Last Updated on October 21, 2025 by mcelik
Blood cancer, also known as hematologic cancer, affects thousands of people worldwide. Recent medical advancements have significantly improved the leukemia survival rate. This offers new hope to patients and their families. A notable study highlighted the successful treatment of a patient with a severe infection after undergoing a haploidentical allo-HSCT. This showcases the progress in medical treatments.
We are witnessing a transformative era in the treatment of blood cancer. Different types of cancer require different approaches. Understanding the curability of blood cancer is key for patients to make informed decisions about their care. The question of whether leukemia is curable depends on several factors, including the type and stage of the disease.
Key Takeaways
- Advances in medical treatments have improved the blood cancer survival rate.
- The curability of blood cancer depends on its type and stage.
- Understanding treatment options is key for patients.
- Recent studies highlight the effectiveness of innovative treatments.
- Patients should consult healthcare professionals to determine the best course of treatment.
What Is Blood Cancer? Types and Characteristics
Blood cancer, also known as hematologic malignancy, affects the blood, bone marrow, and lymphatic system. Understanding the different types of blood cancer is key to finding the right treatment.
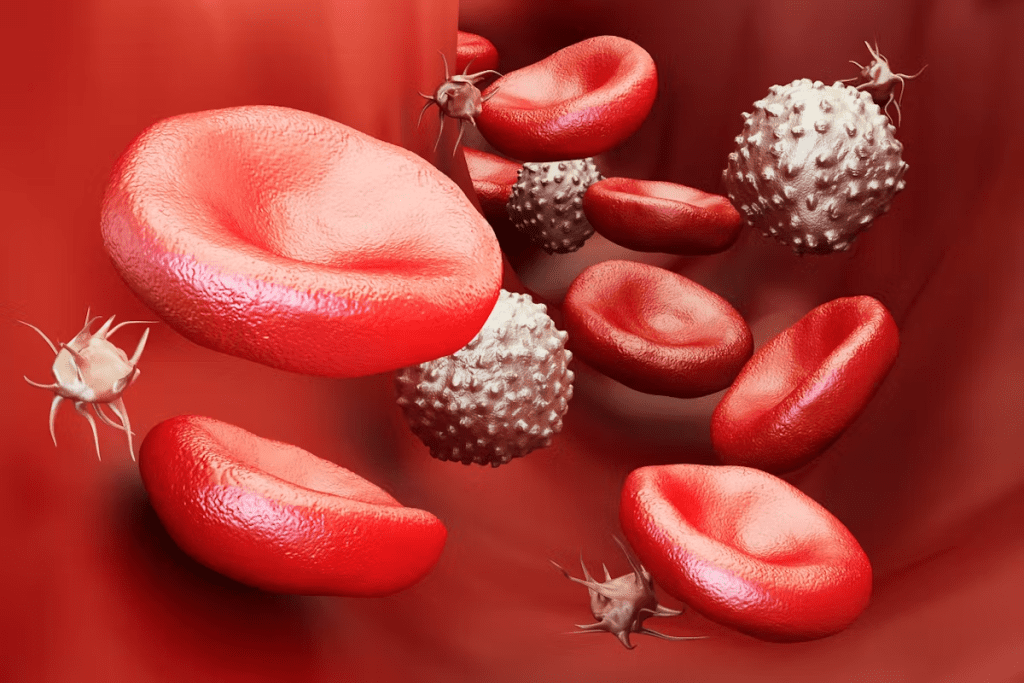
Definition and Development of Blood Cancer
Blood cancer happens when the bone marrow makes abnormal blood cells. Normally, the bone marrow makes healthy blood cells. But in blood cancer, it makes bad cells that don’t work right and take over.
These bad cells can be lymphoid or myeloid. Lymphoid cells turn into lymphocytes, important for the immune system. Myeloid cells turn into red blood cells and platelets. Blood cancer starts with genetic changes that mess up these cell production.
Major Types: Leukemia, Lymphoma, and Myeloma
The main types of blood cancer are leukemia, lymphoma, and myeloma. Leukemia is when the bone marrow makes too many white blood cells. Lymphoma is cancer in the lymphatic system, found in lymph nodes and the spleen. Myeloma is when plasma cells in the bone marrow make too many bad proteins.
How Hematologic Malignancies Differ from Solid Tumors
Hematologic malignancies are different from solid tumors. Solid tumors are a mass in one place. But hematologic malignancies spread through the blood or lymphatic system. This makes them harder to treat than solid tumors.
Blood Cancer Prevalence and Demographics
Blood cancer statistics show a complex picture. We’ll look at the current state of blood cancer in the U.S. We’ll see who’s most affected and how we’re raising awareness.
Current Statistics in the United States
In the U.S., many people are diagnosed with blood cancer each year. Leukemia, lymphoma, and myeloma are the most common types. Leukemia is a big part of these cases, with different forms affecting different ages. The American Cancer Society gives us important insights into these numbers.
Risk Factors and Vulnerable Populations
Some groups are more at risk for blood cancer. Age is a big factor, with risk going up as people get older. Chemicals, radiation, and genetics also play a role. Knowing these factors helps us understand who’s most at risk.
Acute myeloid leukemia (AML) is common in older adults. Acute lymphoblastic leukemia (ALL) is the top cancer in kids. Knowing these differences helps us develop better treatments.
Blood Cancer Awareness Month Initiatives
September is Blood Cancer Awareness Month. We come together to raise awareness about blood cancers. Many initiatives happen during this month to educate, support, and fund research.
We join in with awareness campaigns, fundraising, and educational programs. Our goal is early detection and better treatments. It’s a team effort involving patients, families, healthcare providers, and the community.
Recognizing Blood Cancer: Symptoms and Diagnosis
Spotting the signs of blood cancer early can greatly improve treatment chances and survival rates. Blood cancer, which includes leukemia, lymphoma, and myeloma, shows symptoms that are often not clear. These symptoms can be similar to those of other illnesses.
Common Warning Signs of Blood Cancer
The symptoms of blood cancer vary by type and stage. Common signs include:
- Persistent fatigue or weakness
- Frequent infections
- Unexplained weight loss
- Swollen lymph nodes or spleen
- Bone pain or tenderness
- Easy bruising or bleeding
These symptoms can be vague. They might not immediately point to blood cancer. It’s key to notice body changes and see a doctor if symptoms last or worsen.
Diagnostic Procedures and Tests
Diagnosing blood cancer involves physical exams, medical history, and tests. Important tests include:
- Blood Tests: Complete Blood Count (CBC) to check for abnormal blood cells.
- Bone Marrow Biopsy: To look for cancer cells in the bone marrow.
- Imaging Tests: CT scans, MRI, or PET scans to see how far the disease has spread.
- Genetic Tests: To find specific genetic changes linked to blood cancer.
These tests help doctors find out if you have blood cancer, what type, and how far it has spread. This info is vital for planning treatment.
The Importance of Early Detection
Finding blood cancer early is key to better treatment and survival. Early diagnosis means more treatment options and a chance for some types of blood cancer to be cured. Knowing the symptoms and risk factors can lead to quicker medical help.
We know how a blood cancer diagnosis affects patients and their families. Early detection leads to better medical results. It also gives patients more treatment choices and a better life during and after treatment.
How Curable Is Blood Cancer? Factors Affecting Prognosis
The outlook for blood cancer patients depends on many factors. Knowing these factors helps doctors choose the best treatments. This improves how well patients do. We’ll look at what makes blood cancer curable, focusing on different types and their chances of recovery.
Curability by Cancer Type
Blood cancer includes leukemia, lymphoma, and myeloma, each with its own treatment path. Leukemia is a fast-growing cancer of blood and bone marrow. Its cure rate changes based on whether it’s acute or chronic.
Genetic and Molecular Factors
Genetics and molecular factors greatly influence blood cancer prognosis. Some genetic changes can make the disease more aggressive or harder to treat. For example, in chronic lymphocytic leukemia (CLL), certain genes can show how likely the disease will get worse.
Age and Overall Health Considerations
A patient’s age and health are key to their prognosis. Older people might face a tougher time due to less energy and health issues. Younger patients usually do better because they can handle stronger treatments.
Stage at Diagnosis Impact
The cancer’s stage at diagnosis is very important. Being diagnosed early means a better chance of treatment success. But, if the cancer is advanced, treatment is harder and the outlook is less hopeful.
Understanding these factors helps both patients and doctors make better choices. This leads to better results for those with blood cancer.
Leukemia Survival Rate: Current Statistics and Trends
Medical research has made big strides in improving leukemia survival rates. This brings hope to those fighting the disease. It’s key to know what affects these rates.
Overall 5-Year Survival Rates
The 5-year survival rate is a key measure for leukemia. In the U.S., it’s about 65% for leukemia patients. This number has gone up over the years. Thanks to better treatments and early detection.
Acute vs. Chronic Leukemia Survival Differences
Leukemia is split into acute and chronic types. Each has its own survival rate. Acute leukemia, which moves fast, has a 5-year survival rate of about 40% for ALL and 30% for AML in adults.
Chronic leukemia, which moves slower, has a 5-year survival rate of about 70% for CLL and 65% for CML. These numbers show why early diagnosis and specific treatments are so important.
Leukemia Survival Rate by Age and Type
Age and type of leukemia greatly affect survival rates. For example, kids with ALL have a 5-year survival rate over 90%. But adults over 65 with AML have a much lower rate, around 10%.
Knowing these numbers helps doctors tailor treatments. This can improve outcomes.
- Children with ALL: Over 90% 5-year survival rate
- Adults with AML: Around 30% 5-year survival rate
- Adults over 65 with AML: Around 10% 5-year survival rate
Improvements in Survival Over Time
Leukemia survival rates have gotten better over time. This is thanks to new treatments like targeted therapies and immunotherapies. More research and trials are needed to keep improving survival rates and quality of life for leukemia patients.
As we look ahead, keeping up with the latest stats and treatments is vital. This ensures the best care for those with leukemia.
Lymphoma and Myeloma: Survival Rates and Curability
It’s important to know the survival rates and curability of lymphoma and myeloma. These blood cancers have different characteristics and treatment outcomes. So, it’s key to look closely at their prognosis.
Hodgkin vs. Non-Hodgkin Lymphoma Prognosis
Lymphoma is divided into Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL). Each has its own survival rates. Hodgkin lymphoma is very curable, mainly when caught early.
The 5-year survival rate for HL is about 85%, recent stats show. NHL’s survival rate varies, from 70% to 90%. This depends on the type and stage at diagnosis.
- Hodgkin Lymphoma: High cure rate with proper treatment.
- Non-Hodgkin Lymphoma: Survival varies by type and stage.
Multiple Myeloma Survival Statistics
Multiple myeloma is a blood cancer with malignant plasma cells in the bone marrow. Survival stats for multiple myeloma have gotten better in the last decade. This is thanks to new treatments.
The 5-year survival rate for multiple myeloma is now about 50%. This is a big jump from before. Survival depends on the stage, age, and how well the patient responds to treatment.
- Early diagnosis and treatment start.
- New treatments.
- Patient’s health and age.
Bone Marrow Cancer Survival Rate
Bone marrow cancer, like multiple myeloma and leukemia, has seen better survival rates. This is thanks to better treatment plans. Survival rates vary a lot, depending on the cancer type, stage, and patient factors.
For example, survival for multiple myeloma has gotten better, as mentioned before. Other bone marrow cancers also have better treatment options now. This means better outcomes for patients.
We keep seeing progress in treating lymphoma and myeloma. This gives hope for better survival rates and quality of life for patients.
Conventional Treatment Approaches for Blood Cancer
It’s important for patients and doctors to know about blood cancer treatments. Blood cancer includes leukemia, lymphoma, and myeloma. Each needs a treatment plan that fits the disease type and stage.
Chemotherapy Success Rates and Protocols
Chemotherapy is key in treating blood cancers. Its success depends on the cancer type, stage, and the patient’s health. For example, chemotherapy works well for acute lymphoblastic leukemia (ALL) in children.
Chemotherapy protocols aim to kill fast-growing cancer cells. The choice of drugs and treatment length are key. We keep improving these plans to get better results with fewer side effects.
Radiation Therapy Applications
Radiation therapy is used for some blood cancers, like lymphoma. It uses high-energy rays to kill or slow cancer cells. The treatment depends on the cancer’s location and spread.
In some cases, radiation therapy helps with symptoms like pain or breathing trouble. It’s often used with chemotherapy to make treatments more effective.
Targeted Drug Therapies
Targeted drug therapies are a big step forward in blood cancer treatment. They aim at specific molecules in cancer cells, reducing harm to healthy cells. For example, tyrosine kinase inhibitors help with chronic myeloid leukemia (CML), and monoclonal antibodies treat certain lymphomas.
The creation of targeted therapies has led to better patient outcomes. By focusing on cancer’s molecular traits, we can offer treatments that are more precise and less harmful.
Treatment Selection Criteria
Choosing the right treatment for blood cancer involves many factors. These include the cancer type and stage, the patient’s age and health, and the cancer’s genetic or molecular traits. A team of healthcare experts works together to find the best treatment plan.
The main goal is to offer a treatment that works well for the patient. This should also help keep their quality of life good.
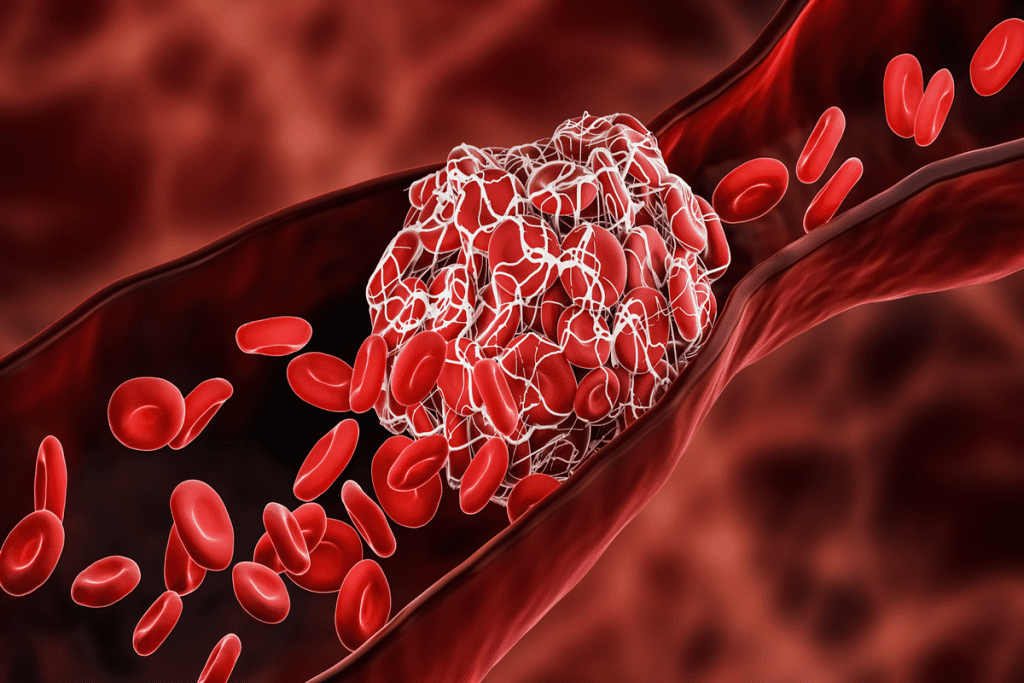
Stem Cell Transplantation and Bone Marrow Therapy
For many patients with blood cancer, stem cell transplantation is a hopeful treatment. This method replaces damaged bone marrow with healthy stem cells. It helps the body make normal blood cells again.
Autologous vs. Allogeneic Transplants
There are two main types of stem cell transplants: autologous and allogeneic. Autologous transplants use the patient’s own stem cells. These are collected, stored, and then given back after chemotherapy. This method lowers the risk of GVHD but might increase the chance of cancer coming back.
Allogeneic transplants use stem cells from a donor. This can help fight cancer with the donor’s immune cells. But, it carries a higher risk of GVHD and needs careful donor matching.
Transplant Success Rates by Cancer Type
The success of stem cell transplantation depends on the blood cancer type. For example:
- For multiple myeloma, autologous stem cell transplantation is often used, with significant improvements in survival rates.
- In acute leukemia, allogeneic transplantation can be curative, when a suitable donor is available.
- Lymphoma patients may benefit from either autologous or allogeneic transplants, depending on their specific disease characteristics and overall health.
Donor Matching and Availability
For allogeneic transplants, finding a suitable donor is key. Donors are matched based on HLA typing. The availability of a matched donor greatly affects transplant success.
We are seeing better donor matching techniques and alternative donor sources. This includes haploidentical donors (half-matched family members) and umbilical cord blood units. These advancements are making allogeneic transplantation more accessible.
Post-Transplant Care and Recovery
After stem cell transplantation, patients need careful monitoring and supportive care. This is to manage complications like infections, GVHD, and organ toxicity. The recovery process can take several months to a year or more for the immune system to fully recover.
We stress the importance of a detailed post-transplant care plan. This includes regular check-ups, medication management, and lifestyle adjustments. These steps support long-term health and well-being.
Immunotherapy: Revolutionizing Blood Cancer Treatment
Immunotherapy is changing the game in blood cancer treatment. It uses the body’s immune system to fight cancer. This method is more targeted and less toxic than old treatments.
CAR T-Cell Therapy Success Stories
CAR T-cell therapy is a big win for blood cancer, like acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL). It changes T-cells to attack cancer cells. This has led to high remission rates in trials.
- High Response Rates: Some studies show response rates up to 90% in certain groups.
- Durable Remissions: Many patients stay disease-free for years.
- Ongoing Research: Trials are ongoing to make CAR T-cell therapy better and use it for more cancers.
Monoclonal Antibodies in Blood Cancer
Monoclonal antibodies are also promising for blood cancer. They’re made to target cancer cells, helping the immune system destroy them.
For example, rituximab and obinutuzumab have helped patients with lymphoma.
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors help the immune system fight cancer better. They’re new in blood cancer but show promise for lymphoma and other cancers.
Combination Immunotherapy Approaches
Researchers are mixing different immunotherapies to make treatments better. They’re trying CAR T-cell therapy with checkpoint inhibitors or monoclonal antibodies.
Clinical Trials and Emerging Treatments
The world of blood cancer treatment is changing fast. Many clinical trials and new therapies are showing great promise. It’s important to know about these new directions and options.
Promising Research Directions
Researchers are looking into several promising areas. These include:
- Immunotherapy combinations: Mixing different immunotherapies to make them work better.
- Targeted therapies: Creating drugs that only harm cancer cells, not healthy ones.
- Precision medicine: Treating each patient based on their unique genetic makeup.
Gene Therapy for Blood Cancers
Gene therapy is a new and exciting way to treat blood cancers. It changes a patient’s genes to fight cancer better. Key parts of gene therapy include:
- CAR T-cell therapy: Changing T-cells to find and kill cancer cells.
- Gene editing: Using CRISPR to fix genes and remove cancer-causing mutations.
How to Access Experimental Treatments
If you want to try experimental treatments through clinical trials, here’s what to do:
- Consult with your healthcare provider: Talk to your doctor about if you’re a good fit and what options you have.
- Search clinical trial databases:Look for studies on .
- Contact research centers: Get in touch with big cancer research places or those running trials.
Evaluating Clinical Trial Opportunities
When thinking about joining a clinical trial, it’s key to think it over. Consider things like:
- Trial phase: Knowing if the trial is in its early or later stages.
- Potential risks and benefits: Thinking about the possible good and bad outcomes.
- Eligibility criteria: Making sure you meet the trial’s specific needs.
By keeping up with clinical trials and new treatments, blood cancer patients can make better choices. They might even get to try the latest therapies.
Remission vs. Cure: What Patients Should Understand
The terms ‘remission’ and ‘cure’ are often used in blood cancer treatment. But what do they really mean for patients? Understanding these concepts is key for patients and their families. We will look at the differences between remission and cure and their impact on survival and quality of life.
Defining Complete Remission
Complete remission means there’s no detectable cancer in the body after treatment. Tests like blood counts, bone marrow biopsies, and imaging studies confirm this. Reaching complete remission is a big win in blood cancer treatment, showing the disease is controlled.
When Is Blood Cancer Considered “Cured”?
The idea of a “cure” is more complex. It means the cancer won’t come back, and the patient can live a normal life. For some blood cancers, staying in complete remission for a while can be considered a cure. But it depends on the cancer type, its aggressiveness, and the patient’s health.
Monitoring for Relapse
Even in complete remission, regular check-ups are key to watch for relapse. This includes blood tests and sometimes bone marrow biopsies. Early detection and treatment are possible through monitoring.
Long-term Survival Considerations
Surviving long-term with blood cancer means more than just managing the disease. It’s also about dealing with treatment side effects. This includes managing fatigue, emotional impacts, and keeping overall health through a balanced lifestyle.
Special Patient Populations: Children and Elderly
Children and elderly patients face unique challenges with blood cancer. Their treatment plans differ due to health, resilience, and other medical conditions.
Pediatric Blood Cancer Treatment Success
Children with blood cancer, like acute lymphoblastic leukemia (ALL), have seen better survival rates. Advances in chemotherapy and care have played a big role in this. Kids often handle tough treatments better than adults, leading to higher success rates.
Treatment for kids with blood cancer includes chemotherapy, radiation, and sometimes stem cell transplants. It’s important to tailor treatment to the child’s genetic and molecular profile for the best results.
Elderly Patient Treatment Challenges
Elderly patients with blood cancer have unique challenges. They often have other health issues, reduced organ function, and a higher risk of complications. Other health problems can limit how intense treatment can be.
It’s key to assess the health and function of elderly patients to choose the right treatment. Geriatric assessment tools help find who can benefit most from intensive therapies.
The section on Age-Specific Treatment Modifications can be enhanced by incorporating a transition phrase to connect the treatment considerations for pediatric patients and elderly patients, improving the overall flow and coherence of ideas.
Children and elderly patients need treatments tailored to their age. For kids, this might mean adjusting doses to avoid long-term side effects. For the elderly, treatments might be less intense or use gentler alternatives.
| Age Group | Treatment Considerations | Common Therapies |
| Pediatric | Minimizing long-term side effects, intensive chemotherapy protocols | Chemotherapy, radiation therapy, stem cell transplantation |
| Elderly | Managing comorbidities, reducing treatment intensity | Modified chemotherapy, targeted therapies, supportive care |
Quality of Life Considerations
For both kids and elderly patients, keeping quality of life high is key. This means managing symptoms, addressing mental health, and supporting patients and families. Starting palliative care early can greatly improve outcomes and satisfaction.
By understanding the unique needs of these groups, we can improve treatment and quality of life for children and elderly patients with blood cancer.
Living with Blood Cancer: Support and Resources
Living with blood cancer is more than just treatment. It needs a full support system. Understanding the resources for patients is key.
Managing Treatment Side Effects
Managing side effects is vital for blood cancer patients. We suggest a mix of medicine, lifestyle changes, and other therapies. For example, chemotherapy can cause fatigue, nausea, or hair loss.
Supportive care like nutrition advice, pain management, and mental support can help a lot. This makes life better for patients.
A study shows that adding palliative care to treatment improves life quality. This shows the need for a complete approach to side effects.
Psychological and Emotional Support
Blood cancer affects patients and families deeply. We stress the need for emotional support. This includes counseling, support groups, and therapies like meditation and yoga.
- Counseling for anxiety, depression, and trauma
- Support groups for patients and families
- Mind-body therapies to reduce stress
One group says emotional support is as important as medical care. This shows the need for a full support system.
Financial Assistance Programs
The cost of blood cancer treatment is high. We know financial help is key. Organizations offer aid for treatment, travel, and more.
“Financial help is vital for care, letting patients focus on treatment, not money.”
Patient Advocacy Organizations
Patient groups are essential for blood cancer support. They offer info on treatments, trials, and services. We suggest connecting with them for better support.
These groups provide many services, like:
| Service | Description |
| Information and Referral | Info on treatments, services, and trials |
| Emotional Support | Support through counseling, groups, and mentoring |
| Advocacy | Support for patient rights and interests |
Conclusion: The Evolving Landscape of Blood Cancer Treatment
The world of blood cancer treatment is changing fast. New therapies like immunotherapy and targeted drugs are making a big difference. These advancements are helping patients live longer and better.
Today, treatments are getting more personal. Doctors use genetic and molecular insights to create plans just for each patient. This shift is making care more precise and effective.
These improvements in treatment are not just about living longer. They also make life better for those fighting blood cancers. More research and trials are needed to keep making progress. This gives hope to those with leukemia, lymphoma, and myeloma.
It’s important to support patients and their families too. They need help with mental health, money, and access to new treatments. By working together, we can keep making blood cancer treatment better.
By embracing new ideas and teamwork, we can make a big difference. Our goal is to manage or cure blood cancers in the future. This will improve lives and give hope to many.
FAQ
References
Liu, M. C., et al. (2025). Evaluation of an innovative multi-cancer early detection test with high specificity but variable sensitivity across cancer types. Frontiers in Oncology, 13, 1520869.
Virdee, P. S., et al. (2024). The association between blood test trends and undiagnosed cancer: A systematic review and critical appraisal. PLoS One, 19(4), e11083147.
Is blood cancer curable?
Whether blood cancer is curable depends on several things. These include the cancer type, how advanced it is, and the patient’s health. Some blood cancers, like certain leukemias and lymphomas, have good cure rates. This is true when caught and treated early.
What are the survival rates for leukemia?
Survival rates for leukemia vary by type. For acute leukemia, treatments have made survival rates better. Chronic leukemia survival rates also vary, depending on the type and patient factors.
How successful is chemotherapy for blood cancer?
Chemotherapy is a common treatment for blood cancer. Its success rate varies by cancer type and stage. It’s often used with other treatments to improve results.
What is the difference between remission and cure in blood cancer?
Remission means the cancer is controlled but might come back. A cure means the cancer won’t return. The difference between remission and cure is complex. It depends on the cancer type and treatment response.
Are there new treatments available for blood cancer?
Yes, new treatments for blood cancer are being tested. These include immunotherapy, gene therapy, and targeted therapies. They offer hope for patients, even those with hard-to-treat cancers.
How does age affect the treatment and survival of blood cancer?
Age is a big factor in blood cancer treatment and survival. Older adults may face more challenges due to health issues. Younger patients, like children and young adults, often have better outcomes with the right treatments.
What support resources are available for patients living with blood cancer?
Patients with blood cancer can find many support resources. These include patient groups, financial help, emotional support, and advice on managing side effects.
Can blood cancer be treated with stem cell transplantation?
Yes, stem cell transplantation is a treatment option for some blood cancers. Success depends on factors like donor match, cancer type, and patient health.
What are the common symptoms of blood cancer?
Common symptoms include fatigue, weight loss, fever, night sweats, and frequent infections. Symptoms vary by cancer type, such as leukemia, lymphoma, or myeloma.
How is blood cancer diagnosed?
Diagnosis involves physical exams, blood tests, bone marrow biopsies, and imaging. Early detection is key for effective treatment and better survival chances.





