Last Updated on November 27, 2025 by Bilal Hasdemir
Understanding malignant meningioma is key for those looking for answers. We aim to give detailed info on this rare and aggressive meningioma. It grows fast and often comes back.
At Liv Hospital, we lead in advanced care for cancer meningioma. We give families the latest research and care. Our focus is on the grades of meningioma for personalized treatment.
Key Takeaways
- Understanding the different grades of meningioma is key for diagnosis and treatment.
- Malignant meningioma is a serious brain cancer needing special care.
- Advanced diagnostic techniques are vital for accurate grading.
- Patient-centered care is essential for managing the condition well.
- Survival rates depend on the grade and diagnosis of meningioma.
- Liv Hospital offers full care and support for international patients.
What Are Meningiomas and How Do They Develop?
Meningiomas start in the meninges, which protect our brain and spinal cord. These tumors are usually not cancerous and grow from the meninges. Their growth is influenced by genetics and the environment.
Origin and Formation in the Meninges
Meningiomas come from the arachnoid cells in the meninges. The meninges have three layers: dura mater, arachnoid mater, and pia mater. The arachnoid layer is where most meningiomas form.
The exact reason for meningioma growth is not known. But, genetic changes are thought to be key. These changes can be caused by radiation or genetic conditions.
Common Locations and Prevalence
Meningiomas can grow anywhere the meninges are. But, they often appear near the brain’s surface. They are found near the sagittal sinus, on the brain’s sides, and at the skull base.
These tumors are common, making up 30% of brain tumors in adults. They are more common in women and get more frequent with age. Hormones might play a part in this gender difference.
Risk Factors and Causes
The exact cause of meningiomas is unknown. But, some risk factors have been found. Ionizing radiation and genetic conditions like neurofibromatosis type 2 increase the risk.
Hormones and environmental factors might also play a role. But, more research is needed to understand meningioma causes and risk factors.
The Classification System: Understanding Meningioma Grades
Knowing how meningiomas are classified is key to finding the right treatment and understanding the future. The World Health Organization (WHO) grades them from 1 to 3. This is based on their look and how they act. This helps doctors know what to expect and how to help patients.
Grade 1 Meningioma: Benign Characteristics
Grade 1 meningiomas are not harmful and usually do well. They grow slowly and rarely come back after surgery. Benign meningiomas are often treated with surgery. Sometimes, watching them closely is enough if they’re not causing problems.
Grade 2 Meningioma: Atypical Features
Grade 2 meningiomas are not as good as Grade 1. They grow faster and come back more often. They might need surgery and radiation therapy. The atypical features of Grade 2 meningiomas mean they need to be watched closely.
Grade 3 Meningioma: Malignant Indicators
Grade 3 meningiomas are the most serious. They grow fast, come back a lot, and can spread to other parts of the brain. Treatment for malignant meningiomas usually includes surgery, radiation, and sometimes chemotherapy.
Putting meningiomas into these three grades helps doctors plan the best treatment. Knowing about each grade helps doctors give better care. This leads to better results for patients.
Malignant Meningioma: Key Characteristics and Behavior
Malignant meningiomas have unique features that set them apart from benign ones. These traits help us understand why they grow aggressively and affect patients’ health.
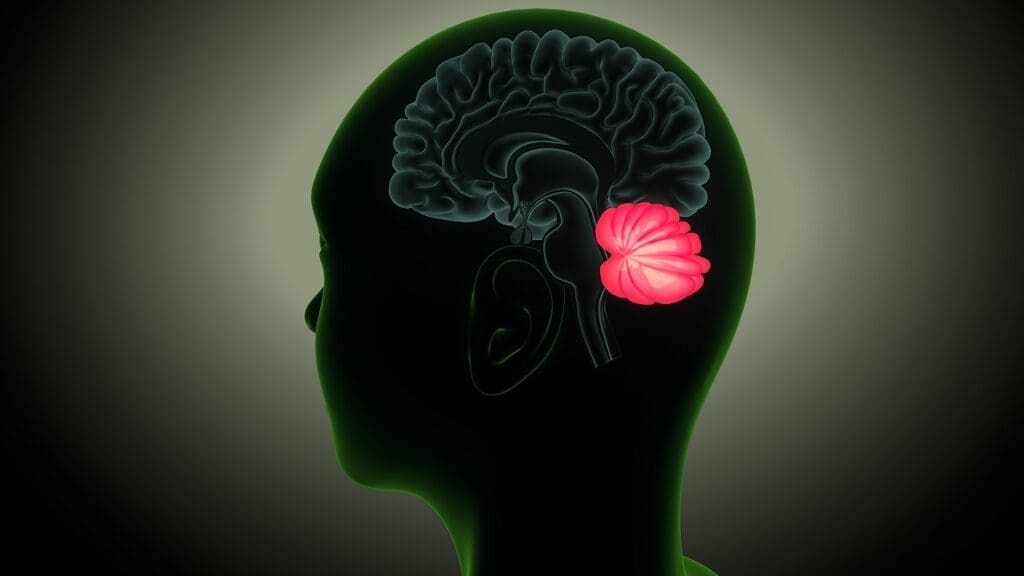
Cellular and Histological Features
Malignant meningiomas have a lot of cells, unusual cell shapes, and lots of cell division. These signs show they are aggressive and can grow fast.
Histological examination shows papillary or rhabdoid morphology. This is linked to a more serious disease. The World Health Organization (WHO) grades meningiomas based on these features. Malignant ones are usually WHO Grade III.
“The histological features of malignant meningiomas, including high mitotic rates and presence of necrosis, are critical in distinguishing them from lower-grade meningiomas.” –
Aggressive Growth Patterns
Malignant meningiomas grow quickly and spread into brain tissues. This makes surgery hard and increases the chance of coming back.
These tumors can spread in unpredictable ways. They can grow into nearby brain areas. This makes it hard to remove them completely.
| Feature | Benign Meningioma | Malignant Meningioma |
|---|---|---|
| Cellularity | Low to Moderate | High |
| Mitotic Activity | Low | High |
| Growth Pattern | Slow, Expansile | Rapid, Invasive |
Invasion and Metastatic Potentia
Malignant meningiomas can spread into nearby tissues and, rarely, to other parts of the body. Their ability to spread makes treatment harder and worsens their outlook.
It’s important to know how likely these tumors are to spread. While it’s rare, it can happen, mainly if they have spread a lot locally.
Because of their complex behavior, treating malignant meningiomas needs a team effort. This includes surgery, radiation, and sometimes chemotherapy or targeted treatments.
Can Meningiomas Be Cancerous? The Spectrum of Malignancy
Meningiomas are usually seen as benign tumors. But, they can sometimes act like cancer, leading to questions about their malignancy. We will look into how meningiomas can change from benign to malignant.
Defining Cancer in Meningiomas
Cancer in meningiomas shows aggressive growth and invades nearby tissues. Most meningiomas are benign (Grade 1). But, some are atypical (Grade 2) or malignant (Grade 3), being the most aggressive. We will talk about what makes a meningioma cancerous and what it means for treatment.
Transformation from Benign to Malignant
Some meningiomas can turn from benign to malignant over time. The reasons for this change are not fully known. We will look into what causes this transformation and its importance in medicine.
Anaplastic Meningioma as a True Cancer
Anaplastic meningioma, or Grade 3 meningioma, is a true cancer. It grows very aggressively and has a poor outlook. These tumors have high cell division, a lot of cell death, and easily spread and invade. We will discuss what makes anaplastic meningioma so challenging to treat.
In summary, while most meningiomas are benign, there are malignant forms. Knowing about these changes is key to finding better treatments. We will keep exploring the impact of malignancy in meningiomas in the next sections.
Diagnosing Meningiomas: From Symptoms to Confirmation
Diagnosing meningiomas is a detailed process. It starts with noticing common symptoms and ends with confirmation through advanced imaging and tissue analysis. This thorough method ensures accurate diagnosis and helps decide on treatment.
Common Presenting Symptoms
Meningiomas can cause symptoms based on their location and size. Symptoms include headaches, seizures, and neurological deficits like weakness or numbness in limbs. The symptoms’ nature and severity differ among patients, depending on the tumor’s location and its effect on brain tissue.
In some cases, meningiomas may not show symptoms and are found by chance during imaging for other reasons. But, when symptoms do appear, they usually lead to further investigation.
Imaging Techniques (MRI, CT, Angiography)
Imaging is key in diagnosing meningiomas. Magnetic Resonance Imaging (MRI) is often the first choice because it’s very sensitive and shows soft tissues well. MRI helps find the tumor’s size, location, and how it affects nearby tissues.
Computed Tomography (CT) scans are used too, mainly in emergencies or when MRI isn’t available. CT scans can quickly spot larger tumors and any complications like bleeding or fluid buildup in the brain.
Cerebral angiography might be used to check the tumor’s blood supply and plan treatments like surgery or endovascular interventions.
The Role of Neuropathologists in Tissue Analysis
While imaging gives important details, the final diagnosis of a meningioma comes from histopathological examination of tissue samples. Neuropathologists are essential in analyzing these samples to confirm the diagnosis and determine the tumor’s grade.
Neuropathologists examine tissue morphology and cellular characteristics to classify meningiomas. They use the World Health Organization (WHO) classification system. This helps guide treatment and predict the outcome.
Treatment Approaches Based on Meningioma Grade
Knowing the grade of a meningioma is key to picking the right treatment. The tumor’s grade affects the treatment choice, from simple management to more aggressive methods.
Surgical Resection Strategies
Surgery is often the first step for meningiomas, mainly for Grade 1 and some Grade 2. The aim is to remove the tumor and some surrounding tissue to get rid of all cancer cells.
The surgery method depends on the tumor’s location and size. Tumors near important areas might need special care to avoid harming the brain or nerves.
- Microsurgical techniques for precise tumor removal
- Endoscopic surgery for minimally invasive approaches
- Craniotomy for larger or more complex tumors
Radiation Therapy Protocols
Radiation is often suggested for Grade 2 and Grade 3 meningiomas, or for tumors left behind after surgery. It’s also used for tumors that can’t be removed surgically.
Modern radiation methods like stereotactic radiosurgery (SRS) and intensity-modulated radiation therapy (IMRT) target the tumor precisely. They help protect the healthy tissue around it.
| Radiation Technique | Description | Application |
|---|---|---|
| SRS | Delivers high-dose radiation in a single fraction | Small, well-defined tumors |
| IMRT | Modulates radiation beams to conform to tumor shape | Larger or irregularly shaped tumors |
| Fractionated RT | Divides total dose into multiple fractions | Tumors near critical structures |
Chemotherapy for Malignant Cases
Chemotherapy is mainly for malignant (Grade 3) meningiomas or those that come back after other treatments. The choice of chemotherapy depends on several factors, like previous treatments and the tumor’s characteristics.
Common chemotherapy regimens include:
- Hydroxyurea
- Temozolomide
- Combination therapies
Emerging Targeted Therapies
Research into targeted treatments for meningiomas is growing. New approaches target specific molecular pathways involved in tumor growth and spread.
As we learn more about meningioma biology, we’ll see better and more tailored treatments come along.
Survival Rates for Different Meningioma Grades
The outlook for meningioma patients changes with the tumor grade. Knowing these differences helps both patients and doctors make better choices about treatment and care.
Excellent Prognosis for Grade 1 Meningioma
Grade 1 meningiomas are usually benign and have a great outlook. The survival rate for meningioma patients with Grade 1 tumors is very high. Most patients live a normal life after treatment, which often includes surgery to remove the tumor.
Studies show that the 5-year survival rate for Grade 1 meningioma patients is over 90%. Many patients are cured after surgery.
Intermediate Outcomes for Grade 2 Meningioma
Grade 2 meningiomas are atypical and have a higher chance of coming back. The meningiomas survival rate for Grade 2 is lower than for Grade 1, with a 5-year survival rate between 70% and 80%. Treatment for Grade 2 meningiomas often includes surgery and radiation therapy to slow tumor growth and lower the risk of coming back.
Survival Statistics for Grade 3 Meningioma
Grade 3 meningiomas are malignant and have the worst prognosis. The prognosis of meningiomas for Grade 3 is generally poor, with a much lower survival rate than Grade 1 and Grade 2 tumors. The 5-year survival rate for Grade 3 meningioma patients can be as low as 30% to 50%, depending on several factors like how much of the tumor is removed and how well the patient responds to additional treatments.
In summary, knowing the survival rate for meningioma based on the tumor grade is key for managing patient hopes and guiding treatment choices. While Grade 1 meningiomas have a great outlook, Grade 2 and Grade 3 tumors need more aggressive treatments and have different outcomes.
Recurrence Patterns and Long-term Monitoring
The risk of meningioma coming back depends on its grade. This means we need to watch patients closely over time. Early detection and treatment are key to managing the disease.
Follow-up Protocols by Grade
Every meningioma patient is different, and so is their follow-up care. Grade 1 meningiomas are usually benign and need less frequent checks. Patients with these tumors might have MRI or CT scans every 6 to 12 months at first. If there’s no sign of the tumor coming back, they might only need scans once a year.
Grade 2 and 3 meningiomas are at higher risk of coming back. So, they need more careful watching. Doctors might recommend scans every 3 to 6 months at first. This can change to annual scans if the tumor stays stable. The exact plan depends on the patient and the doctor’s advice.
| Meningioma Grade | Initial Follow-up Interval | Long-term Follow-up Interval |
|---|---|---|
| Grade 1 | 6-12 months | Annually |
| Grade 2 | 3-6 months | 6-12 months |
| Grade 3 | 3 months | 6 months |
Warning Signs of Recurrence
It’s important for patients to know the signs of meningioma coming back. These include new or worse symptoms like headaches, seizures, vision problems, or weakness. If you notice any of these, get checked with imaging right away.
Management Strategies for Recurrent Disease
When meningioma comes back, treatment depends on several factors. These include the tumor’s grade, where it is, and what treatments it’s had before. Options might include surgery, radiation, or chemotherapy. New treatments are also being looked into.
Handling meningioma that comes back needs a team effort. Neurosurgeons, radiation oncologists, and medical oncologists all play a part. We work with patients to create treatment plans that fit their needs and goals.
Living with a Meningioma Diagnosis: Patient Perspectives
Getting a meningioma diagnosis can be tough. It takes a lot of strength, support, and knowing what it means. Patients face big challenges that can change their life and how they feel.
Coping Strategies
Dealing with meningioma needs a mix of medical care, emotional support, and changes in lifestyle. Here are some ways patients can cope:
- Education and Awareness: Knowing about their condition helps patients make better choices for their health.
- Support Networks: Having family, friends, and support groups can offer comfort and help.
- Mind-Body Techniques: Activities like meditation, yoga, and mindfulness can help with stress and mental health.
Quality of Life Considerations
The life quality of meningioma patients can change based on the tumor’s size, location, and treatment. Important things to think about include:
- Handling symptoms and side effects of treatment.
- Keeping physical function and mobility.
- Dealing with changes in thinking and feelings.
Healthcare teams can help improve patients’ life quality by focusing on these areas.
Support Resources and Communities
It’s important for meningioma patients to have access to support and communities. These can include:
- Patient Support Groups: A place to share experiences and get advice.
- Online Forums and Social Media: A space to connect with others who face meningioma challenges.
- Professional Counseling: Help for patients and families to deal with emotional effects of the diagnosis.
Using these resources, patients can get the support they need to handle their diagnosis well.
Current Research and Future Directions in Meningioma Treatment
New paths in treating meningioma are being explored. Research aims to better understand meningioma, find more effective treatments, and improve patient care.
Advances in Molecular Classification
Recent studies have made big strides in classifying meningiomas by their genes. This molecular profiling helps doctors tailor treatments for each patient. It could lead to better results.
Advanced molecular techniques, like next-generation sequencing, have given us new insights. These discoveries are key for creating targeted treatments that can better manage meningioma.
Novel Therapeutic Approaches
New treatments are being tested to tackle meningioma’s challenges. Targeted therapies that target specific growth pathways are showing promise.
Clinical trials are underway to check these new treatments’ safety and effectiveness. These include immunotherapies that use the body’s immune system to fight cancer. They could greatly improve patient outcomes.
Improving Outcomes for Malignant Cases
Malignant meningiomas are tough to treat because they grow fast and have a poor outlook. Researchers are working on better treatments, like combination therapies and advanced radiation.
They’re also studying the biology of these aggressive tumors to find new ways to intervene. This research could lead to better survival rates and quality of life for patients.
Conclusion
Understanding malignant meningioma is key for both patients and doctors. We’ve looked into how to diagnose meningioma, its types, and treatment options. This includes how the tumor’s grade affects treatment.
Getting a diagnosis early and choosing the right treatment is essential. We’ve talked about how new imaging and lab tests help doctors diagnose better. This leads to treatments like surgery, radiation, and new targeted therapies.
As we learn more about meningioma, we can find new ways to treat it. For those with malignant meningioma, knowing what to expect and getting the right care is important. It helps improve their chances of doing well.
We need to keep researching and spreading the word about meningioma. This will help us manage it better. It’s all about making life better for those dealing with this tough condition.
FAQ
What is a meningioma, and how does it develop?
A meningioma is a tumor that grows in the meninges. These are protective membranes around the brain and spinal cord. It happens when cells in the meninges grow abnormally, forming a tumor.
What are the different grades of meningioma, and what do they mean?
The World Health Organization (WHO) classifies meningiomas into three grades. Grade 1 is benign, Grade 2 is atypical, and Grade 3 is malignant. The grade shows how aggressive the tumor is and how likely it is to come back.
What are the characteristics of malignant meningioma?
Malignant meningioma, or Grade 3, grows aggressively. It has high cell division and can spread and invade other areas. We consider these tumors true cancers.
Can benign meningiomas become malignant?
Yes, benign meningiomas can turn into malignant tumors over time. We keep a close eye on patients with benign meningiomas to catch any changes.
How are meningiomas diagnosed?
We diagnose meningiomas with imaging like MRI, CT, and angiography. A neuropathologist also analyzes tissue samples. These tools help us find the tumor’s grade and plan treatment.
What are the treatment options for meningiomas?
Treatment for meningiomas depends on the tumor’s grade and where it is. Options include surgery, radiation, chemotherapy, and new targeted therapies.
What are the survival rates for different grades of meningioma?
Survival rates vary by meningioma grade. Grade 1 has a great prognosis, but Grade 3 has a worse outlook.
How often should I have follow-up appointments after a meningioma diagnosis?
Follow-up visits depend on the tumor’s grade and treatment. Regular checks help catch any recurrence or changes in the tumor.
What are the warning signs of meningioma recurrence?
Signs of recurrence include new or worsening symptoms like headaches, seizures, or neurological problems. It’s important to tell your doctor about any changes.
Are there any support resources available for patients living with meningioma?
Yes, we offer support like counseling, support groups, and online communities. These help patients deal with their diagnosis and improve their quality of life.
What advancements are being made in meningioma research?
Research is exploring new ways, like molecular classification and novel treatments, to improve meningioma care. This is important for malignant cases.
Reference:
https://www.cancer.gov/rare-brain-spine-tumor/tumors/meningioma