It’s important to know the terms related to blood clotting and blood clots for proper diagnosis and treatment. At Liv Hospital, we focus on patient care and proven results. We will look at 11 key medical terms used by doctors for conditions like Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE). Learn 11 important medical word for blood clot and blood clots with clear, simple explanations.
The medical term for a blood clot is thrombus. It’s a solid mass made from blood platelets, proteins, and cells in a blood vessel or the heart. Knowing these terms helps international patients understand their treatment options.
Key Takeaways
- Understanding key medical terms related to blood clotting and blood clots.
- The term “thrombus” refers to a solid mass formed within a blood vessel or the heart.
- Conditions like DVT and PE are closely related to blood clotting.
- Accurate diagnosis relies on a clear understanding of medical terminology.
- Liv Hospital prioritizes patient-centered care and evidence-based outcomes.
Understanding Blood Clots and Their Importance
Blood clots are key to our body’s healing when injured. Yet, they can also pose serious health risks. The clotting process, or coagulation, is complex, involving many factors and pathways.
The Normal Blood Clotting Process
Blood clotting, or hemostasis, is vital to stop bleeding when a blood vessel is hurt. It starts with platelet activation and the coagulation cascade. This leads to a fibrin clot that seals the injury. Hemostasis balances procoagulant and anticoagulant factors, ensuring clots form only when needed.
When Blood Clotting Becomes Problematic
When hemostasis is off balance, it can cause issues. The body might not form clots when it should (hypocoagulability) or form too many clots (hypercoagulability). Hypercoagulability can lead to thrombophilia, making it easier to form blood clots. This can cause serious problems like deep vein thrombosis (DVT) or pulmonary embolism (PE).
It’s important to understand normal and abnormal clotting to diagnose and treat clotting disorders. Recognizing the role of blood clots and their risks helps healthcare professionals treat and prevent clotting-related issues.
Thrombus: The Medical Word for Blood Clot
In medical terms, a blood clot is called a ‘thrombus.’ It forms inside a blood vessel. Knowing about thrombus formation helps us understand heart and blood vessel diseases and their treatments.
Definition and Etymology
A thrombus is a blood clot in a blood vessel, in veins or arteries. The word ‘thrombus’ comes from the Greek “thrombos,” meaning ‘clump’ or ‘lump.’ This shows a thrombus that blocks blood flow.
How Thrombi Form in the Body
Thrombus formation starts with platelet activation and the coagulation cascade. These chemical reactions create a fibrin clot. This clot can block blood flow, causing serious health problems.
Venous thrombosis happens in veins, like deep vein thrombosis (DVT) in the legs. Arterial thrombosis occurs in arteries, leading to heart attacks or strokes if it blocks blood to vital organs.
It’s key to know how thrombi form and the difference between venous and arterial thrombosis. This knowledge helps in preventing and treating these conditions. Recognizing risk factors and symptoms lets doctors act early to avoid serious problems.
Coagulation: The Primary Blood Clotting Mechanism
Coagulation is a vital process that helps our bodies stop bleeding. When a blood vessel gets hurt, our body quickly forms a blood clot to prevent too much blood loss. This complex process involves many factors and pathways.
We will dive into the details of coagulation, focusing on the coagulation cascade and its factors. Knowing how our bodies stop bleeding when a vessel is damaged is key.
The Coagulation Cascade Explained
The coagulation cascade is a series of steps that lead to a fibrin clot. It has two main paths: the intrinsic and extrinsic pathways. These paths merge into the common pathway. The intrinsic pathway starts with damage inside the blood vessels and is more complex. The extrinsic pathway is triggered by damage outside the blood vessels.
Both paths lead to the activation of factor X. This then starts the common pathway, leading to thrombin and fibrin. Fibrin is key because it forms the clot that stops bleeding.
| Pathway | Description | Key Factors Involved |
| Intrinsic | Activated by internal vascular damage | Factors XII, XI, IX, VIII |
| Extrinsic | Triggered by external trauma | Factor VII, Tissue Factor |
| Common | Converges to form a fibrin clot | Factors X, II (Thrombin), I (Fibrinogen) |
Factors Affecting Coagulation
Many things can change how our blood clots, like our genes, medicines, and health. For example, people with hemophilia can’t clot properly because they lack certain factors. On the other hand, some conditions and medicines can make us more likely to form clots.
It’s important to understand these factors to manage blood clotting issues. By knowing how different things affect coagulation, doctors can better treat bleeding problems and clotting issues.
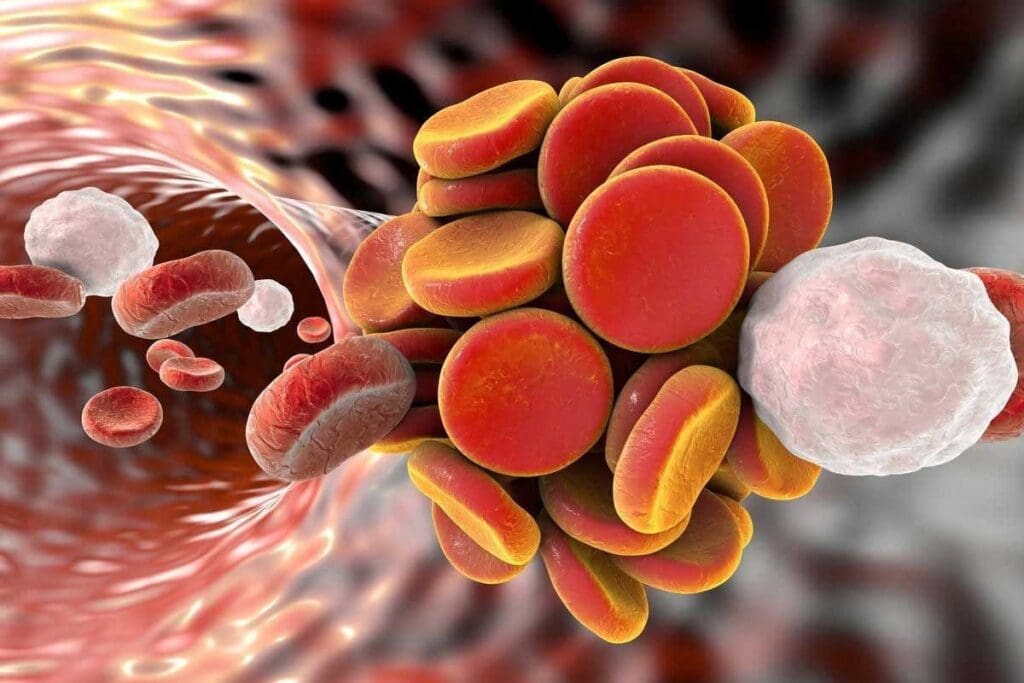
Thrombosis: When Blood Clots Form Within Blood Vessels
Thrombosis happens when blood clots form inside blood vessels. This can cause serious problems, like blocked blood flow and tissue damage. Knowing about thrombosis is key for preventing and treating it.
Types of Thrombosis
There are two main types of thrombosis: venous and arterial. Venous thrombosis forms in veins, often in the legs, known as deep vein thrombosis (DVT). Arterial thrombosis forms in arteries and can lead to heart attacks or strokes.
Risk Factors for Thrombosis
Many things can increase your risk of getting thrombosis. These include having had a clot before, certain genetic mutations, and other health issues. We’ll look at these in more detail.
Risk factors for thrombosis fall into three groups: genetic, acquired, and environmental.
- Genetic factors include mutations like Factor V Leiden and prothrombin G20210A.
- Acquired factors include age, obesity, and being immobile for a long time.
- Environmental factors include smoking and taking certain medicines.
| Risk Factor Category | Specific Risk Factors |
| Genetic | Factor V Leiden, Prothrombin G20210A |
| Acquired | Age, Obesity, Prolonged Immobilization |
| Environmental | Smoking, Certain Medications |
Understanding thrombosis and its risk factors helps us prevent and treat it. It’s important to spot the signs and symptoms early to avoid serious problems.
Deep Vein Thrombosis (DVT): Clots in the Deep Veins
When a blood clot forms in the deep veins, usually in the legs, it’s called Deep Vein Thrombosis (DVT). This condition needs quick medical care. DVT is serious and can cause severe problems if not treated right.
Symptoms and Diagnosis
DVT symptoms include swelling, pain, and redness in the affected limb. Sometimes, DVT has no symptoms, so knowing the risk factors is key. Doctors use an ultrasound to find and locate blood clots.
If you think you might have DVT, see a doctor right away. Early diagnosis is key to avoiding serious problems like pulmonary embolism.
Treatment Options
Treating DVT aims to stop the clot from getting bigger and breaking loose. This can cause a life-threatening pulmonary embolism. Doctors use anticoagulant medicines to prevent new Knowing about medical terms for clotting and DVT risks helps manage the condition better.
In severe cases, treatments like thrombolysis or vena cava filters might be needed. These are used when other treatments don’t work or when the case is very serious.
Pulmonary Embolism (PE): When Clots Travel to the Lungs
A blood clot traveling to the lungs can cause a serious medical emergency called Pulmonary Embolism. We will look at how it happens, its symptoms, and treatment options. Pulmonary Embolism is a serious issue that comes from Deep Vein Thrombosis (DVT). In DVT, a clot breaks loose and goes to the lungs.
Development from DVT
A clot in the deep veins, usually in the legs, is called Deep Vein Thrombosis. If this clot breaks loose, it can travel to the lungs. This can block blood flow to the lungs, causing serious health problems.
Recognizing and Treating Pulmonary Embolism
It’s important to know the symptoms of Pulmonary Embolism to get help quickly. Symptoms include shortness of breath, chest pain, and coughing up blood. If you have these symptoms and you’ve had DVT before, you need to see a doctor right away.
Treatment for Pulmonary Embolism often includes medicines to stop more clotting. In severe cases, medicines to dissolve the clot might be used. Sometimes, surgery is needed to remove the clot or fix lung damage.
Thrombogenesis: The Origin and Formation of Blood Clots
Learning about thrombogenesis helps us understand how blood clots form and their effects on our health. It’s the process our body uses to make blood clots. This is important to stop too much bleeding when we get hurt.
Factors Contributing to Thrombogenesis
Many things can lead to thrombogenesis. These include damage to the blood vessel lining, changes in blood flow, and a tendency for the blood to clot too much. Endothelial injury happens when the blood vessel lining gets damaged. This exposes collagen and tissue factor, starting the clotting process.
Changes in blood flow can also cause clots. This includes when blood flow is too turbulent or stops moving. Hypercoagulability makes blood more likely to clot. It can be caused by genetics, cancer, or some medicines.
Medical Conditions Associated with Abnormal Thrombogenesis
Some health issues can make thrombogenesis go wrong, raising the risk of blood clots. For example, cancer can cause more blood clots because of substances tumors produce.
Sepsis also messes with normal clotting, making clots more likely. Knowing about these conditions and how they affect thrombogenesis is key to managing and preventing blood clots.
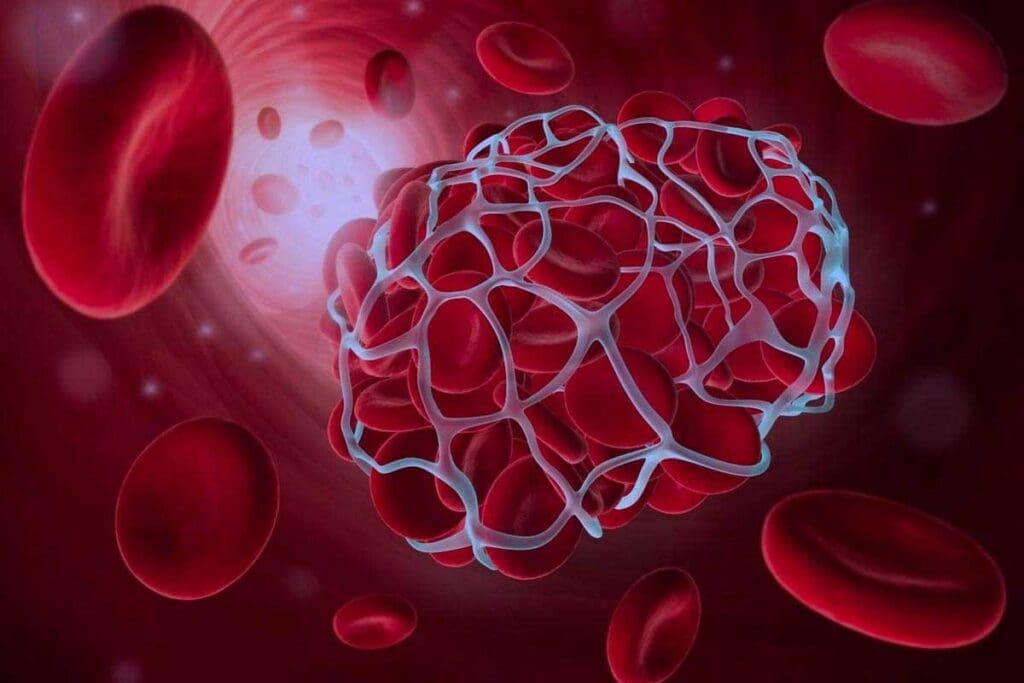
Embolism: When Blood Clots Travel Through the Bloodstream
A blood clot that breaks loose and travels through the bloodstream can cause an embolism. This can lead to severe health problems. An embolism happens when a clot, called an embolus, blocks a blood vessel. This blockage can cause serious issues, depending on where it occurs.
It’s important to know about the different types of emboli. This knowledge helps doctors diagnose and treat embolism better. We will look at these types and how they affect the body.
Different Types of Emboli
Emboli can be made of different materials, each with its own health risks. The most common types are:
- Thromboembolism: This happens when a blood clot (thrombus) breaks loose and travels through the bloodstream. It’s another term related to blood clotting, similar to another word for blood clotting or another name for blood clotting.
- Fat Embolism: This usually happens after a major injury, like a fracture, when fat globules get into the bloodstream.
- Air Embolism: This occurs when air bubbles get into the bloodstream, often during medical procedures.
Each type of embolism needs a different treatment plan. This shows why accurate diagnosis is so important.
Consequences of Embolism in Different Body Systems
The effects of an embolism vary based on where it lodges. For example:
| Location of Embolus | Potential Consequences |
| Lungs | Pulmonary Embolism (PE), potentially life-threatening |
| Brain | Stroke or Cerebral Embolism, leading to neurological deficits |
| Limbs | Ischemia or gangrene, potentially requiring amputation |
Knowing these effects is key for healthcare providers to manage embolism well. This helps reduce long-term damage. The medical term for a clot is closely related to embolism, as clots are a common cause of emboli.
In conclusion, embolism is a complex condition with various causes and effects. Recognizing the different types of emboli and their impacts on the body is essential for proper care.
Venous Thromboembolism (VTE): A Global Health Concern
Venous Thromboembolism (VTE) is a big health problem worldwide. It includes Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE). Every year, it affects hundreds of thousands of people, causing a lot of sickness and death.
Global Impact and Statistics
VTE is a major health issue that puts a big strain on healthcare systems everywhere. It leads to a lot of hospitalizations and deaths each year.
Here are some important statistics to show how big of a problem VTE is:
| Region | VTE Incidence Rate | Mortality Rate |
| North America | 1-2 per 1,000 adults annually | 10-30% within 1 month of diagnosis |
| Europe | 1-2 per 1,000 adults annually | 10-30% within 1 month of diagnosis |
| Asia | 0.5-1 per 1,000 adults annually | 15-40% within 1 month of diagnosis |
Prevention Strategies for High-Risk Individuals
Stopping VTE is key, mainly for those at high risk. This includes people who have had DVT or PE before, those having major surgery, and those with certain illnesses like cancer.
Prevention strategies include:
- Anticoagulation therapy: Using medicines to stop blood clots.
- Mechanical prophylaxis: Using devices like compression stockings or intermittent pneumatic compression devices.
- Mobility: Encouraging movement and exercise to improve blood flow.
By knowing the risks and using these prevention methods, we can lower VTE cases and its serious side effects.
Microclots and Their Role in COVID-19
Microclots in COVID-19 are a key area of study. They help us understand how the disease works. In severe cases, microclots play a big role.
Recent Research Findings
Studies show microclots are common in severe COVID-19. They can cause breathing problems and heart issues. The more microclots, the worse the disease seems to get.
Microclots are not just a side effect. They might actually help the disease spread. Scientists use special imaging to see and count these clots. This gives us clues about their role.
Implications for Treatment Approaches
Knowing about microclots changes how we treat COVID-19. Doctors can now focus on these clots to help patients. This could lead to better care.
Research is looking into using blood thinners to stop microclots. The table below shows what we’ve learned so far and how it might help treatment.
| Research Findings | Treatment Implications |
| Microclots are common in severe COVID-19 cases | Use of anticoagulant therapies to prevent microclot formation |
| Microclot formation is associated with disease severity | Targeted therapies to address microclots and reduce disease severity |
| Advanced imaging techniques can identify microclots | Early detection and treatment of microclots to improve patient outcomes |
Studying microclots in COVID-19 is very promising. It helps us understand the disease better and find new treatments. By keeping up with this research, we can give patients the best care possible.
Conclusion: The Importance of Understanding Blood Clot Terminology
Knowing the medical term for blood clot and related terms is key. It helps us understand the complex world of blood clotting. In this article, we’ve covered important terms and concepts.
When we understand these terms, we can better manage our health. Terms like thrombus, thrombosis, and embolism are vital. They help us grasp different medical conditions.
Good communication between doctors and patients depends on clear blood clot terms. Knowing these terms helps patients take charge of their health. It makes their healthcare journey better.
FAQ
What is the medical term for a blood clot?
A blood clot is called a thrombus. It forms inside a blood vessel.
What is the difference between thrombosis and embolism?
Thrombosis is when a clot forms in a blood vessel. Embolism is when a clot or particle travels and blocks a vessel.
What is Deep Vein Thrombosis (DVT)?
DVT is when a clot forms in the deep veins, usually in the legs. It’s serious and can cause big problems if not treated.
What is Pulmonary Embolism (PE)?
PE is a serious condition. It happens when a clot from DVT travels to the lungs.
What is Venous Thromboembolism (VTE)?
VTE includes DVT and PE. It’s a big health issue worldwide.
What is thrombogenesis?
Thrombogenesis is how blood clots start. It involves injury to the blood vessel and other factors.
What is the coagulation cascade?
The coagulation cascade is a series of steps leading to fibrin formation. Fibrin is key in blood clots.
What are the risk factors for thrombosis?
Risk factors for thrombosis include medical conditions, genetics, and lifestyle. These can increase the chance of blood clots.
How are blood clots treated?
Treatment for blood clots depends on the clot’s location and size. Anticoagulation therapy and mechanical methods are common.
What is the link between microclots and COVID-19?
Research shows microclots in severe COVID-19 cases. This suggests a link between microclots and disease severity.
What is hemostasis?
Hemostasis is the body’s normal clotting process. It prevents too much bleeding and keeps blood vessels intact.
What is thrombophilia?
Thrombophilia is when blood clotting gets out of balance. It increases the risk of blood clots.
References:
- Tripathi, A. K., & Lappin, D. (2025). Laboratory evaluation of acute leukemia. StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK611988/





