Last Updated on November 27, 2025 by Bilal Hasdemir

Learning about meningioma brain tumors is key for those dealing with these common tumors. We aim to give you all the facts you need. This includes what they are, how common they are, and where they usually occur.
Meningioma brain tumors make up to 37.6 percent of primary central nervous system tumors. They are also about half of all benign brain tumors. At Liv Hospital, we know how vital expert care is for these conditions.
Our team is known worldwide for caring for patients. By knowing about meningioma brain tumors, patients can make better choices about their care.
Key Takeaways
- Meningioma brain tumors are the most common primary central nervous system tumors.
- They represent up to 37.6 percent of such tumors.
- Understanding their characteristics and locations is crucial for effective diagnosis and treatment.
- Liv Hospital provides internationally respected, patient-focused care.
- Expert diagnosis and treatment can significantly impact patient outcomes.
What Are Meningioma Brain Tumors?

Meningiomas are tumors that grow from the meninges. These are the protective layers around the brain and spinal cord. They can be either benign or malignant.
Definition and Origin in the Meninges
Meningiomas start from the meninges, which have three layers. Most come from the arachnoid mater. These tumors can differ a lot in how they affect people.
Benign vs. Malignant Meningiomas
Most meningiomas are benign, meaning they are not cancerous. But, 1-3 percent can be malignant, which means they could be cancerous. Benign ones grow slowly and might not cause symptoms right away. Malignant ones grow faster and can spread to other brain areas.
“The distinction between benign and malignant meningiomas is crucial for determining the appropriate treatment and prognosis.”
| Type | Characteristics | Prognosis |
|---|---|---|
| Benign Meningioma | Slow-growing, non-cancerous | Generally favorable with appropriate treatment |
| Malignant Meningioma | Rapidly growing, potentially cancerous | More guarded, requires aggressive treatment |
Common Terminology and Alternate Spellings
Meningiomas are also known as meninggioma, meninigioma, meniingioma, and meninginoma. Knowing these names helps doctors and patients talk clearly.
Understanding meningiomas helps patients and their families deal with diagnosis and treatment. It lets them make informed choices about their health.
Prevalence and Demographics of Meningiomas

Meningiomas are a common type of brain tumor. Knowing about their prevalence and demographics helps both patients and healthcare providers. These tumors are usually benign and grow from the meninges, which protect the brain and spinal cord.
Frequency Among Brain Tumors
Meningiomas are a major concern in adults. They make up about 30% of all primary brain tumors. The Central Brain Tumor Registry of the United States (CBTRUS) says they are the most common benign intracranial tumor.
Here’s how meningiomas compare to other brain tumors:
| Tumor Type | Frequency (%) |
|---|---|
| Meningiomas | 30% |
| Glioma | 25% |
| Pituitary Tumors | 15% |
Age and Gender Distribution
Meningiomas mostly affect adults over 60. The risk of getting meningiomas goes up after the age of 50. Women are twice as likely as men to get these tumors.
A study in the Journal of Neuro-Oncology found:
“The age-adjusted incidence rate of meningiomas is higher in women than in men, with a female-to-male ratio of approximately 2:1. The incidence peaks in the 7th and 8th decades of life.”
Genetic and Environmental Risk Factors
What causes meningiomas is still being studied. But we know some risk factors. Ionizing radiation and genetic conditions like Neurofibromatosis type 2 (NF2) can increase the risk.
We’re still learning about the genetic and environmental factors that lead to meningiomas. Understanding these can help us diagnose and treat them better.
12 Essential Facts About Meningioma Brain Tumors and Their Most Common Locations
Meningioma brain tumors are complex. They grow from the meninges, which protect the brain and spinal cord. Knowing about these tumors helps in understanding their diagnosis and treatment.
Key Facts About Tumor Biology and Growth
Meningiomas grow slowly and are mostly benign. About 80-90% are WHO Grade I, meaning they grow slowly and rarely spread. This makes them less dangerous than other tumors.
Some meningiomas stay small for years, while others grow and cause symptoms. The reasons for their growth are still a mystery. Hormones, genetics, and environment might play a part.
Important Facts About Prevalence and Demographics
Meningiomas are the most common brain tumors in adults, making up 30-40% of all primary brain tumors. Women get them more often than men, with a 2:1 to 3:1 female-to-male ratio. Most cases happen between 40 and 70 years old.
Genetic conditions like Neurofibromatosis Type 2 (NF2) raise the risk. Childhood radiation exposure also increases the risk. But, the exact causes of meningiomas are still unknown.
Critical Facts About Tumor Locations and Their Significance
The location of a meningioma affects its symptoms and treatment. Most meningiomas are found on the convexity of the brain. Left frontal convexity meningiomas are common and can cause specific symptoms.
Posterior fossa meningiomas are at the base of the skull. They can press on important brain areas, causing serious problems. Knowing where a meningioma is helps doctors plan the best treatment.
“The location of meningiomas plays a significant role in their clinical presentation and management. Understanding these tumors’ characteristics is essential for providing optimal care.”
In summary, meningioma brain tumors are complex. Their biology, prevalence, demographics, and locations all matter. By knowing these 12 essential facts, doctors and patients can better handle these tumors.
Common Locations of Meningioma Brain Tumors
Meningioma brain tumors can happen in different parts of the brain. Some areas are more likely to have these tumors. Knowing where meningiomas usually occur helps doctors diagnose and plan treatment.
Convexity Meningiomas: The Most Common Site
Convexity meningiomas are very common. They grow on the outer brain surface. Because of their location, they can grow big before causing symptoms.
Key characteristics of convexity meningiomas include:
- They are often superficial and can be easily accessed for surgical removal.
- Symptoms may include headaches, seizures, and neurological deficits depending on their location and size.
- Convexity meningiomas are typically benign and have a good prognosis with appropriate treatment.
Left Frontal Convexity Meningiomas
Left frontal convexity meningiomas are a subtype of convexity meningiomas. They are found in the frontal brain area. These tumors can impact brain functions like thinking and movement.
Common symptoms of left frontal convexity meningiomas include:
- Personality changes or cognitive impairments.
- Motor weakness or paralysis on the right side of the body.
- Speech difficulties if the tumor is located in or near Broca’s area.
Posterior Fossa Meningiomas
Posterior fossa meningiomas are found in the brain’s lower back part. They are near the brainstem and cerebellum. Treating these tumors can be hard because of their location.
Symptoms of posterior fossa meningiomas may include:
- Dizziness or loss of balance.
- Hearing loss or tinnitus.
- Coordination and gait disturbances.
Other Notable Locations
While convexity meningiomas are common, tumors can also appear in other spots. This includes the skull base, sphenoid wing, and along the optic nerve sheath.
Other notable locations and their associated symptoms:
- Skull base meningiomas: Can cause cranial nerve deficits and affect vital functions.
- Sphenoid wing meningiomas: May lead to proptosis, double vision, or facial pain.
- Optic nerve sheath meningiomas: Can result in visual disturbances or loss.
Signs and Symptoms of Meningioma Brain Tumors
It’s important to know the signs and symptoms of meningioma brain tumors early. This helps in early detection and treatment. Meningiomas can cause different symptoms because of their location and size.
General Symptoms and Warning Signs
Meningioma brain tumors can show various symptoms. These include headaches, seizures, and neurological problems. Headaches are common, often due to increased pressure in the brain.
Other symptoms may be:
- Weakness or numbness in the arms or legs
- Vision changes, such as double vision or loss of peripheral vision
- Difficulty with speech or understanding language
- Cognitive changes, including memory loss or confusion
Location-Specific Symptoms
The symptoms of meningioma can vary based on the tumor’s location. For instance:
| Tumor Location | Possible Symptoms |
|---|---|
| Frontal Lobe | Personality changes, weakness on one side of the body |
| Temporal Lobe | Seizures, memory problems, difficulty with language |
| Cerebellum | Coordination problems, balance issues, double vision |
Knowing these location-specific symptoms is key to diagnosing and treating meningiomas well.
When to Seek Medical Attention
If you or someone you know has symptoms that could be from a meningioma, get medical help. Early diagnosis and treatment can greatly improve outcomes.
Be aware of sudden changes in your condition. This includes severe headaches, new neurological problems, or seizures. Tell your healthcare provider right away.
Diagnosis and Imaging of Meningiomas
Diagnosing meningiomas involves several steps. First, we assess the patient’s condition. Then, we use advanced imaging and histological tests. Accurate diagnosis is key to choosing the right treatment and improving patient care.
Initial Assessment and Physical Examination
The first step is a detailed initial assessment and physical exam. We look at the patient’s medical history and symptoms. We also do a neurological exam to find any issues. This helps us decide if more tests are needed.
Advanced Imaging Techniques (MRI, CT, PET)
Advanced imaging is crucial for diagnosing meningiomas. Magnetic Resonance Imaging (MRI) is often the first choice because it’s very sensitive. It gives detailed images of soft tissues. Computed Tomography (CT) scans are useful for finding calcifications in tumors. Positron Emission Tomography (PET) scans help understand tumor metabolism and tell if the meningioma is benign or malignant.
The choice of imaging depends on the tumor’s location, size, and the patient’s health. By combining data from different scans, we get a full picture of the tumor.
Biopsy and Histological Classification
Imaging gives us clues, but a biopsy and histological exam confirm the diagnosis. A biopsy takes a tumor sample for microscopic analysis. The World Health Organization (WHO) grades meningiomas based on their features. Grade I is benign, while Grades II and III are more aggressive.
Understanding the tumor’s type is vital for treatment planning. By knowing the tumor’s characteristics, we can tailor a treatment plan that meets the patient’s needs.
Treatment Options for Meningioma Brain Tumors
Treating meningioma brain tumors depends on several factors. These include the tumor’s location, size, and how it looks under a microscope. We will look at the different ways to treat these tumors, so you understand all your options.
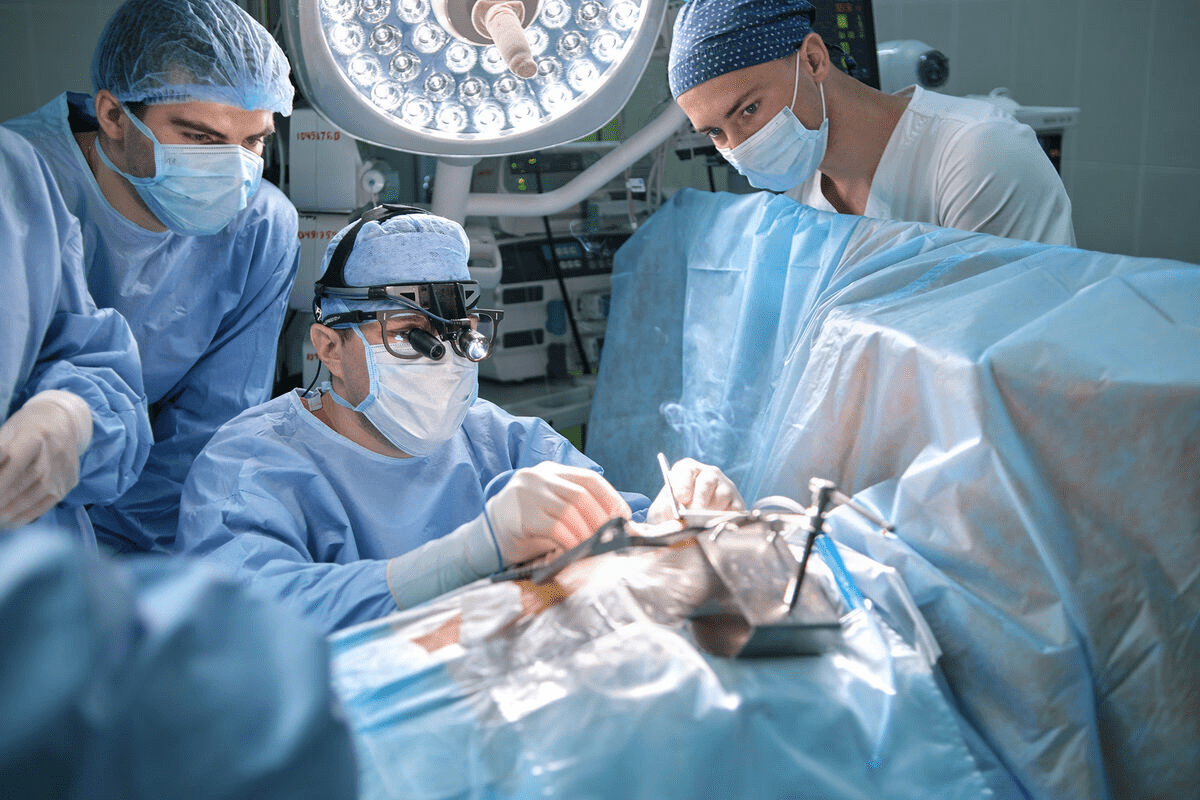
Surgical Approaches and Techniques
Surgery is often the first step in treating meningiomas. This is especially true for tumors that cause symptoms or grow. The goal is to remove the tumor completely, if it’s safe to do so, without harming the brain.
New techniques in neurosurgery have made surgery safer and more effective. These include:
- Microsurgical techniques for precise tumor removal
- Intraoperative imaging to ensure complete resection
- Neurophysiological monitoring to protect critical brain areas
Radiation Therapy and Radiosurgery
For some meningiomas, especially those hard to remove or in sensitive areas, radiation therapy or radiosurgery might be needed. These treatments use high-energy beams to kill tumor cells.
There are different types of radiation therapy, including:
- Stereotactic radiosurgery (SRS) for precise, high-dose radiation
- Fractionated stereotactic radiotherapy (FSRT) for delivering radiation in multiple sessions
- Intensity-modulated radiation therapy (IMRT) for shaping the radiation beam to the tumor
Medication and Emerging Treatments
While surgery and radiation are key, research is ongoing for new treatments. This includes medicines and treatments that target specific tumor characteristics.
Treatment Selection Based on Tumor Location
The location of the meningioma is very important in choosing treatment. For tumors near important areas, doctors might choose more careful approaches to avoid damage.
| Tumor Location | Common Treatment Approaches |
|---|---|
| Convexity | Surgery, potentially followed by observation or radiation |
| Skull Base | Surgery, radiation therapy, or a combination of both |
| Posterior Fossa | Surgery, potentially with radiation for residual tumor |
It’s important to know all the treatment options for meningioma brain tumors. This helps in making informed decisions about care. We work with patients to create personalized plans that meet their unique needs.
Living with Meningioma: Prognosis and Quality of Life
The outlook for meningioma patients depends on several important factors. These include the tumor’s type and how well treatment works. Knowing these details helps patients understand their diagnosis and treatment plan.
Factors Affecting Prognosis
Many things can affect a meningioma patient’s prognosis. These include the tumor’s grade, size, and where it is, as well as the patient’s health and age. Tumors that are benign (Grade I) usually have a better outlook than atypical (Grade II) or malignant (Grade III) ones.
How well the first treatment works is also key. Patients who have all of their tumor removed tend to do better than those with some left behind.
Recurrence Rates and Long-term Monitoring
How often meningiomas come back depends on their grade and how much of the tumor was removed. Benign meningiomas that are fully removed have a lower chance of coming back than atypical or malignant ones. It’s important to keep up with regular imaging, like MRI, to catch any return early.
Even patients with benign tumors need to be monitored over time. How often they need imaging checks depends on their tumor and health.
Coping Strategies and Support Resources
Dealing with meningioma is not just about medical treatment. It’s also about handling the emotional and mental side of the diagnosis. Support groups, counseling, and educational resources are key in helping patients and their families.
It’s important for patients to find support, like online forums, local groups, and counseling. These can offer valuable advice, emotional support, and tips on managing the condition and improving life quality.
By understanding their prognosis, staying on top of long-term monitoring, and using available support, meningioma patients can manage their condition well. This helps them maintain a good quality of life.
Conclusion
Meningioma brain tumors are a big deal because they’re common and can affect people’s lives a lot. Even though most are not cancerous, they can still cause health problems. This depends on where and how big they are.
We’ve talked about important facts about meningioma brain tumors. This includes what they are, how common they are, where they usually grow, and how to tell if you have one. We also looked at how to diagnose and treat them, and what the future might hold.
In short, meningiomas are usually not cancerous but can still be a big deal. Knowing about them and catching them early is key to managing them well. We believe more research and teaching patients is needed to help those with meningiomas.
We hope this detailed look at meningioma brain tumors has helped. We want to make sure readers know how to deal with diagnosis and treatment. This should help improve care and support for those affected.
FAQ
What is a meningioma brain tumor?
A meningioma is a tumor that grows in the meninges. These are protective membranes around the brain and spinal cord. Most are benign, but some can be malignant.
What are the common locations of meningioma brain tumors?
Meningiomas often appear in the brain’s convexity, especially in the frontal, parietal, and temporal areas. They also show up in the sphenoid wing, olfactory groove, and posterior fossa.
What are the symptoms of a meningioma brain tumor?
Symptoms vary based on the tumor’s location and size. Common signs include headaches, seizures, and weakness or numbness in limbs. Vision changes and cognitive issues are also common. Some people may not notice symptoms until the tumor grows a lot.
How are meningioma brain tumors diagnosed?
Diagnosis involves imaging tests like MRI, CT, and PET scans. A biopsy confirms the tumor’s type and grade. A detailed medical history and physical exam are also key.
What are the treatment options for meningioma brain tumors?
Treatment varies based on the tumor’s size, location, and grade. Options include surgery, radiation therapy, or radiosurgery. Sometimes, just watching the tumor is recommended.
Can meningioma brain tumors recur?
Yes, meningiomas can come back, even if they’re benign. The risk depends on the tumor’s grade and how much was removed during surgery. Regular check-ups are important to catch any recurrence.
What is the prognosis for someone with a meningioma brain tumor?
The prognosis varies by tumor grade, size, and location, and the person’s health. Benign meningiomas usually have a good outlook. Malignant ones need more aggressive treatment and have a worse prognosis.
Are there any risk factors for developing a meningioma brain tumor?
While causes are not fully known, some factors may increase risk. These include radiation exposure, genetic predisposition, and hormonal influences. Women are more likely to get meningiomas than men.
Can meningioma brain tumors be prevented?
There’s no known way to prevent meningiomas. But, knowing the risk factors and living a healthy lifestyle might help lower the risk.
What are the differences between benign and malignant meningiomas?
Benign meningiomas grow slowly and are non-cancerous. Malignant ones are cancerous and grow faster. The tumor’s grade determines the prognosis and treatment plan.
How do meningiomas affect quality of life?
The impact on quality of life depends on the tumor’s location, size, and symptoms. Treatment and management can help reduce symptoms and improve well-being.
What are convexity meningiomas?
Convexity meningiomas occur on the brain’s surface, often in the frontal, parietal, or temporal regions. They can cause seizures, weakness, and cognitive problems.
What are posterior fossa meningiomas?
Posterior fossa meningiomas happen in the brain’s lower back, near the cerebellum and brainstem. They can lead to balance issues, hearing loss, and trouble swallowing.