Last Updated on December 2, 2025 by Bilal Hasdemir
After a mastectomy, patients face a tough recovery at home. This can take weeks. Understanding the limits on arm use is essential for safe healing.
A mastectomy changes the body and mind. It leads to big emotional aftermath and body image shift. As patients heal, knowing these changes is vital. It helps with daily tasks, like moving arms.
Get the mastectomy untold insights no one talks about. We reveal the shocking truth about recovery, sensation, and emotional healing.
Key Takeaways
- Understanding arm usage restrictions is key after a mastectomy.
- Recovery at home can last weeks.
- Knowing the emotional and body changes is important.
- Clear arm care advice is needed for a smooth recovery.
- Following specific instructions helps avoid problems.
What is a Mastectomy and Why is it Performed?
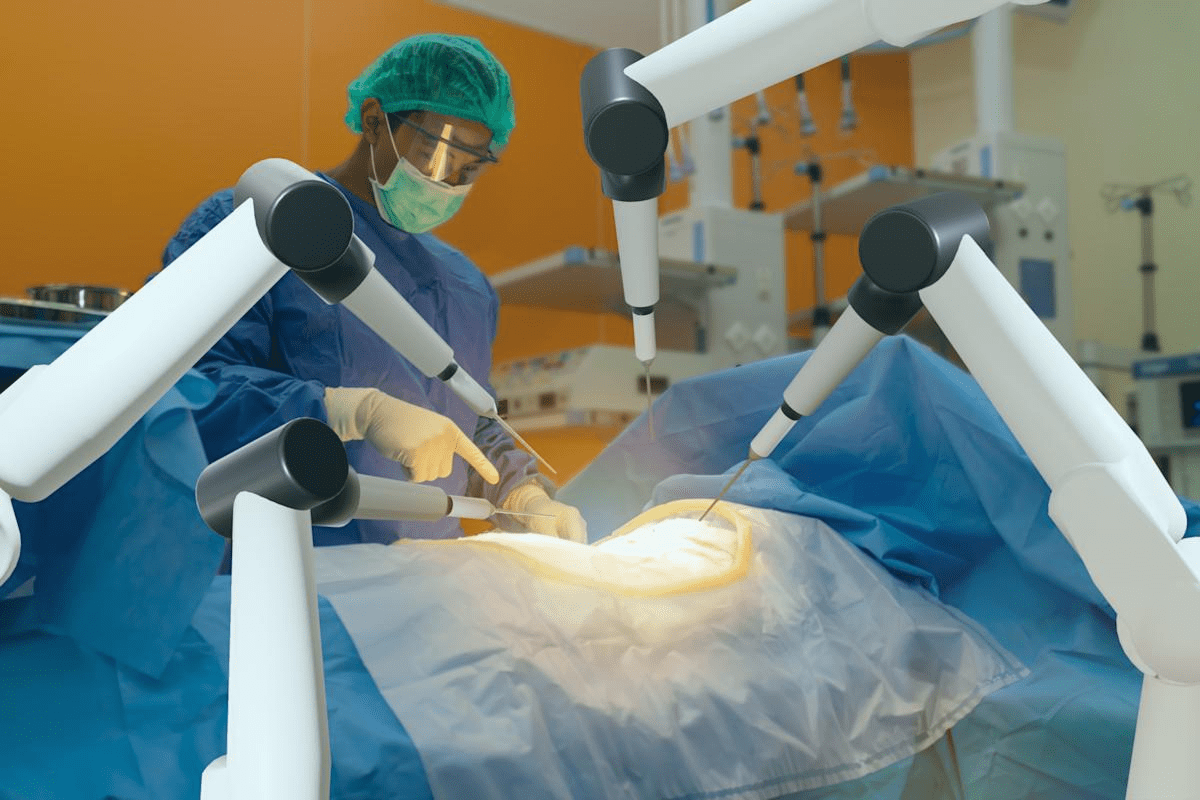
Choosing to have a mastectomy is a big decision. It involves knowing about the surgery, its types, and why it’s recommended. A mastectomy removes one or both breasts, either partially or fully. It’s often chosen for those with breast cancer or at high risk of getting it.
Types of Mastectomy Procedures
There are different mastectomy procedures, each for specific reasons and results. These include:
- Total (or Simple) Mastectomy: This removes the whole breast, including the nipple, areola, and most skin.
- Modified Radical Mastectomy: It takes out the breast tissue, the skin over the chest muscles, and usually the lymph nodes under the arm.
- Nipple-Sparing Mastectomy: This keeps the nipple-areola complex, helping to lessen the emotional impact of losing a nipple.
- Skin-Sparing Mastectomy: It removes the breast tissue but keeps as much skin as possible, making immediate reconstruction easier.
Reasons for Mastectomy
Mastectomy is mainly for treating breast cancer. It can also be a preventive choice for those at high risk due to genetic mutations like BRCA1 and BRCA2. The decision to have a mastectomy is personal and depends on many factors, like cancer stage, health, and personal wishes.
Post-Surgery Expectations
After a mastectomy, recovery involves managing pain and adjusting to changes in sensation. Some may experience phantom sensation or loss of normal sensation in the breast area. Knowing these possible outcomes helps manage expectations and aids in a smoother recovery. Post-surgical care and follow-ups are key to address any issues or concerns.
It’s also important for patients to know about reconstruction options after a mastectomy. This can be discussed with their healthcare provider. A dedicated care team plays a crucial role in supporting patients throughout their journey of mastectomy and recovery. They ensure patients get the right guidance and support throughout their treatment.
Importance of Arm Care After Surgery
Arm care is key after a mastectomy, affecting both healing and mobility. Patients must focus on arm care to avoid problems and ensure a smooth recovery.
Healing and Recovery Process
The healing process after a mastectomy is vital. Proper arm care is essential. We suggest a care plan with gentle exercises, wound care, and watching for complications.
As the third source advises, “Talk to your treatment team at your pre-surgical visit about what to expect.” This shows how important it is to understand the healing process and be ready for post-surgery care.
During recovery, patients might feel unexpected tightness or reconstruction disruption. These can affect their mobility and comfort. It’s important for patients to know about these issues and follow their treatment team’s advice on managing them.
Impact on Mobility and Function
Mastectomy surgery can greatly affect a patient’s mobility and function, mainly in the arm and shoulder. We help patients create a rehabilitation plan to address these changes. This helps them regain strength and motion.
By focusing on arm care and following a structured rehabilitation program, patients can reduce the risk of long-term mobility problems.
- Gentle exercises to improve flexibility and strength
- Proper wound care to promote healing
- Monitoring for signs of complications, such as infection or lymphedema
Common Arm Usage Restrictions Post-Mastectomy
Understanding the limits on arm use is essential for safe healing.
Limitations on Lifting and Reaching
One main rule is to limit lifting and reaching. Patients should not lift anything heavier than a gallon of milk for a few weeks after surgery. This rule helps avoid putting too much stress on the surgery area and lowers the risk of lymphedema or other issues.
Avoiding heavy lifting is very important in the early recovery days. This means not carrying heavy bags, lifting kids, or doing hard household tasks without support or doctor approval.
Avoiding Certain Movements
Patients also need to avoid certain movements that could harm healing. This includes not doing repetitive arm or shoulder actions on the surgery side. We stress the need for gentle, slow movements to keep flexibility without stressing the surgery area too much.
It’s very important to follow these guidelines to avoid problems like lymphedema, infection, or seroma. By being careful with their movements and sticking to the rules, patients can greatly lower their risk of these issues.
Duration of Restrictions
The length of time for arm usage restrictions varies. It depends on the mastectomy type, if there are drains, and the patient’s health. Usually, patients need to follow these rules for weeks to months after surgery. Drains might mean longer restrictions on certain activities.
We give each patient personalized advice on how long to follow these rules. We consider their unique situation and how they’re doing. Our goal is to support them through their recovery.
Role of Physiotherapy in Recovery
Physiotherapy plays a big role in the recovery after mastectomy. It helps create a full recovery plan. This plan meets both physical and emotional needs of patients.
Physiotherapy is key in the recovery after mastectomy. It helps regain arm strength and mobility. It also improves overall well-being by lowering the risk of complications and boosting quality of life.
Benefits of Physical Therapy
Physical therapy after mastectomy offers many benefits. Improved mobility and reduced stiffness are major advantages. These allow patients to use their arm again. It also helps manage pain and prevent lymphedema.
Physical therapy is also vital for fatigue recovery. It helps patients do daily activities with more energy and less pain.
Recommended Exercises
There are specific exercises recommended after mastectomy. These exercises help improve arm mobility and strength. They include:
- Gentle stretching exercises to loosen the shoulder and arm
- Arm elevation and rotation exercises to improve mobility
- Strengthening exercises using light weights or resistance bands
It’s important to work with a physiotherapist. They can create an exercise plan that fits your needs and progresses at the right pace.
When to Start Therapy
The right time to start physiotherapy varies. It depends on your health, the surgery’s extent, and your surgeon’s advice. We suggest starting with gentle exercises soon after surgery. More intense therapy can start once the wound heals enough, under a healthcare professional’s guidance.
Recognizing Signs of Complications
After a mastectomy, it’s important to watch your body’s recovery closely. Spotting complications early can greatly improve your healing. We’ll help you understand common issues and when to get medical help.
Common Post-Surgical Complications
Complications after a mastectomy can include incision sensitivity, swelling, or unexpected side effects. Knowing these signs is key to getting help quickly if needed.
Types of Complications
Some common issues are:
- Infection: Look for redness, swelling, or fever.
- Seroma: This is fluid buildup at the surgery site.
- Lymphedema: Swelling in the arm from lymph node removal.
When to Seek Medical Advice
If you notice unusual symptoms like more pain, swelling, or infection signs, get medical advice fast. Keep an eye on how your body reacts to surgery. Tell your healthcare provider about any worries.
| Complication | Signs and Symptoms | Recommended Action |
| Infection | Redness, swelling, fever | Contact your doctor immediately |
| Seroma | Fluid accumulation, swelling | Consult your healthcare provider |
| Lymphedema | Arm swelling, heaviness | Discuss with your doctor or a lymphedema specialist |
Knowing about possible complications and when to ask for help can improve your recovery. Always talk to your healthcare provider if you’re worried about your healing.
Psychological Impact of Arm Restrictions
Recovering from mastectomy is more than just healing physically. It also requires mental strength. Patients face emotional challenges due to arm restrictions, affecting their mental health.
Emotional and Mental Health Considerations
After mastectomy and arm restrictions, patients deal with many emotions. They might feel anxious, depressed, frustrated, or grieve for their body changes. It’s key to tackle these emotional hurdles as part of healing.
Common emotional and mental health issues include:
- Feelings of loss or grief over body image or function changes
- Anxiety about the future or fear of cancer coming back
- Depression or sadness about losing independence
- Frustration with physical limits and the recovery journey
Understanding the limits on arm use is essential for safe healing.
Support Systems and Resources
A strong support network is critical for coping with arm restrictions’ emotional impact. Patients should surround themselves with family, friends, and healthcare professionals. They offer emotional support and guidance during recovery.
Some helpful resources include:
- Professional counseling or therapy for emotional and mental health
- Support groups, online or in-person, to connect with others facing similar issues
- Information and resources to understand the condition and recovery
For some, emotional challenges may last, requiring ongoing counseling or support. We urge patients to actively seek help to overcome these hurdles.
By recognizing the psychological effects of arm restrictions and using available support, patients can manage the emotional side of recovery better.
Assessing Your Recovery Timeline
A dedicated care team plays a crucial role in supporting patients throughout their journey of mastectomy and recovery.
Factors Influencing Recovery Time
How long it takes to recover from a mastectomy can vary. The type of surgery, your health, and following your doctor’s advice are key. Patients who stick to their recovery plan often have an easier time getting better.
Important factors include:
- The extent of the surgery
- Presence of any complications
- Age and overall health of the patient
- Effectiveness of pain management
- Participation in physical therapy
Setting Realistic Rehabilitation Goals
Setting realistic goals for rehabilitation is vital. We help our patients set goals that fit their situation. This approach keeps them positive and helps the recovery go smoothly.
Women who have had a mastectomy say setting goals and celebrating small wins helps a lot. It boosts their mental and emotional health during recovery.
“Recovery is not just about physical healing; it’s also about mental resilience. Setting achievable goals helped me stay focused and positive throughout my journey.”
A survivor’s testimonial
Here’s a quick summary of what affects recovery time and setting goals:
| Factor | Influence on Recovery |
| Type of Surgery | Affects the extent of tissue removal and trauma to the body |
| Overall Health | Pre-existing health conditions can complicate recovery |
| Adherence to Care Instructions | Following post-surgical instructions is key for healing |
| Physical Therapy | Helps in regaining mobility and strength |
We will keep supporting our patients as they recover. We make sure they have the help and guidance they need to reach their rehabilitation goals.
Adjusting Daily Activities Post-Mastectomy
Recovering from mastectomy surgery means making big changes in your daily life. It’s important to plan carefully and adjust your routine to avoid pain and complications.
Modifying Household Tasks
Doing household chores can be tough after mastectomy. Try breaking tasks into smaller parts to avoid too much strain. For example, clean in short bursts with breaks in between.
Having family or friends help can also make things easier. Here are some tips:
- Avoid heavy lifting, bending, or stretching
- Use ergonomic tools to reduce strain
- Prepare meals ahead of time to cut down on kitchen time early on
| Task | Pre-Mastectomy | Post-Mastectomy Adjustment |
| Laundry | Wash, dry, fold, and iron in one session | Break into smaller tasks; consider having someone else do it |
| Cooking | Prepare complex meals daily | Simplify meals or prepare in advance; use pre-cut or pre-cooked ingredients |
| Cleaning | Clean the entire house in a day | Clean one room at a time; take regular breaks |
Strategies for Work and Leisure Activities
Going back to work and leisure activities needs careful planning. Talk to your employer about when you can start back, maybe with part-time hours or easier tasks.
For fun activities, think about these tips:
- Pick hobbies that don’t strain your arm or chest
- Stay away from activities that require heavy lifting or pushing
- Slowly add more activities as you feel more comfortable
It’s also key to manage bra discomfort and swelling unpredictability. Wear comfy, supportive bras and use compression clothes as your doctor suggests.
By adjusting your routine and listening to your body, you can make the recovery period easier.
Long-term Changes and Adaptations
After a mastectomy, patients face long-term changes that impact their daily lives. Adapting to these changes can be tough. But, with the right help, people can learn to live with these changes.
Persistent Effects on Arm Function
Some patients struggle with lasting arm mobility issues. This makes simple tasks hard. Gentle exercises and stretches can slowly improve arm function.
Embracing a New Normal
Adjusting to new life circumstances is a big step. People might need to find new hobbies and tasks. This helps them feel normal and fulfilled again.
It’s key to watch out for insurance surprises and have a support system. A partner can offer emotional support and help with daily tasks. Being proactive and prepared helps face the challenges of long-term changes after mastectomy.
FAQ
What are the common arm usage restrictions after mastectomy?
After mastectomy, patients are often told to avoid heavy lifting, bending, or stretching. This helps with healing and prevents complications. The specific rules depend on the surgery type and your recovery.
How long do arm usage restrictions last after mastectomy?
The time you must avoid using your arms varies. It depends on the surgery extent, if you have drains, and how fast you heal. Usually, it’s a few weeks, and your doctor’s advice is key.
What is the role of physiotherapy in recovery after mastectomy?
Physiotherapy is vital for getting your arm back to normal after mastectomy. A physical therapist will give you exercises to improve movement, reduce stiffness, and aid in recovery.
What are the signs of complications after mastectomy that I should watch out for?
Look out for increased pain, swelling, redness, or infection at the surgery site. Also, numbness or tingling is a red flag. If you notice these, get medical help right away.
How can I manage emotional and mental health after mastectomy?
To manage your emotional and mental health, talk to family, friends, or support groups. Consider counseling if needed. Remember to take care of yourself and give yourself time to adjust.
How do I assess my recovery timeline after mastectomy?
To track your recovery, watch your progress and adjust to new limits. Set realistic goals for your rehabilitation. Your recovery time depends on your health, surgery extent, and any complications.
What adjustments can I make to my daily activities after mastectomy?
After mastectomy, you might need to change how you do daily tasks. Take breaks, find new ways to do things, and prioritize tasks. Avoid heavy lifting and wear comfy clothes.
What are the long-term changes and adaptations I may experience after mastectomy?
You might face lasting effects on arm mobility and body image changes. Embrace new routines and seek support. This helps in adapting to these changes.
How can I manage bra discomfort and swelling after mastectomy?
For bra discomfort, choose comfy, supportive bras and consider prosthetics or breast forms. Swelling can be managed with elevation, compression, and gentle exercises as advised by your doctor.
What resources are available for support after mastectomy?
There are many resources for support after mastectomy. Healthcare providers, support groups, online forums, and counseling services offer emotional support and guidance. They help you navigate the challenges of mastectomy.
How can I deal with the emotional aftermath and body image shift after mastectomy?
To cope with emotional and body image changes, seek support and practice self-care. Allow time for adjustment. Focus on the positive aspects of recovery and the reasons for mastectomy.
What are the possible insurance surprises and partner adjustments I may face after mastectomy?
To avoid insurance surprises, understand your coverage and talk to your insurance provider. With partner adjustments, communicate openly about needs and challenges. Consider counseling together.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6514493/