Surgery is a lifesaving medical intervention but comes with risks. Over 230,000 surgical complications are reported annually in the United States alone. This shows the importance of knowing the risks of different surgeries.
Laparoendoscopic surgeons, experts in minimally invasive surgeries, are key in managing these risks. This guide will explore the top 3 riskiest surgeries. It will also explain the factors that increase surgical risk and how skilled surgeons reduce these risks.
Key Takeaways
- Understanding the risks of different surgeries is vital for patient safety.
- The top 3 riskiest surgeries are identified based on complication rates and complexity.
- Laparoendoscopic surgeons use advanced, minimally invasive techniques to reduce risks.
- Surgical risk is influenced by many factors, including patient health and surgical expertise.
- This guide offers insights into effectively navigating surgical risks.
Understanding Surgical Risk
Knowing the risks of surgery is key to making smart health choices. Surgical risk is the chance of problems or bad outcomes from a surgery. We’ll look at how risks are checked and what factors play a part.
How Surgical Risk is Measured
There are many ways to measure surgical risk. One method is using a surgical risk calculator. It looks at patient and surgery details to guess the risk of problems. This tool helps doctors and patients see the risks and benefits of a surgery.
Common Risk Factors in Surgery
Many things can affect surgical risk. These include the patient’s health, the surgery type, and the doctor’s experience. Age, health, and existing medical conditions are key for patients. The surgery’s complexity and type also matter.
| Risk Factor | Description | Impact on Surgical Risk |
| Age | Older patients may have higher risks due to decreased physical reserve and comorbidities. | Increased risk of complications and longer recovery times. |
| Pre-existing Conditions | Conditions such as diabetes, heart disease, and lung disease can increase surgical risk. | Higher risk of complications, including infection and cardiovascular events. |
| Surgical Complexity | More complex surgeries, such as neurosurgery or cardiothoracic surgery, carry higher risks. | Increased risk of complications and longer recovery times. |
Knowing these risk factors is very important. It helps doctors and patients plan better. This way, they can lower risks and improve surgery outcomes.
Factors That Determine Surgical Risk
Surgical risk comes from many factors. These include the patient’s health, how complex the procedure is, and the hospital’s expertise. Knowing these helps us understand the risk of surgery.
Patient-Related Factors
Patient health is key in determining surgical risk. This includes the patient’s overall health, age, and any health conditions they have. For example, people with diabetes or heart disease face higher risks during and after surgery. We look at these factors to create a risk assessment for each patient.
Procedure-Related Factors
The type of surgery also affects the risk. More complex surgeries, like neurosurgery or cardiothoracic surgery, are riskier than simpler ones. The surgery’s length and technical difficulty also play a part in the risk.
Hospital and Surgeon Experience
The experience of the hospital and surgical team is very important. Hospitals that do a lot of a certain surgery tend to have better results. This is because the team is more skilled and has better processes. Also, surgeons with lots of experience in a procedure can lower the risk of problems. We stress the importance of choosing a hospital and surgeon with a good track record in the needed procedure.
How Surgical Risk is Calculated
Calculating surgical risk involves looking at many factors. These include the patient’s health and the type of surgery. It’s key to assess these risks well to improve patient care and make smart surgery choices.
Doctors use tools like surgical risk calculators and risk-benefit analysis to figure out risks. These tools help understand the chances of problems or death after surgery.
Surgical Risk Calculators
Surgical risk calculators are online tools that give risk estimates based on patient data. They look at:
- Patient age and health
- Existing medical conditions
- The type of surgery
- The surgeon’s experience and the hospital’s quality
By using these calculators, doctors can better understand the risks involved.
Risk-Benefit Analysis
A risk-benefit analysis weighs the risks of surgery against its benefits. It considers the patient’s health, symptoms, and surgery outcomes.
This analysis helps patients and doctors decide if surgery is right. It also helps find ways to lower risks and improve results.
Important parts of a risk-benefit analysis are:
- Looking at the patient’s condition
- Checking the surgery’s benefits
- Identifying possible risks and complications
- Exploring other treatment options
By examining these factors, doctors can give patients a clear view of surgery risks and benefits.
The Role of Laparoendoscopic Surgeons in High-Risk Procedures
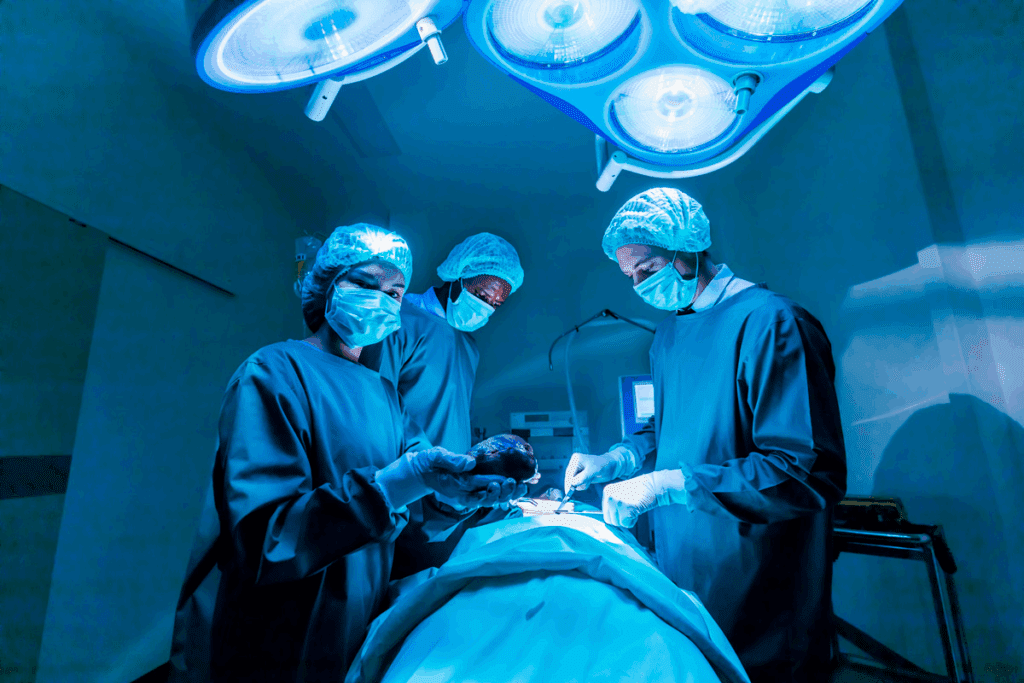
Laparoendoscopic surgeons are key in high-risk surgeries. They use advanced techniques and precision. They get special training to handle complex surgeries.
Specialized Training and Expertise
Laparoendoscopic surgeons get specialized training. They learn both laparoscopic and endoscopic techniques. This skill lets them tackle surgeries from different angles.
High-risk surgeries need more than just technical skills. They also need to know about patient anatomy and possible problems. Laparoendoscopic surgeons are great at dealing with complex surgeries. They are very important in the operating room.
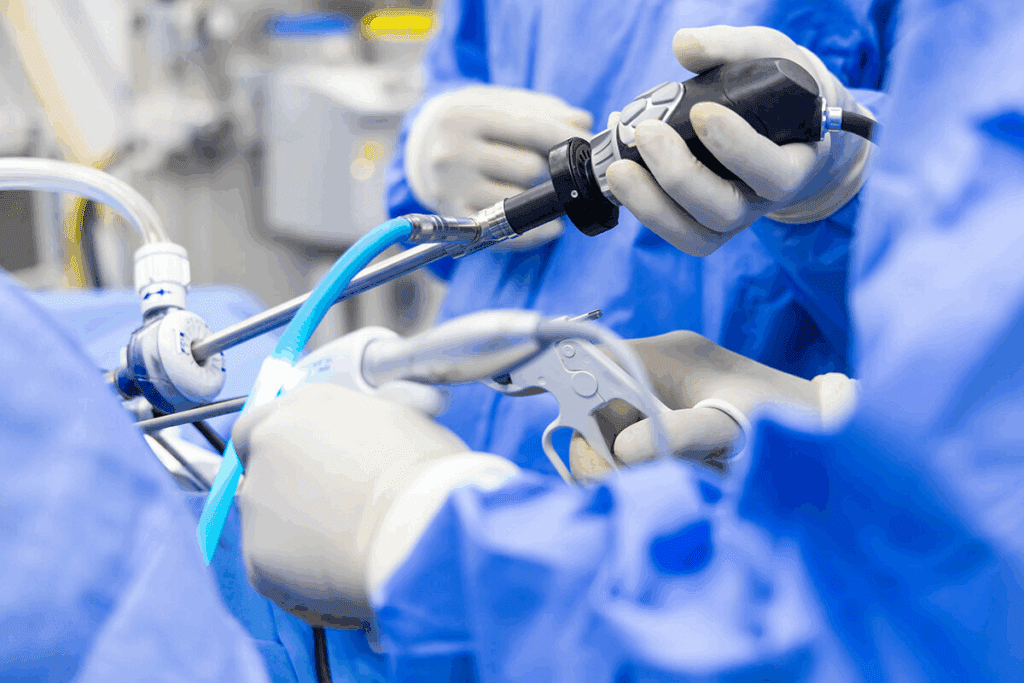
Minimizing Risks Through Advanced Techniques
Laparoendoscopic surgery is minimally invasive. This makes it safer than open surgery. Surgeons use new tools and methods to lower risks and improve results.
They use tools for better vision, precise cutting, and small incisions. These methods help patients recover faster and have fewer complications.
The role of laparoendoscopic surgeons is not just about technical skills. They also understand patient care and managing risks well.
Risky Surgery #1: Craniectomy for Traumatic Brain Injury
Craniectomy for traumatic brain injury is a very risky surgery. It’s complex and can lead to severe complications. This surgery removes part of the skull to let a swollen brain expand. It helps reduce pressure inside the skull.
Why This Surgery is High-Risk
Craniectomy is high-risk for several reasons. It’s often done quickly, when patients are in critical condition. This rush can limit time for detailed planning.
The surgery is also complex, dealing with delicate brain tissue and important blood vessels. Patients often have other serious injuries or health issues. These can make the surgery and recovery even riskier.
Mortality and Complication Rates
Mortality rates for this surgery are high, showing how serious the initial injury and surgery risks are. Studies show mortality rates from 15% to over 30%. Complications like infection, swelling, and fluid buildup in the brain are common.
Complication rates vary based on the patient, the injury’s severity, and the surgery and care received. But, it’s clear that craniectomy for traumatic brain injury is very risky.
Recovery and Long-Term Outcomes
Recovery from this surgery is long and hard. Patients need a lot of rehabilitation to regain lost functions. The outcomes can vary, with some recovering well and others facing lasting disabilities.
Many factors affect long-term outcomes. These include the injury’s severity, the patient’s age and health, and the quality of care and rehabilitation. Despite the challenges, better neurosurgery, intensive care, and rehabilitation have helped many patients.
Brain Surgery: Types and Associated Risks
Brain surgery is a complex field that requires great skill and precision. It’s a key part of neurosurgery, aimed at treating brain-related issues. We’ll look at the different types of brain surgery and their risks.
Brain Tumor Resection
Brain tumor resection is a surgery to remove brain tumors. The complexity of the surgery is influenced by the size, location, and type of the tumor. It’s a risky procedure because surgeons must carefully move through the brain to reach the tumor. Risks include infection, bleeding, and damage to nearby brain tissue.
Doctors decide on this surgery after carefully checking the patient and the tumor. New imaging and surgical tools have made this surgery safer.
Cerebral Aneurysm Repair
Cerebral aneurysm repair is a complex surgery for brain aneurysms. An aneurysm is a bulge in a blood vessel that can burst. The surgery aims to stop the aneurysm from bursting or bleeding again. It can be done through clipping or coiling.
Risks include vasospasm, hydrocephalus, and possible brain damage. The choice between clipping and coiling depends on the aneurysm’s location and the patient’s health.
Brain Surgery Survival Rates
Survival rates for brain surgery vary based on the surgery type, patient condition, and other factors. For brain tumor resection, survival chances are better for benign tumors. For cerebral aneurysm repair, surgery before rupture improves survival rates.
It’s important for patients and families to know the risks and possible outcomes of brain surgery. We provide personalized care and support during the surgery process.
Risky Surgery #2: Open Heart Surgery
Open heart surgery is very risky because it’s so invasive. It’s done on the heart or big blood vessels near it. The surgeon has to open the chest to do it.
Coronary Artery Bypass Grafting (CABG)
CABG helps blood flow to the heart by bypassing blocked arteries. It’s for those with severe heart disease. A graft from another part of the body is used to bypass the blockage.
Key aspects of CABG include:
- Relieving symptoms of angina
- Reducing the risk of heart attack
- Improving survival in certain patient groups
Valve Replacement Surgery
Valve replacement surgery fixes a faulty heart valve. It’s needed when a valve doesn’t work right. The choice of valve depends on age, lifestyle, and health.
The decision to undergo valve replacement surgery is typically made when:
- The valve disease is severe and symptomatic
- Other treatments have failed or are not suitable
- The risks of surgery are outweighed by the benefits
Complications and Mortality Rates
CABG and valve replacement surgeries have big risks. Complications and death can happen. The risk depends on health, age, and other conditions. Common issues include bleeding, infection, stroke, and heart attack.
Mortality rates for open heart surgery vary:
- The overall mortality rate for CABG is around 2-3%
- For valve replacement surgery, the mortality rate can range from 3-5%
- These rates can be higher for patients with significant comorbidities or those undergoing emergency surgery
Knowing these risks is key for patients and families. It helps them decide about open heart surgery. We’ll look at more in the next sections.
Cardiac Surgery: Advancements and Challenges
Cardiac surgery is getting better, thanks to new technologies. These advancements have made complex surgeries safer. But, there are also challenges we need to face.
Technological Innovations Reducing Risk
New technologies have changed cardiac surgery. Some key innovations include:
- Robotic-assisted surgery: It makes surgery more precise and cuts down recovery time.
- 3D printing: It helps plan surgeries better and creates models for each patient.
- Advanced imaging techniques: They give detailed views of the heart.
- Minimally invasive techniques: They reduce the need for big cuts and help patients heal faster.
These new tools have made surgery safer and more possible for more people. Even those at high risk can now get help.
Patient Selection for High-Risk Cardiac Procedures
Choosing the right patients is key for success in high-risk surgeries. A detailed check is needed to find who will benefit most from surgery.
Important things to consider include:
- Comprehensive medical history: Knowing the patient’s health and past heart issues.
- Current health status: Looking at the patient’s current health and any other health problems.
- Cardiac function: Checking how well the heart is working and if it can handle surgery.
- Potential for recovery: Guessing how well the patient will do after surgery and in the long run.
By choosing wisely and using new technologies, we can keep making cardiac surgery better. Even for the toughest cases.
Risky Surgery #3: Separation of Conjoined Twins
Separating conjoined twins is a very complex and risky surgery. It needs a team of experts, like surgeons, anesthesiologists, and neonatologists. They work together to make sure the twins are okay.
Unique Challenges and Complexities
Separating conjoined twins is very hard. They can be connected at different parts of their bodies. This can be the head, chest, abdomen, or pelvis.
The surgery’s complexity depends on how and where they are connected. It also depends on if they share vital organs.
Some big challenges include:
- They might share vital organs like the heart or liver, which need careful separation.
- Their complex anatomy requires detailed planning and imaging before surgery.
- A coordinated team is needed to manage their vital signs and handle any problems.
Historical Success Rates
In the past, separating conjoined twins was very risky. But, thanks to new surgical methods, imaging, and care, outcomes have gotten better.
Some successes include:
- Advances in separating craniopagus twins, who are connected at the head.
- Better survival rates for twins sharing vital organs, thanks to better planning and surgery.
Ethical Considerations
There are many ethical questions about separating conjoined twins. These include deciding if separation is possible, the risks and benefits, and the twins’ quality of life after surgery.
Some ethical issues are:
- When separation is very risky for one or both twins.
- When they share vital organs, making separation dangerous.
- Thinking about the twins’ autonomy and life quality after being separated.
As medical professionals, we must think deeply about these issues. We need to talk a lot with the twins’ families to make good decisions.
Other High-Risk Surgical Procedures
There are many surgeries that are considered high-risk. These include complex procedures that can have serious complications. They need skilled surgeons and a dedicated care team to manage risks and ensure the best results.
Partial Hepatectomy (Liver Resection)
Partial hepatectomy, or liver resection, involves removing part of the liver. It’s often done to remove tumors or damaged liver tissue. The liver’s role in the body and its complex blood vessels make this surgery challenging.
Risks include bleeding, infection, and liver failure. But the liver can grow back, which helps. The surgery requires careful technique and post-operative care.
| Risks | Complications | Precautions |
| Bleeding | Hemorrhage | Careful surgical technique |
| Infection | Sepsis | Prophylactic antibiotics |
| Liver Failure | Reduced liver function | Monitoring liver function |
Esophagectomy
Esophagectomy removes part or all of the esophagus, often for esophageal cancer. The surgery is complex because of the esophagus’s location and its closeness to important structures.
“The complexity of esophagectomy requires a multidisciplinary approach to minimize risks and improve patient outcomes.”
Risks include leakage, respiratory problems, and trouble swallowing. Advanced techniques and post-operative care are key to managing these risks.
Pancreaticoduodenectomy (Whipple Procedure)
The Whipple procedure removes the head of the pancreas, the duodenum, and nearby tissues. It’s mainly for pancreatic cancer or other pancreas issues.
Risks include infection, delayed gastric emptying, and pancreatic fistula. The surgery’s complexity demands a skilled team and thorough post-operative care.
Experts say, “The Whipple procedure is a tough operation. It needs precise technique and post-operative management to reduce complications.”
| Surgery | Major Risks | Survival Rate |
| Partial Hepatectomy | Bleeding, Infection | 70-90% |
| Esophagectomy | Leakage, Respiratory issues | 50-60% |
| Whipple Procedure | Infection, Pancreatic fistula | 80-90% |
What Makes a Surgery “Difficult to Perform”
Several factors make a surgery hard to do. These include technical complexity, anatomical variations, and the physical and mental demands on the surgeon. It’s important for both doctors and patients to understand these challenges.
Technical Complexity
Technical complexity means the surgery needs special skills and tools. It might require minimally invasive techniques or real-time imaging. These are examples of complex surgeries.
Also, surgeries that need teams of specialists are more complex. This teamwork is key for success and safety.
Anatomical Challenges
Anatomical challenges happen when a patient’s body is different from the usual. For example, if organs are not in the right place. Surgeries on complex anatomical structures need a deep understanding of these differences.
Previous surgeries, trauma, or disease can make things even harder. Surgeons must adjust their methods to succeed.
Time Constraints and Surgeon Fatigue
Long surgeries can be very hard on surgeons. They can get tired and make mistakes. Surgeon fatigue can slow them down and affect their skills.
To avoid these problems, teams might change surgeons during long operations. They also try to make the operating room a better place to work.
Most Painful Surgeries and Recovery
Some surgeries are very painful and hard to recover from. The pain and recovery time can vary. This depends on the surgery type, the patient’s health, and post-operative care.
Pain Management Strategies
Managing pain well is key to better patient outcomes and fewer complications. We use several methods to control pain, including:
- Multimodal Analgesia: Mixing different pain medicines for better control.
- Regional Anesthesia: Giving anesthesia directly to the surgery area.
- Patient-Controlled Analgesia (PCA): Letting patients give themselves pain relief as needed.
These methods help reduce pain and make recovery better for patients.
Surgeries with Difficult Recovery Periods
Some surgeries are harder to recover from because of their complexity. They affect sensitive areas of the body. Examples include:
- Thoracic Surgeries: Chest surgeries are very painful because of the area’s sensitivity.
- Orthopedic Surgeries: Joint replacement surgeries are tough to recover from.
- Neurosurgeries: Brain or spine surgeries need careful care and have complex recoveries.
Knowing these challenges helps us prepare patients better. We tailor our care to meet their specific needs.
By understanding the pain and recovery challenges, we can improve patient care. We aim to reduce these issues and help patients recover better.
The Financial Cost of High-Risk Surgeries
High-risk surgeries are not just health risks. They also have big financial costs. It’s important for patients and families to understand these costs in the complex healthcare world.
Insurance Coverage for Risky Procedures
Insurance is key in reducing the financial stress of high-risk surgeries. Most plans cover major surgeries. But, how much they cover can differ a lot.
We’ll look into insurance for high-risk surgeries. We’ll see what’s usually covered and what might change coverage.
Cost Comparison of Major Surgeries
The cost of major surgeries changes based on several things. These include the surgery type, the surgeon’s fees, and the hospital’s charges.
| Surgery Type | Average Cost | Insurance Coverage |
| Craniectomy | $100,000 – $200,000 | 80% – 90% |
| Open Heart Surgery | $150,000 – $300,000 | 80% – 90% |
| Separation of Conjoined Twins | $200,000 – $500,000 | 70% – 90% |
The table shows the high costs of high-risk surgeries. Even with insurance, there can be big out-of-pocket costs.
When thinking about high-risk surgery, we must consider these financial aspects. It’s part of weighing the surgery’s risks and benefits.
How to Prepare for a High-Risk Surgery
When you’re facing a high-risk surgery, getting ready is key. It helps reduce anxiety and improves recovery. Being prepared is essential for the surgery’s success.
Questions to Ask Your Surgeon
Talking openly with your surgeon is a must. Asking the right questions can clear up doubts. Here are some important ones:
- What are the possible risks and complications?
- What are the expected results, and how will success be measured?
- Are there other options instead of surgery?
- How will pain be managed during and after the surgery?
- What’s the expected recovery time, and what care will be needed after?
A famous surgeon once said,
“The key to a successful surgery lies not just in the operation itself, but in the complete care given before, during, and after.”
Second Opinions and Hospital Selection
Getting a second opinion is a smart move. It offers more insights and confidence in your treatment plan. When picking a hospital, look at:
- The hospital’s experience with the surgery you need.
- The skills and qualifications of the surgical team.
- The quality of care in the ICU and after surgery.
Choosing a hospital that does many similar surgeries can greatly improve your chances. Research shows better results and lower death rates at high-volume centers.
Physical and Mental Preparation
Getting physically ready is vital for surgery. This includes:
- Improving any health issues you have.
- Boosting nutrition to aid healing.
- Doing exercises as advised to get stronger.
Mental preparation is also key. Meditation, counseling, and support groups can help with anxiety. Having a strong support system is vital for emotional support during surgery.
By thoroughly preparing for a high-risk surgery, you can greatly improve your chances of success. It’s about making a detailed plan for your medical, emotional, and practical needs.
The Future of High-Risk Surgeries
The future of high-risk surgeries is changing fast. New tech in robotic surgery and AI is leading the way. We’re seeing big changes in how complex surgeries are done.
Robotic Surgery and AI Assistance
Robotic surgery has changed the game. It gives surgeons better precision and control. Adding AI makes it even better, helping surgeons make smarter choices.
AI in robotic surgery brings many benefits. For example:
- It makes surgeries more accurate and cuts down on mistakes
- It offers better views and analyzes data in real-time
- It can spot problems before they happen
AI can look at a patient’s past, current health, and surgery data. It can then predict issues and suggest fixes.
Personalized Risk Assessment
Technology is also changing how we assess risks. Advanced data and AI help us give more accurate, personalized risk assessments. This is key for high-risk surgeries.
Personalized risk assessment includes:
- Genetic tests to find genetic risks
- Deep looks at a patient’s medical history
- Monitoring vital signs during surgery
By focusing on each patient’s needs, we can make surgeries safer and more effective. This approach improves outcomes for everyone.
Conclusion: Balancing Risks and Benefits in Surgical Decision-Making
Certain surgeries come with risks that need careful consideration. The top three riskiest surgeries include craniectomy for traumatic brain injury, open heart surgery, and separation of conjoined twins. These complex procedures require detailed planning and skill.
Laparoendoscopic surgeons are key in helping patients make these tough decisions. They offer specialized training and expertise. This helps reduce risks and improve results. Understanding what affects surgical risk is important for making informed choices.
It’s all about finding the right balance between risks and benefits. Working with experienced surgeons and healthcare teams is essential. This way, patients can face high-risk surgeries with confidence and achieve the best results.
FAQ
What are the riskiest surgeries?
Some risky surgeries include craniectomy for brain injury, open heart surgery, and separating conjoined twins. These surgeries are complex and risky. But, the risk level can change based on the individual case.
How is surgical risk measured?
Risk in surgery is measured with tools like risk calculators and analysis. These look at the patient’s health, the surgery type, and the surgeon’s and hospital’s experience.
What factors determine surgical risk?
Risk in surgery comes from patient health, the surgery type, and the surgeon’s and hospital’s experience. Knowing these factors helps both patients and doctors make better choices.
What is the role of laparoendoscopic surgeons in high-risk procedures?
Laparoendoscopic surgeons are key in high-risk surgeries. Their training and skills help reduce risks with new techniques. This improves patient results.
How can I prepare for a high-risk surgery?
To get ready for a high-risk surgery, ask your surgeon questions and think about getting a second opinion. Choose your hospital wisely. Physical and mental prep can also help you face surgery’s challenges.
What are the most painful surgeries?
Painful surgeries often involve a lot of tissue damage or trauma. Examples are open heart surgery or spinal surgery. Good pain management can make recovery easier.
How much do high-risk surgeries cost?
High-risk surgery costs vary by procedure, location, and insurance. Knowing your insurance and comparing prices can help you decide.
What is the future of high-risk surgeries?
High-risk surgeries might see advancements in robotic surgery, AI, and personalized risk assessment. These could lead to better outcomes and lower risks.
How can I minimize risks during surgery?
To lower surgery risks, choose carefully, do thorough checks before surgery, and use the latest techniques. Experienced surgeons, like laparoendoscopic ones, are key in reducing risks.
What are the survival rates for brain surgery?
Brain surgery survival rates depend on the procedure, the condition, and the patient. Knowing the risks and benefits helps patients make informed choices.
What are the complications of open heart surgery?
Open heart surgery can lead to complications like bleeding, infection, and heart rhythm problems. Talking about these risks with your doctor can prepare you for the surgery.
References
Centers for Disease Control and Prevention. Riskiest surgeries A laparoendoscopic perspective. Retrieved from https://www.cdc.gov/mmwr/volumes/73/wr/mm7303a3.htm










