Last Updated on October 22, 2025 by mcelik

A bone marrow transplant can significantly impact life expectancy after stem cell transplant. Survival rates and longevity depend on factors like the patient’s age, overall health, and the underlying disease being treated. Advances in medical care and transplant techniques have improved long-term outcomes, allowing many patients to live years or decades beyond their transplant.
Key Takeaways
- Knowing the age limit for bone marrow transplant is key for patients and doctors.
- Survival rates after stem cell transplant change based on the patient’s health and condition.
- Life expectancy after stem cell transplant is affected by many factors, like age and health.
- Bone marrow transplant is a complex process that needs careful planning.
- Patients should talk to their doctors to figure out the best treatment for them.
Bone marrow transplants and stem cell transplants are frequently confused, yet they are distinct procedures.
Bone marrow transplants, also known as stem cell transplants, replace damaged stem cells with healthy ones. This is key for patients with blood disorders and cancers.
Bone marrow transplants and stem cell transplants are frequently confused, yet they are distinct procedures.
Bone marrow transplants and stem cell transplants are frequently confused, yet they are distinct procedures. Bone marrow transplants take stem cells directly from the bone marrow, usually under general anesthesia. On the other hand, stem cell transplants collect stem cells from the blood after using special medicines.
“The choice between bone marrow and stem cell transplant depends on various factors, including the patient’s condition and the donor’s availability,” says , a leading hematologist.
Types of Transplants: Autologous, Allogeneic, and Haploidentical
There are three main types of bone marrow or stem cell transplants:
- Autologous transplants use the patient’s own stem cells, which are collected, stored, and then reinfused after conditioning.
- Allogeneic transplants involve using stem cells from a donor, which can be a related or unrelated match.
- Haploidentical transplants are a type of allogeneic transplant where the donor is a half-match, often a family member.
Each type has its own benefits and risks, like the risk of graft-versus-host disease (GVHD) in allogeneic transplants.
The Importance of Matching Donors and Recipients
Matching donors and recipients is key to avoid complications, like GVHD. The human leukocyte antigen (HLA) typing is used for matching. A close HLA match boosts the transplant’s success and lowers GVHD risk.
Bone marrow transplants and stem cell transplants are frequently confused, yet they are distinct procedures.
Medical Conditions Requiring Bone Marrow Transplants
Bone marrow transplants are needed for many blood and immune system issues. These problems can be very serious and even life-threatening. A bone marrow transplant might be the only cure.
Blood Cancers: Leukemia, Lymphoma, and Multiple Myeloma
Blood cancers are a top reason for bone marrow transplants. Leukemia is a cancer of the blood and bone marrow. It makes abnormal white blood cells.
Lymphoma affects the immune system, mainly the lymphatic system. Multiple myeloma is a cancer of plasma cells in the bone marrow. It causes anemia, bone pain, and infections.
For these cancers, a bone marrow transplant can be a lifesaver. It offers a chance for a cure or better survival chances.
Bone Marrow Failure Syndromes
Bone marrow failure syndromes, like aplastic anemia, happen when the bone marrow doesn’t make enough blood cells. This leads to severe anemia, infections, and bleeding.
A bone marrow transplant is often the best treatment. It’s usually recommended for younger patients or those with a matched donor.
Genetic Disorders like Sickle Cell Disease
Sickle cell disease is a genetic disorder that affects hemoglobin production. It makes red blood cells misshapen and break down. Severe cases might need a bone marrow transplant to fix the genetic problem.
Deciding on a transplant for sickle cell disease is complex. It involves weighing the risks and benefits, including the age limit for the transplant.
Immune Deficiency Disorders
Some immune deficiency disorders can be treated with a bone marrow transplant. These include severe combined immunodeficiency (SCID) and other congenital immunodeficiencies. A transplant can replace bad immune cells with healthy ones from a donor.
Knowing about the medical conditions that need bone marrow transplants is key. It helps patients and their families make informed choices about treatment. They can understand the benefits and risks of bone marrow transplantation.
Age Considerations for Bone Marrow Transplant Recipients
Medical technology has made it easier for older people to get bone marrow transplants. Before, age was a big issue because of the risks. But now, thanks to better care and techniques, more older patients can get transplants.
Historical Age Restrictions and Why They Existed
Older patients used to face big hurdles getting transplants. Doctors worried about the risks and how well they could handle the procedure. But, as transplant success rates have gone up, these barriers have come down.
Current Age Guidelines for Different Types of Transplants
Age rules differ based on the transplant type. Autologous transplants, where the patient’s own stem cells are used, are less age-restricted. Allogeneic transplants, which use donor cells, have stricter age limits. Haploidentical transplants, using half-matched donors, also offer hope for older patients.
Each transplant center has its own age limits. Some might accept patients up to 70 or more for certain transplants, depending on their health.
How Comorbidities Affect Eligibility More Than Chronological Age
Age is important, but health conditions matter more for transplant eligibility. Patients with serious health issues, like heart or lung disease, are at higher risk. But, older patients with fewer health problems might be good candidates.
Comprehensive geriatric assessments help doctors check an older patient’s health and fitness. This helps decide if they’re right for a transplant.
Age, health conditions, and transplant eligibility are all connected. Each patient needs a careful look to decide if a transplant is right for them.
Age Limits for Bone Marrow and Stem Cell Donors
It’s important to know the age limits for bone marrow and stem cell donors. These limits can change based on the donation type and the registry’s rules.
Age Requirements for Joining Bone Marrow Registries
Bone marrow registries usually ask for donors to be between 18 and 40. This is because younger donors are often healthier. They have a lower risk of problems during the donation.
Be The Match Age Limit Policies
Be The Match, a big bone marrow registry, has age rules for donors. You can join if you’re 18 to 40. But, the upper age limit can change based on the recipient’s needs and the donor’s health.
Why Younger Donors Are Often Preferred
Younger donors are often chosen because they’re healthier. They have fewer health issues. This makes the donation process safer and increases the transplant’s success rate.
Special Considerations for Family Member Donors
Family donors, like siblings or kids, might be considered even if they’re not in the usual age range. The choice to use a family donor depends on HLA matching and the donor’s health.
In summary, while there are age guidelines for donors, individual cases can change things. Donors should talk to their doctor and the registry to see if they can donate.
The Evaluation Process for Transplant Candidates
Checking if someone can get a bone marrow transplant is a detailed process. It’s important to see if they’re healthy enough and if the transplant will help them.
Pre-transplant Testing and Assessments
Before getting a bone marrow transplant, patients go through many tests. These tests check their health, the state of their illness, and if they can handle the transplant.
- Medical History Review: A deep look into the patient’s past health to see if it might affect the transplant.
- Physical Examination: A full check-up to see how the patient is doing now.
- Laboratory Tests: Blood tests to check blood counts, organ function, and other important health signs.
- Cardiac Evaluation: Heart tests, like echocardiograms, to make sure the patient can handle the transplant.
- Pulmonary Function Tests: Lung tests to see if the patient might have breathing problems after the transplant.
The Role of the Transplant Team in Determining Eligibility
The transplant team is key in deciding who can get a bone marrow transplant. This team includes doctors, nurses, and other experts.
They look at the test results, the patient’s health, and their medical history. They also talk about the risks and benefits of the transplant with the patient.
How Decisions Are Made for Borderline Cases
For patients who are not clear-cut candidates, the decision is made carefully. The team considers the patient’s age, health, and illness status.
In some cases, more tests or evaluation might be needed. The team works with the patient and their family to make the best choice for them.
Reduced-Intensity Conditioning: Expanding Access for Older Patients
Reduced-intensity conditioning is a big step forward in bone marrow transplants. It makes transplants possible for older or sicker patients. This method is gentler than the old way, which was too harsh for many.
What is Reduced-Intensity Conditioning?
Reduced-intensity conditioning is a gentler way to prepare for a bone marrow or stem cell transplant. It uses lower doses of chemotherapy and radiation. This helps the new cells take hold without harming the patient too much.
Benefits for Older or Medically Compromised Patients
This gentler approach is great for older or very sick patients. It lowers the risk of serious side effects and death from the treatment. This means more people can get life-saving treatments they couldn’t before.
It also helps the body accept the new cells more smoothly. This can lower the chance of serious complications like graft-versus-host disease.
Success Rates Compared to Traditional Conditioning
While it might lead to more relapses, the survival rates for older patients are often the same or better. This is because fewer die from the treatment itself.
The bone marrow transplant survival rate by age has gone up, thanks to this method. It’s shown that older patients can live longer and better with the right care.
In short, reduced-intensity conditioning has changed the game for bone marrow transplants. It offers a chance for older or sicker patients to get the treatment they need without too much harm.
Bone Marrow Transplant Survival Rate by Age
The survival rate of bone marrow transplants changes a lot with age. This is due to many factors.
Statistical Outcomes for Different Age Groups
Younger patients usually do better after bone marrow transplants than older ones. A study in the Journal of Clinical Oncology found big differences. Patients under 30 did much better than those over 50.
The Center for International Blood and Marrow Transplant Research (CIBMTR) has data too. They say patients under 40 have a 50-60% survival rate. But, for those between 40 and 60, it’s only 30-40%.
How Age Impacts Short-Term Survival
Age really matters for survival right after a bone marrow transplant. Older patients face more problems like GVHD, infections, and organ damage. These issues can hurt their chances of living in the short term.
A study in the Journal of Hematology & Oncology found something important. Older patients are more likely to get severe GVHD. This can lead to higher death rates in the first year after the transplant.
Long-Term Survival Considerations
Many things affect how long someone can live after a bone marrow transplant. These include their age, the disease being treated, and any other health problems.
, a top hematologist, said something interesting. “Age is important, but it’s not everything. New treatments and care have helped older patients live longer.”
Recent Improvements in Outcomes for Older Patients
Recently, things have gotten better for older patients getting bone marrow transplants. This is thanks to new, gentler treatments and better care.
“The introduction of reduced-intensity conditioning has been a game-changer for older patients, allowing more individuals to benefit from bone marrow transplants who were previously considered too high-risk.”
These new steps have made more older patients eligible for transplants. This means they can get the treatment with a better chance of success.
Short-term Recovery Milestones
The first time after a stem cell transplant is very important. Patients face many side effects, like feeling tired and sick. It’s vital to watch them closely and get the right care to handle these issues.
Here are some key moments in the short-term recovery:
- Engraftment, where the new stem cells start making blood cells
- When blood counts get back to safe levels
- When immediate problems after the transplant get better
One-year, Five-year, and Ten-year Survival Statistics
Survival rates after stem cell transplants have gotten better over time. This is thanks to new medical tech and better care. But, survival rates depend on the disease, the patient’s age, and the type of transplant.
Recent studies show:
- One-year survival: About 70-80%
- Five-year survival: Around 50-60%
- Ten-year survival: About 30-50%
These numbers are hopeful and show a positive trend in long-term results.
Factors Influencing Long-term Outcomes
Many things can affect how long you live and how well you do after a stem cell transplant. These include:
- Your overall health and any other health issues
- How well the donor’s cells match with yours
- The type of transplant you had
- The care you get after the transplant and how well you manage any problems
Doctors say, “The secret to doing well long-term is good care after the transplant and teaching patients how to take care of themselves.”
“The journey after a stem cell transplant is a marathon, not a sprint. It requires patience, resilience, and a strong support system.”
” Expert in Hematology and Stem Cell Transplantation
Quality of Life Considerations
Living well after a stem cell transplant is a big worry for patients. The transplant can save your life but also brings challenges. Rehab and mental support are key to getting strong again and adjusting to life after the transplant.
Many patients see their quality of life improve as they get better. They start doing things they love again and feel healthier and more alive.
The Bone Marrow Donation Process and Risks
Donating bone marrow can save lives, but it’s important to know the risks and steps involved. The process includes several stages, from signing up to the actual donation and care after.
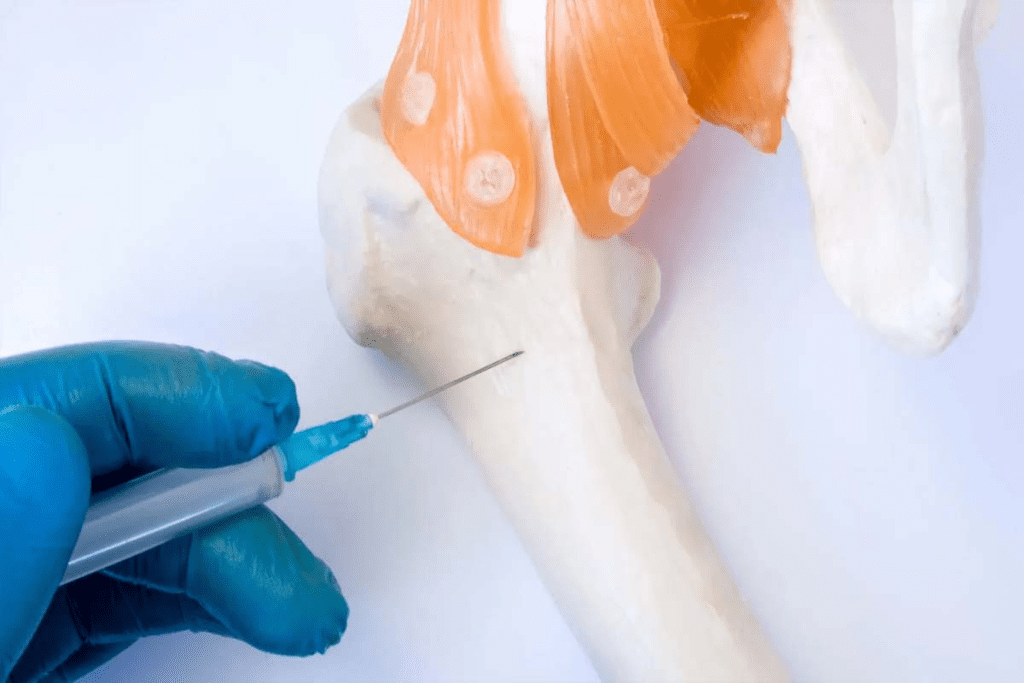
Methods of Collection
Bone marrow transplants and stem cell transplants are frequently confused, yet they are distinct procedures.
Common Side Effects and Recovery Time
Donors might feel tired, have pain or bruising at the site, and more. Recovery time depends on the method used. For aspiration, it takes 2-4 weeks. For PBSC, it’s a few days to a week.
- Fatigue
- Pain at the collection site
- Bruising
- Potential risks associated with anesthesia for bone marrow aspiration
Long-term Effects on Donors
Studies show that long-term effects are usually small. Some donors might feel tired or have minor issues. It’s key to follow care instructions after donation to avoid long-term problems.
Is it Dangerous to Give Bone Marrow?
Bone marrow donation is generally safe, but it comes with risks like any medical procedure. Serious problems are rare, but they can happen. It’s important to talk to a healthcare provider about your specific risks and worries.
In summary, bone marrow donation has risks, but knowing the process and precautions can help. Donors should think carefully and talk to doctors before deciding.
Frequency of Bone Marrow Donation
Many people wonder if they can donate bone marrow more than once. It’s a big decision, and knowing the rules is key.
Can You Give Bone Marrow More Than Once?
Yes, you can donate bone marrow more than once. But, it depends on your health and the recipient’s needs. Also, the rules of the registry or transplant center matter.
If you’ve donated before, you might be able to do it again. You need to be healthy, match the recipient, and meet certain requirements.
Recommended Intervals Between Donations
The time between donations varies. For peripheral blood stem cell (PBSC) donations, it’s usually 8 weeks (56 days). Bone marrow donations might take longer, from months to a year or more.
Donating can affect your body, like making you tired or causing bone pain. You need time to get better before donating again.
Lifetime Limits on Donation Frequency
There’s no strict limit on how many times you can donate bone marrow. But, registries and transplant centers have rules to keep donors safe. The National Marrow Donor Program (NMDP), also known as Be The Match, has these rules.
Donors can usually donate once. But, in some cases, they might be allowed to donate again. This decision depends on your health and the donation’s specifics.
So, how often you can donate bone marrow depends on medical guidelines, registry rules, and your health.
Special Considerations for Specific Conditions
Bone marrow transplants are a key treatment for many serious conditions. Each condition has its own needs. The success of these transplants depends on many things, like the condition, the patient’s age, and the donor’s health.
Bone Marrow Transplant for Sickle Cell Disease Age Limits
Sickle cell disease affects how red blood cells are made, leading to their breakdown. Bone marrow transplants can cure it. But, choosing to have this transplant is a big decision, mainly because of age limits.
Younger patients usually do better because they have fewer health problems and a stronger immune system. Yet, new medical technologies have made it possible for older patients to be considered for transplants too.
Leukemia Transplant Success Rates Across Age Groups
Bone marrow transplants and stem cell transplants are frequently confused, yet they are distinct procedures.
Older patients face more hurdles but can also have good results. This depends on careful selection and management.
Transplantation for Elderly Patients with Myelodysplastic Syndromes
Myelodysplastic syndromes (MDS) are disorders where blood cells don’t form right. Elderly patients with MDS might get bone marrow transplants. But, their age and health issues make it tough.
Reduced-intensity conditioning regimens have helped more elderly patients get transplants. This makes transplantation a possible option for more older patients.
The First 100 Days: Critical Post-Transplant Period
The first 100 days after a bone marrow transplant are key to seeing if the transplant worked. During this time, doctors watch for any problems or graft-versus-host disease (GVHD). Good post-transplant care is important for a smooth recovery.
Milestones at 30, 60, and 100 Days After Transplant
Patients hit big milestones in the first 100 days. By 30 days, they start to recover and the bone marrow starts working. At 60 days, doctors check for GVHD or other issues and adjust treatment plans if needed. By 100 days, many patients have made a lot of progress, but they must keep being watched.
Common Complications and How They’re Managed
During the first 100 days, patients might face infections, GVHD, or organ damage. Doctors use immunosuppressive therapy, antibiotics, and supportive care to manage these problems. The transplant team keeps a close eye on patients to catch and fix any issues quickly.
The Importance of Close Monitoring
Watching patients closely in the first 100 days is key to catching problems early. Regular check-ups and tests help doctors act fast to improve outcomes. This time is also when patients learn about self-care and spotting complications.
When Patients Can Return to Normal Activities
When patients can go back to normal activities varies. It depends on their health and the transplant details. Usually, by 100 days, most can start doing most things they did before. But some might need more time to fully get better.
Knowing how important the first 100 days are helps patients and their families get ready for what’s ahead. With the right care and watching, many patients can have a good outcome and better quality of life.
Long-Term Effects and Follow-Up Care
The journey doesn’t end with the stem cell transplant. Patients must deal with long-term effects that can affect their quality of life. It’s important to know these effects to manage them well and improve survival rates.
Chronic Graft-Versus-Host Disease Management
Chronic graft-versus-host disease (cGVHD) is a big problem after allogeneic stem cell transplants. It happens when the donor’s immune cells attack the recipient’s tissues. Effective management of cGVHD is key to avoid organ damage and improve life quality.
Management strategies include:
- Immunosuppressive therapy to reduce the immune system’s attack on the body’s tissues.
- Supportive care to manage symptoms and prevent infections.
- Regular monitoring to adjust treatment plans as necessary.
Secondary Malignancies and Risk Factors
People who have had stem cell transplants are at higher risk of getting secondary malignancies. These include myelodysplastic syndromes and other cancers. The risk is higher if the conditioning regimen was harsh, if more radiation was used, or if there’s graft-versus-host disease.
Regular follow-up care is key for early detection and management of secondary malignancies. This includes:
- Annual check-ups with a healthcare provider.
- Screening tests as recommended based on individual risk factors.
- Lifestyle modifications to reduce cancer risk.
Organ System Effects and Monitoring
Stem cell transplant can affect many organ systems, leading to problems like cardiovascular disease, pulmonary issues, and endocrine disorders. Long-term monitoring is vital to catch and manage these issues early.
Patients should work closely with their healthcare team to monitor their health and address any concerns promptly.
Psychological and Social Considerations
The psychological and social impact of stem cell transplantation is significant. Survivors may face anxiety, depression, and changes in social relationships. Supportive care services, like counseling and support groups, are important in helping patients cope with these challenges.
By understanding the long-term effects of stem cell transplants and engaging in proactive follow-up care, patients can improve their quality of life and survival outcomes.
Conclusion: The Evolving Landscape of Bone Marrow Transplantation
The age limit for bone marrow transplant has changed a lot. Now, older patients have more treatment options. This is thanks to new ways of preparing for the transplant and better care after it.
Knowing how long someone might live after a stem cell transplant is very important. Recent studies show that more people are living longer and better after the transplant. This is great news for patients and their families.
Medical technology keeps getting better, making bone marrow transplants available to more people. Research and new transplant methods are on the horizon. They promise to help even more patients of all ages.
With bone marrow transplants getting better, patients and doctors have more hope. The future looks bright for better survival rates and a better quality of life for everyone.
FAQ
What is the age limit for bone marrow transplant?
The age limit for bone marrow transplant changes based on the type of transplant and the patient’s health. There’s no strict upper age limit. But older patients are checked for health issues that might affect their eligibility.
What is the difference between bone marrow and stem cell transplants?
Bone marrow transplants and stem cell transplants are frequently confused, yet they are distinct procedures.ot exactly the same. Bone marrow transplants take stem cells directly from the bone marrow. Stem cell transplants collect stem cells from the blood.
Can you give bone marrow more than once?
Bone marrow transplants and stem cell transplants are frequently confused, yet they are distinct procedures.
What are the risks associated with bone marrow donation?
Donating bone marrow can cause pain, fatigue, and infection. But serious problems are rare. Most donors get better in a few weeks.
How does age impact bone marrow transplant survival rates?
Age can affect how well a bone marrow transplant works. Older patients face more risks and lower survival rates. But new transplant methods and care have helped older patients do better.
What is reduced-intensity conditioning, and how does it benefit older patients?
Reduced-intensity conditioning uses lower doses of treatment to prepare for a transplant. It helps older patients by reducing side effects and improving transplant success.
What are the age requirements for joining bone marrow registries?
Age limits for joining bone marrow registries vary. Most registries, like Be The Match, accept donors between 18 and 60. Some registries might have different age limits.
How long does it take to recover from bone marrow donation?
Recovering from bone marrow donation takes a few weeks. Donors may feel tired, in pain, and have other side effects. Most can get back to normal in a month.
What are the long-term effects of stem cell transplant?
Stem cell transplant can lead to long-term issues like chronic graft-versus-host disease and secondary cancers. Patients need ongoing care to manage these risks and ensure the best outcomes.
Can older patients with myelodysplastic syndromes benefit from bone marrow transplant?
Yes, older patients with myelodysplastic syndromes can benefit from bone marrow transplant. Their eligibility is based on their health and other conditions. Reduced-intensity conditioning is often beneficial for older patients.
What is the success rate of leukemia transplant across different age groups?
Leukemia transplant success rates vary by age. Younger patients usually have better outcomes. But new transplant techniques and care have improved results for older patients.
How often can you donate bone marrow?
Bone marrow donation frequency is regulated for safety. Donors can usually donate once. But in some cases, they might be able to donate again after several years.
What are the milestones at 30, 60, and 100 days after bone marrow transplant?
The first 100 days after transplant are critical. Key milestones include engraftment, recovery of blood counts, and managing complications. Patients are closely monitored to ensure the best outcomes.
When can patients return to normal activities after bone marrow transplant?
Patients can usually return to normal activities several months after transplant. This varies based on their recovery and any ongoing complications.
References
- American Cancer Society. (2023). Bone marrow transplant and stem cell transplant. Retrieved from https://www.cancer.org/treatment/treatments-and-side-effects/stem-cell-and-bone-marrow-transplants.html
- National Marrow Donor Program. (2023). Bone marrow donation process. Retrieved from https://bethematch.org/for-donors-and-volunteers/donation-process/
- National Cancer Institute. (2023). Stem cell transplants in cancer treatment. Retrieved from https://www.cancer.gov/about-cancer/treatment/types/stem-cell-transplant
- U.S. National Library of Medicine. (2023). Hematopoietic stem cell transplantation: A review. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539828/