Did you know that brain disorders affect over 43 million people worldwide? A big part of them have brain tumors.neurology vs neuro-oncologyTumor Brain CT Scan: Detection vs MRI
Neurology and neuro-oncology are two medical fields that often work together. But they have different main areas. Neurology is about treating brain, spine, and nervous system problems.
Neuro-oncology is a special area. It deals with brain and spinal cord tumors, their diagnosis, treatment, and management.
Understanding the distinction between neurology and neuro-oncology is crucial for ensuring patients receive the appropriate diagnosis and treatment. This helps patients get the right diagnosis and treatment.
Key Takeaways
- Neurology covers a wide range of neurological disorders.
- Neuro-oncology is a specialized field focusing on brain and spinal cord tumors.
- The distinction between the two fields is vital for accurate diagnosis and treatment.
- Both fields require a deep understanding of the nervous system.
- Collaboration between neurologists and neuro-oncologists is often necessary for complex cases.
The Nervous System: Foundation of Neurological Specialties

Understanding the distinction between neurology and neuro-oncology is crucial for ensuring patients receive the appropriate diagnosis and treatment.
The nervous system has two main parts: the Central Nervous System (CNS) and the Peripheral Nervous System (PNS). The CNS includes the brain and spinal cord, acting as the body’s control center. The PNS has nerves that connect the CNS to the rest of the body.
Central and Peripheral Nervous System Structure
The CNS is protected by the blood-brain barrier. This barrier controls what substances can enter the brain. The PNS has two parts: the somatic nervous system for voluntary actions and the autonomic nervous system for involuntary actions.
Brain and Spinal Cord Functions
The brain is the body’s control center. It processes sensory information, controls movement, and manages functions like emotion and memory. The spinal cord extends the brain and is key for reflex actions and communication between the brain and body.
| Component | Function | Associated Conditions |
| Central Nervous System (CNS) | Control center, processing sensory information | Multiple Sclerosis, CNS disorders |
| Peripheral Nervous System (PNS) | Communication between CNS and body | Peripheral Neuropathy, nerve damage |
| Brain | Control center, emotion, memory, cognition | Alzheimer’s, Parkinson’s, Brain Tumors |
| Spinal Cord | Reflex actions, message conveyance | Spinal Cord Injuries, Spinal Tumors |
The nervous system’s complexity and role in the body’s functions highlight its importance. Neurological conditions often stem from disruptions or diseases affecting this system.
Defining Neurology: Scope and Practice

Neurology is a medical field that studies the nervous system. This system includes the brain, spinal cord, and nerves. It controls how we move, feel, and think.
Neurology is key in healthcare. It deals with many disorders of the nervous system. These can be short-term or long-lasting, needing detailed diagnosis and treatment.
The Role of Neurologists in Healthcare
Neurologists are doctors who specialize in nervous system disorders. They do neurological examinations to check how well the brain and nerves work. Then, they create a neurological treatment plan for each patient.
Neurologists are important for treating conditions like epilepsy, stroke, and multiple sclerosis. They work with other doctors to give the best care possible, helping patients get better.
Common Neurological Disorders and Conditions
Neurologists see many conditions, from common ones like migraines to rare diseases like Parkinson’s and Alzheimer’s.
| Condition | Description | Typical Treatment Approach |
| Epilepsy | A neurological disorder characterized by recurrent seizures. | Anticonvulsant medications, potentially surgery. |
| Stroke | A condition where the blood supply to part of the brain is interrupted or reduced. | Emergency medical treatment, rehabilitation therapies. |
| Multiple Sclerosis | A chronic disease affecting the central nervous system. | Disease-modifying therapies, symptomatic treatments. |
The table shows some common neurological conditions and how they are treated. Neurologists are key in finding these conditions and creating neurology treatment plans.
In summary, neurology is a vital medical field. It helps patients with neurological disorders through detailed care and treatments. Neurologists greatly improve the lives of their patients.
Defining Neuro-Oncology: Focus and Specialization
Neuro-oncology is a special field of medicine. It deals with tumors in the brain and nervous system. It needs a deep understanding of the nervous system and cancer.
More people are getting brain and nervous system tumors. Neuro-oncologists are the experts. They use surgery, radiation, and new treatments like immunotherapy.
The Role of Neuro-Oncologists in Cancer Care
Neuro-oncologists are key in treating brain and nervous system cancers. They:
- Use advanced imaging to diagnose tumors
- Make treatment plans that might include surgery or chemotherapy
- Help manage symptoms to improve quality of life
- Work with other specialists for a complete care plan
Types of Brain and Nervous System Tumors
Brain and nervous system tumors can be benign or malignant. They vary in how they affect patients. Here are some common types:
- Gliomas: Tumors from brain cells, from low-grade to high-grade (glioblastoma)
- Meningiomas: Usually benign tumors in the brain’s membranes
- Medulloblastomas: Malignant brain tumors mostly in children
- Nerve sheath tumors: Tumors from nerve sheaths, like schwannomas and neurofibromas
Knowing the tumor type is key for the right treatment. Neuro-oncologists work with others to give care that fits each patient’s needs.
Neurology vs Neuro-Oncology: Key Differences Explained
Understanding the distinction between neurology and neuro-oncology is crucial for ensuring patients receive the appropriate diagnosis and treatment. Both deal with the nervous system but in different ways. Their focuses, practices, and how they care for patients are quite different.
Scope of Practice Comparison
Neurology deals with many nervous system disorders. This includes the brain, spinal cord, and nerves. Neurologists treat conditions like migraines, epilepsy, stroke, and diseases like Alzheimer’s and Parkinson’s.
Neuro-oncology, on the other hand, focuses on brain and spinal tumors. Neuro-oncologists work with neurosurgeons and radiation oncologists. They aim to give complete care to patients with these tumors.
Patient Population Differences
Neurology and neuro-oncology see different types of patients. Neurologists care for those with chronic conditions needing ongoing care. Neuro-oncologists mainly treat patients with brain or nervous system tumors, often with other oncology specialists.
Key differences in patient populations include:
- Neurology patients often have chronic conditions requiring ongoing care.
- Neuro-oncology patients typically have cancerous or benign tumors affecting the nervous system.
- Neuro-oncology care is often more acute, focusing on tumor treatment and management.
Treatment Approach Variations
Neurology and neuro-oncology use different treatments. Neurologists use medications, lifestyle changes, and neurorehabilitation. Neuro-oncologists use treatments like surgery, radiation, chemotherapy, and targeted therapies for tumors.
Collaborative care is a hallmark of both fields. Specialists work together for patient care. For example, neurologists and neuro-oncologists team up to manage symptoms in cancer patients.
Collaborative Care Models
Both neurologists and neuro-oncologists work in teams. Neurologists might team up with rehabilitation specialists and psychologists. Neuro-oncologists collaborate with neurosurgeons and oncologists for tumor treatment plans.
Examples of collaborative care models include:
- Tumor boards, where specialists discuss patient cases and develop treatment plans.
- Multidisciplinary clinics, providing complete care under one roof.
- Coordinated care pathways, ensuring smooth transitions between treatment phases.
Educational Pathways: Becoming a Neurologist
To become a neurologist, one must go through a lot of education and training. This starts with a strong foundation in medical school.
Medical School and Residency Requirements
The journey to becoming a neurologist starts with medical school. This is a four-year program after getting a bachelor’s degree. In medical school, students learn about many medical specialties, including neurology.
After medical school, aspiring neurologists need to do a residency in neurology. This can last from three to four years. It’s important for getting the needed experience in diagnosing and treating neurological disorders.
Residency programs in neurology are accredited by the Accreditation Council for Graduate Medical Education (ACGME). They offer training in diagnosing and managing neurological conditions like stroke and epilepsy.
Board Certification Process
After residency, neurologists must get board certification from the American Board of Psychiatry and Neurology (ABPN). They pass a tough exam that tests their knowledge and skills. Board certification shows their expertise to patients and peers.
To keep their certification, neurologists must do continuing medical education (CME) courses. They also follow the ABPN’s Maintenance of Certification program. This keeps them up-to-date with the latest in neurology.
Subspecialty Options in Neurology
Neurology has many subspecialties, like pediatric neurology and neuromuscular medicine. Neurologists can get more training through fellowship programs. This lets them focus on specific areas and provide specialized care.
Subspecializing lets neurologists focus on what they’re interested in. For example, a pediatric neurologist works with children. They diagnose and treat conditions specific to kids.
Understanding how to become a neurologist shows the hard work and dedication needed. It highlights the importance of neurologists in healthcare. They play a key role in diagnosing and managing complex conditions and advancing neurology.
Educational Pathways: Becoming a Neuro-Oncologist
Neuro-oncology is a specialized field that needs a deep understanding of neurological disorders and cancer treatment. It requires advanced education.
To become a neuro-oncologist, you need to follow a multi-step process. This includes extensive medical education, specialized training, and keeping up with the latest field advancements.
Additional Training Beyond Neurology or Oncology
First, you must complete medical school. Then, you need to get specialized training in either neurology or oncology. Additional training beyond general neurology or oncology is key for managing complex brain and nervous system tumors.
This extra training focuses on the latest research and treatment methods in neuro-oncology. It includes advanced surgical techniques, radiation therapy, and chemotherapy protocols.
Fellowship Requirements
Fellowship programs in neuro-oncology offer the specialized training needed for managing brain tumors and central nervous system cancers. These programs last one to two years. They provide hands-on experience in multidisciplinary care teams.
During their fellowship, aspiring neuro-oncologists work with experienced specialists. They develop skills in diagnosing and treating complex cases. They also conduct neuro-oncology research.
Multidisciplinary Expertise Development
Neuro-oncologists need to develop a wide range of skills. They must interpret complex imaging studies, perform neurological examinations, and apply the latest neuro-oncology treatment protocols.
Developing multidisciplinary expertise is helped by working with other specialists. This includes neurosurgeons, radiation oncologists, and rehabilitation specialists. Teamwork is key for providing complete care to patients with brain tumors.
| Training Component | Description | Duration |
| Medical School | Foundational education in medicine | 4 years |
| Residency in Neurology or Oncology | Specialized training in neurology or oncology | 4-5 years |
| Fellowship in Neuro-Oncology | Advanced training in neuro-oncology | 1-2 years |
By following these educational paths, future brain tumor specialists are ready to provide top-notch care. They also contribute to neuro-oncology research, helping to advance the field and improve patient outcomes.
Diagnostic Methods in Neurology
Diagnosing neurological disorders is complex. It involves many techniques, from physical exams to advanced imaging and lab tests. Getting the diagnosis right is key for good treatment and managing conditions.
Comprehensive Neurological Examinations
A thorough neurological exam is the first step. It includes a detailed medical history and physical check-up. Neurologists use special tools to check how well the brain and nerves are working.
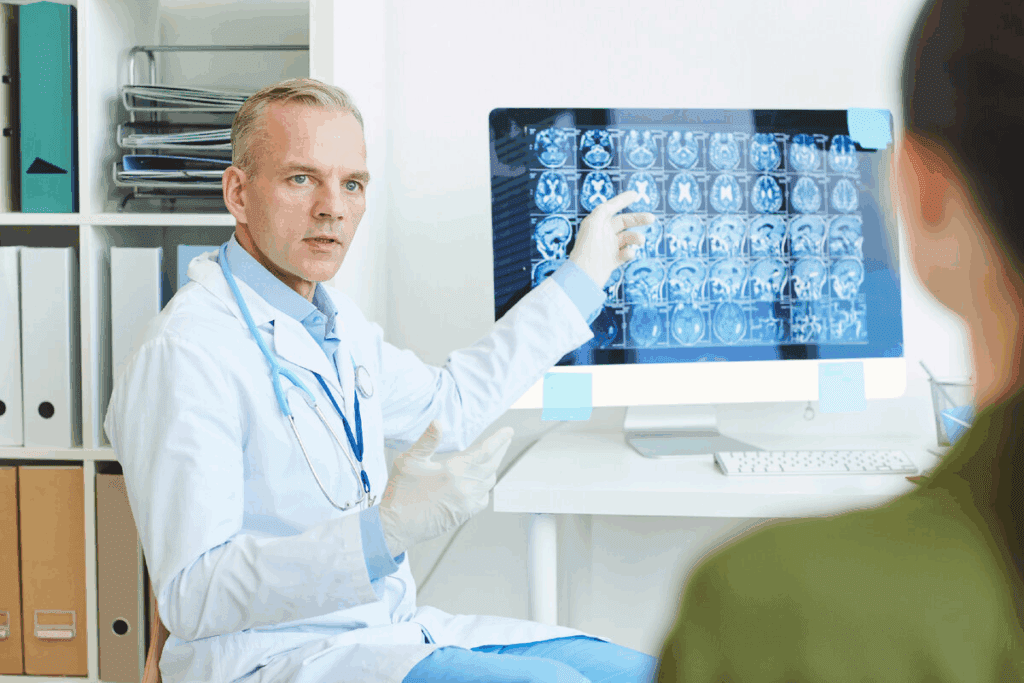
Neuroimaging Techniques
Neuroimaging is vital in neurology. It lets doctors see the brain and spinal cord clearly. MRI, CT scans, and PET scans give important details about the brain’s structure and function. “Neuroimaging has changed neurology, making diagnoses earlier and more accurate,” says a top neurologist.
Electrophysiological Testing
Electrophysiological tests, like EEG and EMG, check the brain and muscle’s electrical activity. These tests are key for diagnosing epilepsy, nerve damage, and muscle issues. They show how well the nervous system is working.
Laboratory Assessments
Laboratory tests analyze blood and other fluids to find signs of neurological diseases. These tests help diagnose conditions like multiple sclerosis and infections. Advanced tests, like genetic testing, are also used in neurology.
In summary, neurology uses many diagnostic methods. Each method gives different insights into the nervous system. By combining these, neurologists can make accurate diagnoses and plan effective treatments.
Diagnostic Methods in Neuro-Oncology
Neuro-oncology uses advanced methods to identify and manage brain tumors. These methods are needed because brain tumors are complex. They require a detailed approach that uses different techniques.
Advanced Tumor Imaging Techniques
Advanced imaging is key in diagnosing and managing brain tumors. Tools like MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans give detailed images. This helps doctors plan treatments.
Functional MRI and MR spectroscopy give more information about the tumor. They show how the tumor affects the brain.
These advanced images help doctors find and understand tumors. They are important for making treatment plans. Diffusion-weighted imaging and perfusion-weighted imaging help see how aggressive the tumor is and how well it’s responding to treatment.
Biopsy Procedures and Tissue Analysis
Biopsy procedures are vital for getting tissue samples. These samples are analyzed to find out the tumor type and grade. This information is key for deciding treatment.
Stereotactic biopsy and open biopsy are used, depending on the tumor’s location and type.
Tissue analysis looks at the tumor’s cells and molecules. It checks histological features, immunohistochemical markers, and other molecular details. This helps classify and predict the tumor’s behavior.
Molecular and Genetic Profiling
Molecular and genetic profiling is vital in neuro-oncology. Next-generation sequencing (NGS) finds genetic mutations that guide treatment. IDH mutations and MGMT promoter methylation are important markers.
This profiling helps tailor treatments and find the right clinical trials. It makes treatment more personal and effective.
Biomarker Testing
Biomarker testing is essential in neuro-oncology. Biomarkers tell us about tumor behavior, treatment response, and prognosis. Liquid biopsies are a non-invasive way to monitor tumor genetics and detect resistance.
Biomarkers help tailor treatments, improving outcomes and reducing harm. Research is ongoing to find and validate new biomarkers for brain tumor management.
Treatment Approaches in Neurology
Neurology uses many treatments for complex conditions. These conditions often need a mix of treatments to manage symptoms and improve life quality.
Medication Management Strategies
Medicine is key in treating neurological conditions. Anticonvulsants help control seizures. Disease-modifying therapies slow conditions like multiple sclerosis. Symptomatic treatments manage pain.
Neurorehabilitation Therapies
Neurorehabilitation helps patients regain lost functions. It includes physical therapy for mobility, occupational therapy for daily tasks, and speech therapy for communication.
Interventional Procedures
Interventional procedures are sometimes needed. They include botulinum toxin injections for spasticity, deep brain stimulation for movement disorders, and spinal cord stimulation for pain.
Chronic Disease Management
Managing chronic neurological diseases needs a full plan. This includes regular checks, lifestyle changes, and patient education. It helps control the disease and improves life quality.
Neurologists use these treatments together to care for patients with neurological disorders.
Treatment Approaches in Neuro-Oncology
Managing brain tumors needs a mix of treatments. Each approach is chosen based on the tumor’s type, size, and where it is. The patient’s health and what they prefer also play a big role.
Surgical Resection Techniques
Surgery is key for many brain tumors. New techniques have made surgery safer and more precise. Awake craniotomy and intraoperative MRI help doctors remove tumors carefully.
Radiation Therapy Modalities
Radiation therapy is vital for some tumors. It’s used when surgery isn’t possible or when there’s leftover tumor. Stereotactic radiosurgery (SRS), fractionated stereotactic radiotherapy (FSRT), and intensity-modulated radiation therapy (IMRT) target tumors well without harming healthy brain.
| Radiation Modality | Description | Typical Use |
| SRS | Delivers a high dose of radiation in a single fraction | Small, well-defined tumors |
| FSRT | Delivers radiation in multiple fractions | Tumors near critical structures |
| IMRT | Modulates beam intensity to conform to tumor shape | Complex or irregularly shaped tumors |
Chemotherapy and Targeted Treatments
Chemotherapy is key for some brain tumors. Temozolomide is often used for glioblastoma. Bevacizumab targets specific tumor growth and blood vessel formation.
Emerging Immunotherapies and Clinical Trials
Immunotherapy is a new hope in neuro-oncology. It includes vaccine-based therapies, checkpoint inhibitors, and CAR T-cell therapy. These early treatments might lead to better outcomes for tough brain tumors.
Patient Experiences: Case Scenarios and Care Journeys
The journey of patients with neurological disorders or brain tumors is complex and multifaceted. Understanding these experiences is key to providing top-notch care.
Neurological Disorder Management Cases
Managing neurological disorders needs a full approach. For example, a patient with Parkinson’s might get treatments like medication, physical therapy, and lifestyle changes.
Case Scenario: A 65-year-old male with Parkinson’s saw big improvements in his motor skills. This was thanks to a special physical therapy program and changes in his meds.
- Initial diagnosis and treatment planning
- Ongoing monitoring and adjustment of treatment
- Multidisciplinary care involving neurologists, therapists, and caregivers
Brain Tumor Treatment Journeys
Patients with brain tumors face big challenges, from diagnosis to treatment and recovery. Their care often includes surgery, radiation, and chemotherapy.
Case Example: A 45-year-old female with glioblastoma had surgery, then radiation and chemo. Her treatment was tweaked based on MRI scans and doctor checks.
| Treatment Phase | Interventions | Goals |
| Surgery | Surgical resection | Remove tumor |
| Adjuvant Therapy | Radiation, Chemotherapy | Kill remaining cancer cells |
| Follow-up | Regular scans, Clinical assessments | Monitor for recurrence |
Quality of Life Considerations
Keeping quality of life high is vital for patients with neurological disorders or brain tumors. This means managing symptoms, addressing mental health, and supporting patients and their families.
Quality of Life Strategies:
- Symptom management through medication and therapy
- Psychological support through counseling and support groups
- Lifestyle adjustments to maintain independence and functionality
By focusing on patient experiences and care journeys, healthcare providers can offer more caring and effective care. This improves outcomes for patients with neurological conditions.
Technological Advancements Shaping Both Fields
Technological advancements are changing neurology and neuro-oncology. They bring new hope for patients and doctors. New technologies improve diagnosis, treatment, and make work easier.
Innovative Diagnostic Technologies
New diagnostic tools have made finding and tracking brain issues better. Some key innovations include:
- Advanced neuroimaging techniques, such as functional MRI and diffusion tensor imaging
- High-resolution ultrasound and optoacoustic imaging
- Liquid biopsy and circulating tumor DNA analysis
These tools help doctors find problems sooner and more accurately. This means they can start treatments faster.
Treatment Delivery Breakthroughs
Treatment methods have also improved a lot. Some new technologies are:
- Precision radiation therapy and stereotactic radiosurgery
- Laser-induced thermal therapy for tumor ablation
- Immunotherapy and targeted therapies tailored to individual patient profiles
These advances make treatments work better and have fewer side effects. This leads to better results for patients.
Artificial Intelligence Applications
Artificial intelligence (AI) is being used more in neurology and neuro-oncology. AI helps with diagnosis, planning treatments, and caring for patients. AI can:
- Analyze large datasets to identify patterns and predict patient outcomes
- Assist in image analysis and tumor segmentation
- Optimize treatment plans based on individual patient characteristics
A study in a top medical journal showed AI’s role in glioblastoma treatment. It shows AI’s power in making medicine more personal.
“The integration of AI in neuro-oncology is poised to revolutionize treatment strategies, enabling more precise and effective care.”
Here’s a look at how AI changes diagnosis compared to old methods:
| Diagnostic Approach | Traditional Methods | AI-Enhanced Methods |
| Image Analysis | Manual interpretation by radiologists | AI algorithms for pattern recognition and anomaly detection |
| Data Analysis | Limited by human capacity to process large datasets | AI-driven analysis for insights and predictions |
| Treatment Planning | Based on clinical guidelines and experience | AI-optimized plans tailored to individual patient profiles |
The future of neurology and neuro-oncology is bright. It’s all about using new technologies to improve care and results.
Career Outlook and Opportunities
The fields of neurology and neuro-oncology are growing fast. This growth is due to new medical technology and an aging population. As a result, there’s a big need for skilled professionals in these areas.
Job Market for Neurologists
The job market for neurologists is strong. This is because more people are getting older and more neurological disorders are happening. Neurologists have many job options, from working in private practice to teaching and researching.
Demand for Neuro-Oncologists
Neuro-oncology is a specialized field that’s in high demand. Experts in this area help diagnose and treat brain and nervous system tumors. Neuro-oncologists are key in healthcare teams because they bring a unique skill set to the table.
Research and Academic Pathways
If you’re into research and teaching, neurology and neuro-oncology are great choices. You can help with important research and teach the next generation of doctors.
Private Practice vs. Hospital-Based Careers
Neurologists and neuro-oncologists can work in private practice or hospitals. Private practice offers freedom and flexibility. Hospital jobs, on the other hand, give you teamwork and access to the latest technology.
In summary, the future looks bright for neurologists and neuro-oncologists. They have many chances to help patients and advance medical science.
Conclusion: The Complementary Relationship Between Neurology and Neuro-Oncology
Neurology and neuro-oncology are two important medical fields. They work together to help patients with brain issues and tumors. This teamwork is key to better care and research.
Neurologists and neuro-oncologists team up to tackle tough cases. They use their skills to make treatment plans that work. This partnership is vital for improving patient care and life quality.
As technology gets better, the bond between neurology and neuro-oncology will grow stronger. Healthcare pros can tackle complex patient needs better by knowing how these fields fit together.
FAQ
What is the primary difference between neurology and neuro-oncology?
Neurology deals with the nervous system’s disorders. Neuro-oncology focuses on brain and nervous system tumors.
What is the role of a neurologist in patient care?
Neurologists treat many neurological disorders. They use medicines and rehabilitation to help patients.
What kind of training is required to become a neuro-oncologist?
To be a neuro-oncologist, one needs extra training. This includes fellowship programs for brain and nervous system tumors.
How do diagnostic methods differ between neurology and neuro-oncology?
Both use neuroimaging. But neuro-oncology uses advanced imaging and biopsies for tumor diagnosis.
What are the treatment approaches used in neurology?
Neurology uses medicines, rehabilitation, and procedures. Treatments are tailored for each disorder.
What treatment modalities are used in neuro-oncology?
Neuro-oncology uses surgery, radiation, and chemotherapy. It also includes new treatments like immunotherapy.
How do neurologists and neuro-oncologists collaborate in patient care?
They work together in teams. This ensures both the tumor and symptoms are managed well.
What is the significance of quality of life considerations in neurology and neuro-oncology?
Quality of life is key in both fields. Treatments aim to manage disease and keep patients well.
How are technological advancements impacting neurology and neuro-oncology?
New technologies improve diagnosis and treatment. They include advanced imaging and artificial intelligence.
What are the career prospects for neurologists and neuro-oncologists?
Both have good career prospects. They can work in research, academia, or private practice.
What is the relationship between neurology and neuro-oncology in patient care and research?
Neurology and neuro-oncology work together. Neurology lays the groundwork, and neuro-oncology focuses on tumors.
References
National Institutes of Health. Evidence-Based Medical Insight. Retrieved from
https://www.ninds.nih.gov/health-information/public-education/brain-basics/know-your-brain