Myeloproliferative neoplasms (MPN) are rare blood cancers. They cause too many blood cells to be made. Getting diagnosed with MPN can change your life. It’s important to know about the treatment options to manage it well.
There are many ways to treat MPN, like chemotherapy, targeted therapy, and managing symptoms. Whether or not to use chemotherapy depends on several things. These include the type of MPN, the patient’s health, and how the disease is progressing.
Key Takeaways
- Understanding MPN and its subtypes is key to finding the right treatment.
- Chemotherapy is one of the many ways to manage MPN.
- Deciding on chemotherapy depends on the disease and the patient’s health.
- Targeted therapy and symptom management are other options, or can be used together.
- Knowing what to do is important for managing MPN well.
What Are Myeloproliferative Neoplasms (MPNs)?
Myeloproliferative neoplasms (MPNs) are a group of blood disorders. They have become a big focus in medicine. These conditions cause too many blood cells to be made, leading to health issues.
Definition and Classification of MPNs
MPNs are diseases that affect the bone marrow. They cause too many blood cells to be made. Doctors sort them out based on the type of blood cell and genetic changes.
Common Types: ET, PV, and Primary Myelofibrosis
The main types of MPNs are Essential Thrombocythemia (ET), Polycythemia Vera (PV), and Primary Myelofibrosis. ET makes too many platelets. PV makes too many red blood cells. Primary Myelofibrosis scars the bone marrow.
Prevalence and Risk Factors
MPNs are rare diseases. Each type has its own rate of occurrence. Risk factors include genetic changes, age, and environmental exposures.
| MPN Type | Prevalence | Common Symptoms |
| Essential Thrombocythemia (ET) | 1-2.5 per 100,000 | Blood clots, thrombosis |
| Polycythemia Vera (PV) | 1-3 per 100,000 | Headaches, dizziness, itching |
| Primary Myelofibrosis | 0.5-1.5 per 100,000 | Fatigue, anemia, enlarged spleen |
The Biology Behind Myeloproliferative Disorders
Myeloproliferative neoplasms (MPNs) start with genetic changes that mess with bone marrow. Knowing how these changes affect bone marrow is key to understanding MPNs. It helps us manage the disease better.
Bone Marrow Function and Blood Cell Production
Bone marrow is the spongy part of bones that makes blood cells. It has stem cells that turn into different blood cells. In healthy people, this process is well-controlled.
In MPNs, this control is lost. This leads to too many blood cells being made.
Blood cell production is complex. It involves many growth factors and cytokines working together. In MPNs, genes like JAK2, CALR, and MPL get mutated. This messes up the process, causing too many blood cells.
Genetic Mutations in MPNs
Genetic changes are key in MPNs. The most common changes are in JAK2, CALR, and MPL genes. These changes start a chain of events that makes cells grow and live longer than they should.
“The discovery of the JAK2 V617F mutation has revolutionized our understanding of MPNs, providing a molecular basis for the diagnosis and classification of these disorders.” –
A leading researcher in the field of MPNs
The Role of JAK2, CALR, and MPL Mutations
The JAK2 V617F mutation is common in MPNs, like polycythemia vera (PV). It changes the JAK2 protein, making it always active. This leads to too many blood cells.
CALR and MPL mutations are also important. They are found in essential thrombocythemia (ET) and primary myelofibrosis (PMF). These mutations also start the same signaling pathways as the JAK2 mutation.
| Gene | Mutation Type | Associated MPN |
| JAK2 | V617F | PV, ET, PMF |
| CALR | Insertion/Deletion | ET, PMF |
| MPL | Various | ET, PMF |
Knowing the genetic changes in an MPN can help a lot. It gives clues about the disease and helps choose the right treatment.
Recognizing MPN Symptoms and Diagnosis
Getting a correct diagnosis for MPNs is key to good treatment and better health. Myeloproliferative Neoplasms (MPNs) cause too many blood cells to be made. This leads to symptoms and health problems.
Common Symptoms Across MPN Types
MPN symptoms can differ from person to person. Yet, some symptoms are common across types like Essential Thrombocythemia (ET), Polycythemia Vera (PV), and Primary Myelofibrosis. These include fatigue, weight loss, and splenomegaly (a big spleen).
ET patients might face thrombosis or bleeding because of too many platelets. PV patients often have headaches, dizziness, and itching after bathing. Primary Myelofibrosis can cause bone pain and severe fatigue from anemia.
Diagnostic Tests and Procedures
To diagnose MPNs, doctors use blood tests, bone marrow biopsy, and sometimes genetic testing. Blood tests check blood cell counts and look for oddities.
- Complete Blood Count (CBC): Checks red, white blood cells, and platelets.
- Bone Marrow Biopsy: Looks at bone marrow cells and fibrosis.
- Genetic Testing: Finds mutations like JAK2, CALR, or MPL in MPNs.
Understanding Your Blood Work Results
It’s important to understand your blood work results for MPN diagnosis and care. Key things to look at include:
- Hemoglobin and Hematocrit: Shows red blood cell amount.
- White Blood Cell Count: Checks for too many white blood cells.
- Platelet Count: Looks at platelet levels.
Your doctor will look at these results with your symptoms and other tests to make a diagnosis.
When Is Chemotherapy Necessary for MPNs?
Figuring out when chemotherapy is needed for myeloproliferative neoplasms (MPNs) is complex. It depends on many factors that guide treatment choices.
Risk Stratification and Treatment Decisions
Risk stratification is key in deciding if chemotherapy is needed for MPN patients. It looks at how likely the disease is to get worse and the patient’s health. Important factors include age, genetic mutations, and past blood clots.
- Age: Older patients are seen as higher risk.
- Genetic mutations: Certain mutations, like JAK2, CALR, or MPL, affect risk.
- Previous thrombotic events: Blood clots increase risk.
High-Risk Patient Profiles
High-risk patients face a greater chance of disease worsening or blood clots. Chemotherapy might be suggested to lower these risks. High-risk groups often have:
- Advanced age
- History of blood clots
- High white blood cell count at start
- High-risk genetic mutations
Disease Progression Indicators
Watching for disease progression signs is vital in managing MPNs. Signs that might mean chemotherapy is needed include:
- Increasing spleen size
- Rising white blood cell counts
- New symptoms or worsening of old ones
- Turning into a more aggressive phase, like myelofibrosis or acute myeloid leukemia
Chemotherapy for MPNs is customized based on the patient’s risk and disease details. Knowing what influences treatment choices helps patients and doctors make the best decisions.
Traditional Chemotherapy Options for MPNs
Chemotherapy is a key part of treating MPNs. It offers different drugs to manage the disease. The choice of drug depends on the type of MPN, the patient’s risk, and their health.
Hydroxyurea: The Most Common Cytoreductive Therapy
Hydroxyurea is a common treatment for MPNs. It’s used for patients with high-risk features or high blood cell counts. It stops DNA synthesis but doesn’t affect RNA or protein, reducing blood cell production in the bone marrow.
Guidelines say hydroxyurea is a first-line treatment for some MPN patients. It helps control high blood cell counts. But, it’s important to watch for side effects like myelosuppression and mucocutaneous toxicity.
“Hydroxyurea has been a mainstay in the treatment of MPNs, providing a relatively well-tolerated option for managing disease-related complications.”
Busulfan and Other Alkylating Agents
Busulfan is used for MPN patients who can’t take hydroxyurea. It’s an alkylating agent that damages cancer cells’ DNA, stopping them from reproducing.
Busulfan can be effective but has a higher risk of myelotoxicity and secondary malignancies than hydroxyurea. It’s used in specific cases where the benefits are greater than the risks.
| Chemotherapy Agent | Primary Use in MPNs | Notable Side Effects |
| Hydroxyurea | Cytoreductive therapy for high-risk patients | Myelosuppression, mucocutaneous toxicity |
| Busulfan | Alternative for hydroxyurea-resistant patients | Myelotoxicity, secondary malignancies |
Expected Outcomes with Chemotherapy
Chemotherapy outcomes in MPNs depend on the drug, patient, and disease. It aims to lower thrombotic risks, control symptoms, and slow disease progression.
For many, chemotherapy improves quality of life and lowers MPN complications. But it’s important to consider the benefits and risks. Discuss these with a healthcare provider.
Myeloproliferative Disorder Treatment Approaches
MPN treatment is tailored to each patient. It uses a risk-adapted strategy that looks at the patient’s specific needs and disease. This ensures the right care for each person.
Risk-Adapted Treatment Strategy
A risk-adapted strategy for MPNs looks at the patient’s risk level. It considers the MPN type, age, and risk factors for disease progression or blood clots.
The goal is to find the best treatment balance. This aims to improve patient outcomes while minimizing risks and side effects.
| Risk Category | Typical Treatment Approach | Goals of Treatment |
| Low-Risk | Watch and wait or low-intensity treatments | Monitor disease progression, manage symptoms |
| High-Risk | Cytoreductive therapy, targeted treatments | Reduce risk of complications, manage symptoms |
Watch and Wait Approach for Low-Risk Patients
Low-risk patients might follow a watch-and-wait approach. This means regular checks without starting aggressive treatments right away.
This method is based on the idea that low-risk patients are less likely to have disease progression or complications soon.
When Active Treatment Becomes Necessary
Active treatment is needed when a patient’s risk changes or symptoms can’t be managed by watchful waiting. This might include cytoreductive therapies like hydroxyurea or targeted treatments to reduce disease complications.
The choice to start active treatment depends on the patient’s unique situation and disease characteristics.
Polycythemia Vera: Beyond Chemotherapy
Managing polycythemia vera requires more than just chemotherapy. This condition causes too many red blood cells, raising the risk of blood clots and other problems.
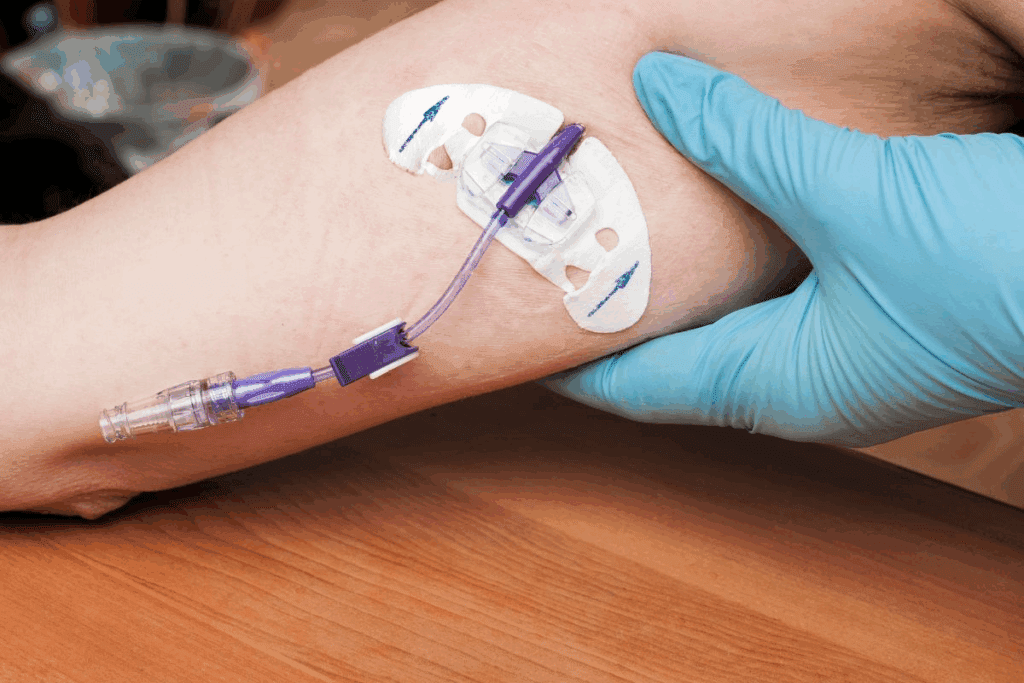
Phlebotomy as First-Line Treatment
Phlebotomy is key in treating polycythemia vera. It removes blood to lower red blood cell counts. This helps prevent blood clots and relieves symptoms.
How often phlebotomy is needed varies. It depends on the patient’s blood levels, health, and how well they respond to treatment. Regular checks are important to adjust phlebotomy as needed.
Low-Dose Aspirin for Thrombosis Prevention
Low-dose aspirin is also used to prevent blood clots in polycythemia vera patients. It stops platelets from sticking together, which lowers clot risk. Studies show it’s effective without increasing major bleeding risk.
Choosing to use low-dose aspirin depends on the patient’s risk factors. It’s important to monitor closely to ensure its benefits outweigh risks.
Non-Chemotherapy Cytoreductive Options
Some patients need more treatments to control blood cell counts. Options include interferon alpha and hydroxyurea alternatives. These aim to reduce blood cell production without chemotherapy.
- Interferon alpha helps by cutting down on red and platelet production.
- New treatments are being explored for polycythemia vera management.
These alternatives offer hope for those who can’t or won’t take traditional treatments. They provide a tailored approach to managing polycythemia vera.
Primary Myelofibrosis: Modern Treatment Options
Understanding the modern treatment landscape for primary myelofibrosis is key to effective disease management. This condition is complex, with scar tissue buildup in the bone marrow. It leads to anemia, spleen enlargement, and other issues.
Symptom-Directed Treatment Approaches
Symptom-directed treatment is a mainstay in managing primary myelofibrosis. It aims to ease symptoms and improve quality of life. Medications and therapies are tailored to address specific symptoms, such as anemia, spleen enlargement, or fatigue.
“The goal is to make patients feel better and live longer,” said a leading expert in myeloproliferative neoplasms. Effective symptom management can significantly enhance a patient’s quality of life.
JAK Inhibitors for Symptom Relief
JAK inhibitors have changed the game in treating primary myelofibrosis by providing significant symptom relief. Ruxolitinib, a JAK1/JAK2 inhibitor, is noted for its ability to reduce spleen size and alleviate symptoms such as night sweats and itching. Other JAK inhibitors, like fedratinib and pacritinib, offer more options for patients, even those who can’t tolerate ruxolitinib.
- Ruxolitinib: Reduces spleen size and improves symptoms
- Fedratinib: Offers an alternative for patients intolerant to ruxolitinib
- Pacritinib: Shows promise in patients with thrombocytopenia
When Chemotherapy May Be Indicated
Even with the progress in targeted therapies like JAK inhibitors, chemotherapy might be needed for some patients with primary myelofibrosis. Chemotherapy can be useful in managing disease progression or in preparing for stem cell transplantation. Hydroxyurea is often used to control white blood cell counts and reduce thrombosis risk.
“Chemotherapy remains a valuable tool in the treatment arsenal for primary myelofibrosis, particularly in specific clinical scenarios,” notes highlighting the importance of a tailored treatment approach.
Stem Cell Transplantation: The Only Curative Option
Stem cell transplantation is the only cure for some MPN patients. It replaces the sick bone marrow with healthy stem cells. This could cure some patients.
Candidate Selection for Transplant
Choosing to get a stem cell transplant depends on several things. These include the patient’s health, the type of MPN, and high-risk features. Patients with primary myelofibrosis often get transplanted because it’s aggressive.
Key factors in candidate selection include:
- Disease severity and risk stratification
- Presence of specific genetic mutations
- Patient’s age and overall health status
- Previous treatment responses
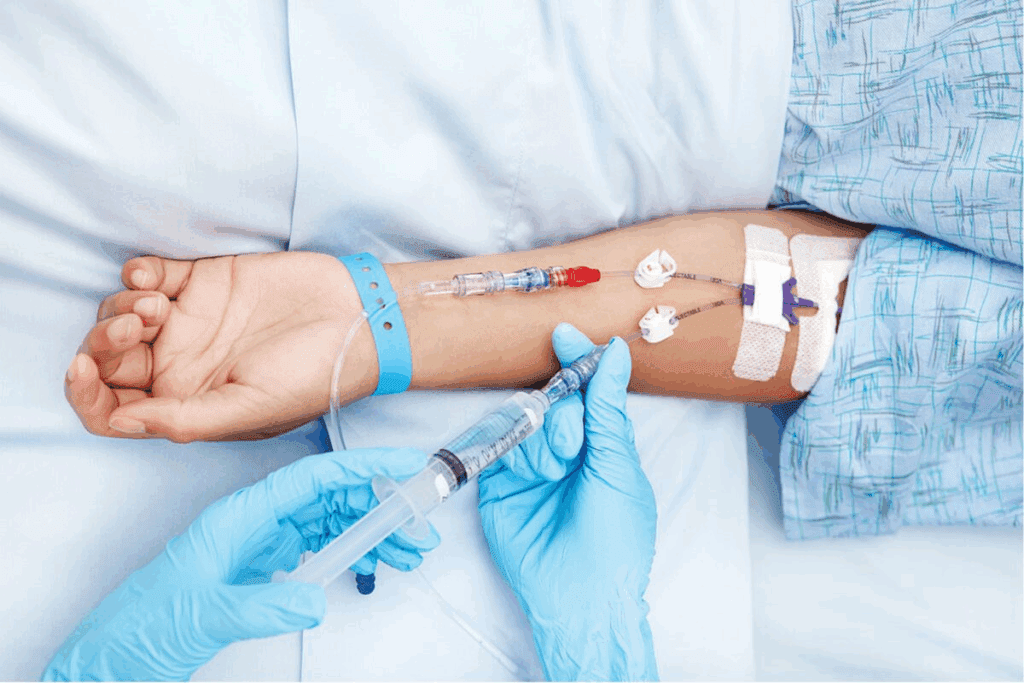
The Transplant Process and Preparation
The transplant starts with conditioning therapy. This uses chemotherapy and/or radiation to clear the sick bone marrow. Then, the patient gets healthy stem cells. These can come from a donor or the patient themselves.
Preparation steps include:
- Comprehensive pre-transplant evaluation
- Donor selection and matching (for allogeneic transplants)
- Conditioning regimen
- Stem cell harvesting and infusion
Outcomes and Survival Rates
MPN transplant outcomes depend on many things. These include the disease type, patient age, and health issues. Thanks to better transplant methods and care, survival rates have gone up.
| Disease Type | 1-Year Survival Rate | 5-Year Survival Rate |
| Primary Myelofibrosis | 70-80% | 40-50% |
| Polycythemia Vera | 80-90% | 50-60% |
| Essential Thrombocythemia | 85-95% | 60-70% |
These survival rates are just estimates. They can change based on the patient and their transplant details.
Managing Side Effects of MPN Treatments
Managing side effects is key in MPN treatment. It helps patients handle therapy and keep a good quality of life. MPN treatments include different therapies, each with its own side effects.
Chemotherapy-Related Side Effects
Chemotherapy is a common MPN treatment. It’s effective but can cause side effects. Common side effects include:
- Nausea and Vomiting: Medications can help manage these symptoms.
- Fatigue: Rest and gentle exercise can help alleviate fatigue.
- Hair Loss: Some chemotherapy agents can cause hair loss.
Patients should talk to their healthcare provider about their chemotherapy. This helps understand side effects and how to manage them.
JAK Inhibitor Side Effect Profile
JAK inhibitors are another treatment option for MPNs. They’re used for patients with certain genetic mutations. Common side effects include:
| Side Effect | Management Strategy |
| Anemia | Monitoring blood counts, transfusions if necessary |
| Infection Risk | Prophylactic antibiotics, monitoring for signs of infection |
Supportive Care During Treatment
Supportive care is vital in managing MPN treatment side effects. It includes:
- Nutritional Support: Ensuring adequate nutrition to help manage treatment side effects.
- Psychological Support: Counseling or therapy to cope with the emotional aspects of MPN treatment.
- Monitoring: Regular follow-up appointments to monitor for side effects and adjust treatment as necessary.
By adding supportive care to their treatment plan, patients with MPNs can manage side effects better. This improves their overall quality of life.
Complementary Approaches to MPN Management
Complementary therapies are great for helping with MPN treatments. They make patients feel better and manage symptoms better. Even though regular treatments are key, these extra methods can also help a lot.
Nutritional Support for MPN Patients
Eating right is very important for MPN patients. It helps keep them healthy and can make some symptoms better. Here are some tips:
- Hydration: Drinking enough water is very important, even more so when getting treatments.
- Antioxidant-rich foods: Eating foods like fruits and veggies can help fight off stress.
- Omega-3 fatty acids: These are in fish and flaxseeds and can help lower inflammation.
Talking to a nutritionist or doctor can help make a diet plan that’s just right for you.
Exercise and Physical Activity Benefits
Being active is good for MPN patients. It has many benefits:
| Exercise Type | Benefits |
| Aerobic Exercise | Improves heart health, cuts down on tiredness |
| Resistance Training | Makes muscles stronger, helps bones stay strong |
| Flexibility Exercises | Makes moving easier, cuts down on stiffness |
Always check with your doctor before starting any new workout plan. They can make sure it’s safe for you.
Mind-Body Interventions for Symptom Management
Mind-body methods are very helpful for MPN symptoms. They can make patients feel better and improve their mood. Some good options are:
- Meditation: Helps lower stress and anxiety.
- Cognitive-behavioral therapy (CBT) can help manage symptoms and mental health.
- Yoga: Mixes physical activity with mindfulness, which can reduce symptoms and improve life quality.
These methods should be used along with, not instead of, regular treatments.
Making Treatment Decisions with Your Healthcare Team
Getting the right treatment for MPN means working together with your healthcare team. This teamwork helps create a treatment plan that fits your unique needs.
Current Clinical Guidelines
It’s important to keep up with the latest treatment guidelines. These guidelines are based on new research and trials. They help doctors and patients manage MPN better.
Guidelines suggest treatments based on how high your risk is. Low-risk patients might just watch and wait. But high-risk patients might need stronger treatments like chemotherapy.
Questions to Ask About Chemotherapy vs. Alternatives
When looking at treatment options, talk to your team about the pros and cons of each. Ask questions like:
- What are the side effects of chemotherapy, and how can they be managed?
- Are there other treatments that could work just as well but have fewer side effects?
- How will this treatment affect my daily life?
- Are there new trials or therapies that could help me?
Shared Decision-Making Process
At the core of managing MPN is shared decision-making. This means talking together to choose the best treatment. It involves patients, their families, and healthcare teams.
Key parts of shared decision-making are:
- Talking openly about the diagnosis, treatment choices, and what to expect.
- Thinking about what matters most to the patient, like their lifestyle and values.
- Looking at the good and bad sides of each treatment option.
- Checking in regularly to see if the treatment plan needs to change.
This way, patients can make choices that fit their personal goals and life. This leads to better treatment results.
Myeloproliferative Neoplasms: Long-Term Outlook
Survival rates for MPN patients depend on several factors. These include the type of MPN and how well the treatment works. Knowing these factors helps both patients and doctors make better treatment choices.
Survival Rates by MPN Type and Treatment
Survival rates for MPN patients differ based on the type of MPN. Essential Thrombocythemia (ET) usually has a better outlook than Primary Myelofibrosis (PMF).
| MPN Type | 5-Year Survival Rate | 10-Year Survival Rate |
| Essential Thrombocythemia (ET) | 85-95% | 70-85% |
| Polycythemia Vera (PV) | 80-90% | 65-80% |
| Primary Myelofibrosis (PMF) | 50-70% | 30-50% |
The table shows how survival rates vary among MPN types. Treatment options, like chemotherapy and targeted therapy, greatly impact these rates.
Factors Affecting Prognosis
Several factors can change an MPN patient’s prognosis. These include genetic mutations and the patient’s age and health at diagnosis.
- Genetic Mutations: The type and number of genetic mutations can significantly affect prognosis.
- Age and Health Status: Older patients or those with comorbid conditions may face a poorer prognosis.
- Disease Characteristics: The specific characteristics of the MPN, such as the presence of fibrosis in PMF, can influence outcomes.
Disease Progression and Transformation Risks
MPN patients are at risk of their disease getting worse or turning into more aggressive forms, like acute myeloid leukemia (AML). The risk of transformation varies by MPN subtype. It’s a key factor in long-term management.
Regular monitoring and adjusting treatment plans are vital. They help manage these risks and improve patient outcomes.
Conclusion: Navigating Your MPN Treatment Journey
Dealing with Myeloproliferative Neoplasm (MPN) treatment needs smart choices and help from doctors. Knowing your treatment options, like chemotherapy, is key to controlling the disease.
In this guide, we’ve looked at the different MPNs, their signs, and treatment methods. From old-school chemotherapy to new JAK inhibitors, managing MPN is complex. Understanding the disease well is vital for good management.
When you’re on your MPN treatment path, team up with your doctors to find the right treatment for you. Being informed and active in your care helps you make better choices. This way, you can live better with MPN.
FAQ
What are myeloproliferative neoplasms (MPNs)?
Myeloproliferative neoplasms (MPNs) are rare blood cancers. They cause the bone marrow to make too many blood cells. Types include essential thrombocythemia (ET), polycythemia vera (PV), and primary myelofibrosis.
What is the role of chemotherapy in MPN treatment?
Chemotherapy helps in MPN treatment. It lowers the risk of blood clots, manages symptoms, and controls blood cell growth. It’s used for high-risk patients or those with disease progression.
What are the common symptoms of MPNs?
Symptoms of MPNs include fatigue, weight loss, night sweats, itching, and a big spleen. Symptoms vary by MPN type and patient.
How are MPNs diagnosed?
Doctors use blood tests, bone marrow biopsies, and genetic tests to diagnose MPNs. They look for JAK2, CALR, or MPL mutations. They also check blood cell counts and bone marrow findings.
What is the significance of the JAK2 mutation in MPNs?
The JAK2 mutation is common in MPNs, like PV. It’s key in disease development and treatment choices.
Are there alternative treatments to chemotherapy for MPNs?
Yes, there are alternatives to chemotherapy. For PV, phlebotomy is used. Low-dose aspirin prevents blood clots. JAK inhibitors help in primary myelofibrosis. Treatment choice depends on MPN type, risk, and patient factors.
What is the watch-and-wait approach in MPN management?
The watch-and-wait approach is for low-risk MPN patients. It involves regular checks without immediate treatment. It’s based on weighing treatment risks against benefits.
Can MPNs be cured?
Stem cell transplantation is the only cure for MPNs. But, it’s for eligible patients with advanced disease or high-risk features due to risks.
How do MPN treatments manage side effects?
Managing side effects is key in MPN treatment. Supportive care, like medications and lifestyle changes, helps. This includes nutritional support and adjusting to treatments like chemotherapy and JAK inhibitors.
What is the long-term outlook for patients with MPNs?
The outlook for MPN patients varies. It depends on MPN type, risk factors, and treatment response. Survival has improved with new treatments like targeted therapies and stem cell transplantation.
What are the risks of disease progression in MPNs?
MPNs can progress to more aggressive forms like myelofibrosis or acute myeloid leukemia. Regular monitoring and timely action are vital to manage these risks.
How do complementary approaches help in MPN management?
Complementary approaches, like nutrition, exercise, and mind-body interventions, help manage symptoms. They improve the quality of life and can make conventional treatments more effective for MPN patients.
References
- Lee, S. S., Tefferi, A., & Verstovsek, S. (2021). Novel therapies in myeloproliferative neoplasms. Hematology/Oncology Clinics of North America, 35(3), 121-134. https://pmc.ncbi.nlm.nih.gov/articles/PMC9138435/



































