuclei in their body. Radiofrequency pulses then disturb these nuclei, creating signals that the MRI system uses to make images.
The image quality depends on several things. These include the magnetic field strength, the complexity of the gradient coils, and the sensitivity of the radiofrequency coils.
Real-Time Imaging Capabilities
iMRI’s biggest plus is its real-time imaging. This lets surgeons see how the surgery is going and adjust as needed. Real-time imaging is super useful in surgeries where the body’s layout changes, like in brain surgery.
Being able to see updates in real-time makes surgeries more precise. It can also lead to better patient outcomes by lowering the chance of complications.
Types of Intraoperative MRI Systems
Intraoperative MRI technology has evolved into different types for various surgical needs. These systems differ in magnetic field strength, mobility, and how they fit into operating rooms.
Low-Field vs. High-Field Systems
Intraoperative MRI systems are mainly divided into low-field and high-field types. Low-field systems have a magnetic field strength under 0.5 Tesla. They are often cheaper and easier to add to existing operating rooms. Yet, they might not have the same image quality as high-field systems.
High-field iMRI systems, with a field strength of 1.5 Tesla or more, offer better image quality. This is key for detailed surgeries. A study in the Journal of Neurosurgery showed high-field iMRI improves tumor removal rates in neurosurgery.
|
Characteristics |
Low-Field iMRI |
High-Field iMRI |
|---|---|---|
|
Magnetic Field Strength |
Less than 0.5 Tesla |
1.5 Tesla or higher |
|
Image Quality |
Lower |
Higher |
|
Cost |
Generally lower |
Higher |
Mobile vs. Fixed Installation Systems
iMRI systems differ in their mobility. Mobile systems can be moved in and out of the operating room. This flexibility can save costs. Fixed systems, on the other hand, are built into the operating room for constant access to MRI.
A surgical team noted, “The mobility of certain iMRI systems allows us to use MRI in multiple operating rooms. This optimizes our surgical workflow.”
Integrated Operating Room Solutions
Integrated operating room solutions are a new approach to iMRI. They fully integrate the MRI scanner into the operating room. These systems use advanced technologies for real-time decision-making during surgeries.
Integrating iMRI into the operating room improves surgical precision and patient outcomes. A report found that hospitals with integrated iMRI solutions see fewer repeat surgeries.
Applications in Neurosurgery
iMRI has greatly improved neurosurgery by making surgeries more precise and successful. It gives surgeons real-time images, helping them perform better.
Brain Tumor Resection
iMRI is key in removing brain tumors. It lets surgeons see the tumor and healthy tissue clearly as they work. This is vital because the difference between tumor and healthy tissue is very small.
Benefits of iMRI in Brain Tumor Resection:
- Improved tumor visualization
- Enhanced precision in tumor removal
- Reduced risk of damaging surrounding brain tissue
Deep Brain Stimulation
Deep Brain Stimulation (DBS) involves placing electrodes in the brain. iMRI helps place these electrodes correctly, leading to better results.
iMRI’s precision in DBS has greatly helped patients with Parkinson’s disease and other movement disorders.
Epilepsy Surgery
iMRI is also important in epilepsy surgery. It helps surgeons find and remove the part of the brain causing seizures. This real-time imaging lets them make changes during the surgery, increasing the chance of success.
iMRI has many uses in neurosurgery and is getting more. Here’s a table showing some key points about iMRI in these surgeries:
|
Procedure |
Role of iMRI |
Benefits |
|---|---|---|
|
Brain Tumor Resection |
Real-time tumor visualization |
Improved precision, reduced risk to surrounding tissue |
|
Deep Brain Stimulation |
Guiding electrode placement |
Enhanced accuracy, improved patient outcomes |
|
Epilepsy Surgery |
Identifying and resecting epileptogenic zone |
More accurate resection, improved surgical outcomes |
Intraoperative MRI in Other Surgical Specialties
iMRI is now used in many surgical fields, changing how surgeries are done. It’s not just for neurosurgery anymore. It’s being used in other important areas too.
Spinal Surgery Applications
In spinal surgery, iMRI is a big help. It lets doctors see images in real time during tough surgeries. This can make surgeries more precise and might help patients heal better.
iMRI helps in spinal surgery by:
- Finding the exact spot of problems
- Watching how the surgery is going
- Spotting any issues right away
ENT Procedures
In ENT surgery, iMRI is being looked at for better results. It’s useful for detailed surgeries in the head and neck. It gives doctors real-time feedback.
Using iMRI in ENT surgery can:
- Show tumor edges more clearly
- Help with precise work in tricky spots
- Maybe cut down on needing to do surgeries again
Emerging Applications in Other Fields
iMRI is also being checked out for other surgeries. It’s being looked at for:
- Orthopedic surgery, like removing tumors or fixing bones
- Small, less invasive surgeries where seeing images in real time helps
- Cancer surgeries where checking tumor edges is key
As iMRI gets better, it will be used in even more surgeries. The benefits of seeing images during surgery are huge. More research will likely find new ways to help patients.
Benefits and Advantages of Intraoperative MRI
MRI technology in the operating room has changed how we do surgery. Intraoperative MRI (iMRI) systems are key in modern surgery. They offer many benefits that greatly improve surgical results.
Improved Surgical Precision
iMRI makes surgery more precise by showing images in real-time. Surgeons can adjust their work as needed. This ensures they remove the right tissues and avoid harming important areas. Real-time imaging reduces the chance of problems and boosts surgeon confidence.
Enhanced Tumor Resection Rates
iMRI helps remove tumors more effectively. It lets surgeons see how much tumor they’ve removed right away. This is very important in brain surgery, where the goal is to remove as much tumor as possible without harming the brain.
Reduced Need for Reoperation
iMRI’s real-time images mean fewer second surgeries. Surgeons can check their work during the operation. This avoids the need for more surgeries, which is good for patients and saves money.
Impact on Patient Outcomes
The benefits of iMRI add up to better patient results. Studies show iMRI leads to fewer complications and better survival rates. Patients often recover faster and have better long-term health when surgery uses iMRI.
|
Benefit |
Description |
Impact |
|---|---|---|
|
Improved Surgical Precision |
Real-time imaging during surgery |
Reduced complications, improved surgical confidence |
|
Enhanced Tumor Resection Rates |
Immediate feedback on tumor removal |
More complete resections during initial surgery |
|
Reduced Need for Reoperation |
Verification of procedure completeness during surgery |
Avoidance of additional surgeries, reduced healthcare costs |
|
Impact on Patient Outcomes |
Better postoperative results |
Reduced morbidity and mortality, faster recovery times |
The Role of Intraoperative MRI in Image-Guided Surgery
Intraoperative MRI is key in image-guided surgery. It gives surgeons real-time feedback. This technology makes surgeries more precise and effective.
Integration with Neuronavigation Systems
iMRI works with neuronavigation systems for better brain structure localization. This combo helps surgeons navigate complex anatomy. It leads to better surgical results.
Real-Time Surgical Decision Making
iMRI helps with real-time surgical decision-making. It gives surgeons up-to-date images during surgery. This lets them adjust the surgery as needed, possibly avoiding extra surgeries.
Compensating for Brain Shift
Brain shift is a big challenge in neurosurgery. It happens when the brain moves during surgery, making preoperative images less accurate. iMRI fixes this by showing current images. This ensures the surgical team has the most accurate info.
iMRI is a big step forward in neurosurgery. It brings better precision, outcomes, and safety for patients.
Challenges and Limitations
Intraoperative MRI technology has many benefits but also faces big challenges. The complexity and high cost of iMRI systems are major hurdles for many hospitals.
Cost and Resource Considerations
Buying an iMRI system is very expensive. It includes the initial cost and ongoing maintenance and upgrades. There are also indirect costs. Hospitals need special equipment and shielded rooms for iMRI. This adds to the financial strain.
Increased Operative Time
Using iMRI in surgery makes operations longer. Moving the patient, scanning, and then starting surgery again takes more time. A study in the Journal of Neurosurgery found this extra time is significant.
This longer surgery time can lead to more anesthesia time. It also raises the risk of complications. It affects the surgical team’s efficiency too.
Technical Challenges in the OR Environment
The OR is a tough place for iMRI systems. Making sure surgical tools and equipment work with the MRI is key.
“The presence of ferromagnetic materials in the OR can interfere with the MRI scanner, posing significant technical challenges.”
Also, MRI systems need to work fast and accurately during surgery. They must provide clear images without slowing down the operation.
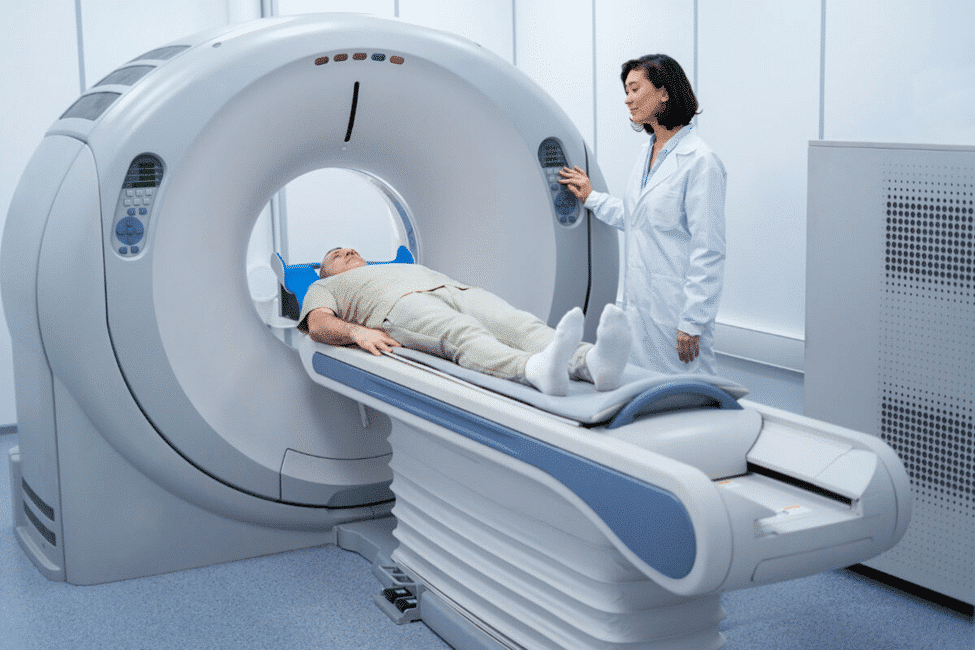
The Intraoperative MRI Procedure: What Patients Can Expect
For those facing surgery with intraoperative MRI, knowing what to expect can ease worries. The process has several stages aimed at top-notch care and precision.
Pre-Surgical Preparation
Before surgery, patients go through a detailed prep. This includes a full medical history check, lab tests, and talks with the surgical team. They’re also told about any changes to their meds and other steps to take.
Anesthesia Considerations
Anesthesia for intraoperative MRI is special. The anesthesia team works with the surgeons to keep the patient safe and comfy. Using MRI-safe anesthesia gear is key.
The Surgical Environment
The operating room is set up for the MRI system. It has the MRI, monitoring, and surgical tools. The team is trained to work well in this setup, making the surgery smooth.
Post-Procedure Recovery
After surgery, patients go to a recovery area for close monitoring. The recovery time depends on the surgery and the patient’s health. They get clear instructions on care and follow-up visits.
Knowing about the intraoperative MRI procedure can make a big difference. Being informed helps patients prepare for surgery and recovery.
The Surgical Team and Intraoperative MRI
Intraoperative MRI needs a skilled and coordinated surgical team. The team must know the tech and the surgery under MRI. This is key for iMRI procedures.
Specialized Training Requirements
The team needs specialized training for iMRI. This includes MRI safety, using the tech, and reading images during surgery. It’s a big part of the job.
“The use of iMRI has changed surgery a lot,” says a top neurosurgeon. “But training the team is a big change too.”
Team Composition and Roles
The composition of the surgical team is very important for iMRI. The team needs experts in MRI, surgery, and patient care under MRI. Everyone knows their role to keep things running smoothly and safe.
- Surgeons trained in iMRI techniques
- Anesthesiologists experienced in managing patients during MRI scans
- Nurses knowledgeable about MRI safety and patient care
- Radiological technicians skilled in operating iMRI equipment
Communication and Coordination
Effective communication is key for the team during iMRI. They need to work together well. This is because surgery under MRI is always changing.
Good communication is very important. It keeps the surgery safe and effective. The team should have clear briefings and know their roles well.
Safety Considerations for Intraoperative MRI
Intraoperative MRI (iMRI) has changed surgery a lot. But, it needs careful safety rules. The iMRI room is special and needs extra care to keep everyone safe.
MRI-Compatible Surgical Instruments
Using MRI-safe surgical tools is key in iMRI. Normal tools can fly around in a strong magnetic field, which is very dangerous. MRI-compatible instruments are made to be safe in the MRI room, reducing the chance of metal problems.
- Instruments are made from non-ferromagnetic materials.
- They undergo rigorous testing to ensure compatibility.
- The use of MRI-compatible instruments is mandatory in iMRI procedures.
Patient Monitoring During Scanning
Keeping an eye on the patient is very important during iMRI. Special equipment that works with MRI is used to watch the patient’s health. This helps keep the patient safe and gets good MRI pictures.
Key aspects of patient monitoring include:
- Vital sign monitoring (e.g., heart rate, blood pressure).
- Anesthesia management.
- Continuous observation of the patient’s condition.
Staff Safety Protocols
Keeping staff safe is very important in iMRI rooms. People working there need special training. They must know the dangers of MRI and how to stay safe.
Safety protocols for staff include:
- Screening for ferromagnetic objects before entering the MRI suite.
- Understanding emergency procedures.
- Regular training on MRI safety.
Managing Ferromagnetic Risks
Keeping metal risks low is a big deal in iMRI rooms. This means controlling what goes into the MRI area very carefully.
- Ferromagnetic detection systems.
- Strict access controls.
- Regular audits of equipment and supplies.
Following these safety steps helps make sure iMRI rooms are safe for patients and staff.
Future Directions in Intraoperative MRI Technology
Intraoperative MRI technology is on the verge of big changes. New innovations are set to change how iMRI systems work. These changes will make iMRI systems better in many ways.
Emerging Technological Innovations
One big change is the use of advanced imaging. High-field iMRI systems are becoming more common. They give better images and help surgeons be more precise.
A top neurosurgeon says “The future of iMRI is in real-time, high-quality images during surgery.” More surgeons are using iMRI because of its benefits.
“The future of iMRI lies in its ability to provide real-time, high-resolution imaging during complex surgical procedures.”
Integration with Other Imaging Modalities
iMRI is also getting better by working with other imaging tools. Adding intraoperative ultrasound or fluorescence-guided surgery gives surgeons a clearer view. This mix can make surgeries more accurate and better for patients.
|
Imaging Modality |
Benefits |
Potential Applications |
|---|---|---|
|
iMRI + Intraoperative Ultrasound |
Real-time imaging, enhanced tissue differentiation |
Brain tumor resection, spinal surgery |
|
iMRI + Fluorescence-Guided Surgery |
Improved visualization of tumor margins |
Oncological surgeries, neurosurgery |
Artificial Intelligence Applications
Artificial intelligence (AI) will be key in iMRI’s future. AI can quickly analyze images, giving surgeons important info. It could help with things like finding tumors and predicting surgery results.
Miniaturization and Mobility Improvements
There’s a push to make iMRI systems smaller and more mobile. Portable iMRI could make advanced surgery options available to more places. This could help more people get better care.
The future of intraoperative MRI looks bright. With new tech coming, surgeries will likely be more precise, safe, and effective.
Conclusion: The Evolving Role of Intraoperative MRI in Modern Surgery
Intraoperative MRI has become a key tool in modern surgery. It boosts precision and improves outcomes in many surgical areas. Its role is growing because it offers real-time imaging, helping doctors make better decisions and care for patients.
As iMRI technology gets better, it’s being used in more surgeries, like spinal and ENT procedures. It’s also being combined with other imaging and artificial intelligence. This will make it even more useful.
iMRI is important because it makes surgeries more precise. It also cuts down on the need for second surgeries. As it keeps improving, it will likely become even more central to surgery’s future.
FAQ
What is intraoperative MRI, and how does it differ from standard MRI?
Intraoperative MRI (iMRI) is a special kind of MRI used during surgery. It gives real-time images. Unlike standard MRI, it’s made for use in the operating room, helping surgeons adjust as needed.
What are the benefits of using intraoperative MRI in neurosurgery?
Using iMRI in neurosurgery boosts precision and improves tumor removal rates. It also means fewer follow-up surgeries. This leads to better patient outcomes by ensuring tumors are fully removed.
How does intraoperative MRI work, and what are its technical components?
iMRI uses a strong magnetic field and radio waves to show body structures. It has a magnet, gradient coils, and a radiofrequency coil. These work together to create clear images in real-time.
What are the different types of intraoperative MRI systems available?
There are low-field and high-field systems, as well as mobile and fixed installations. Some systems are integrated with other technologies, like neuronavigation systems, to improve surgery.
Is intraoperative MRI used in surgical specialties beyond neurosurgery?
Yes, iMRI is used in spinal surgery and ENT procedures too. It’s also being explored in orthopedic and general surgery.
What are the challenges and limitations of using intraoperative MRI?
Using iMRI can be costly and time-consuming. It also poses technical challenges in the OR. Ensuring patient and staff safety is a top priority.
What can patients expect during an intraoperative MRI procedure?
Patients will prepare for surgery and may need anesthesia. They’ll be in a special OR with iMRI. Their recovery will be closely monitored.
What role does the surgical team play in intraoperative MRI procedures?
The surgical team is key in iMRI procedures. They need special training and must work well together. Good communication is essential for success.
What safety considerations are essential for intraoperative MRI?
Safety is critical with iMRI. This includes using MRI-safe tools and monitoring patients. Staff must follow safety protocols and manage risks to prevent accidents.
What is the future of intraoperative MRI technology?
The future of iMRI looks bright. New technologies, integration with other imaging, and AI are on the horizon. Improvements in miniaturization and mobility are also expected.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/9316044/



































