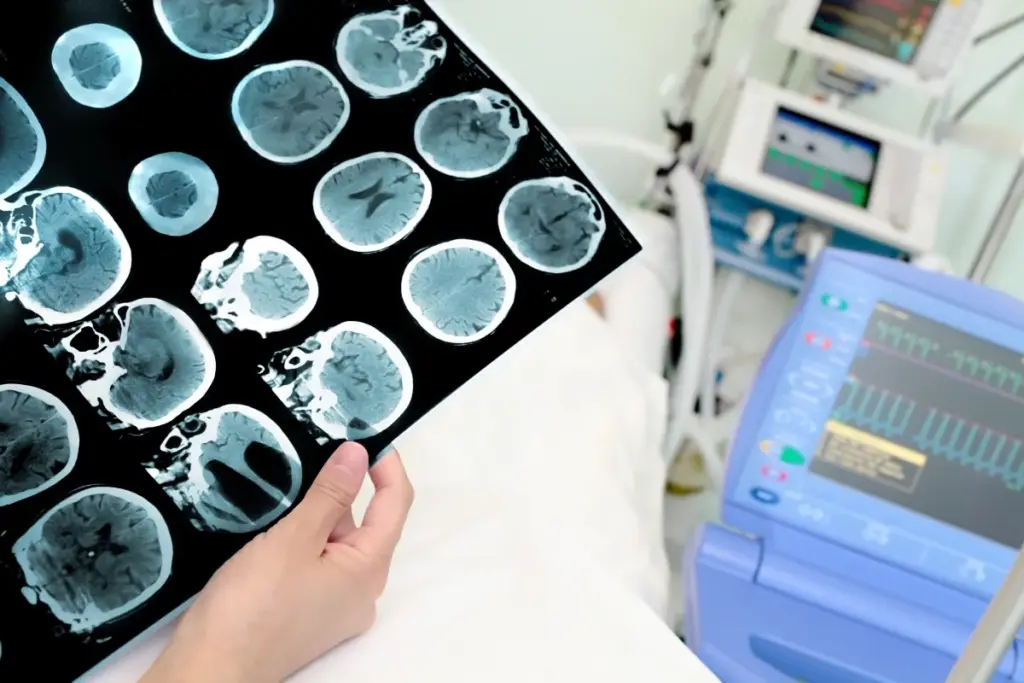
Neurology diagnoses and treats disorders of the nervous system, including the brain, spinal cord, and nerves, as well as thought and memory.
Send us all your questions or requests, and our expert team will assist you.

Vascular neurology is the specialized branch of medicine dedicated to the health, pathology, and treatment of the blood vessels supplying the nervous system. While commonly synonymous with stroke care, the field encompasses a much broader spectrum of disorders, including aneurysms, vascular malformations, vasculitis, and spinal cord vascular diseases. It operates at the intersection of hydrodynamics, hematology, and neuroanatomy, studying how the disruption of blood flow—whether by blockage or rupture—alters brain function.
The brain is metabolically voracious. Despite accounting for only 2% of body weight, it consumes 20% of the body’s oxygen and 25% of its glucose. Unlike muscle or liver tissue, the brain has almost no energy reserves. It relies on a continuous, uninterrupted perfusion of blood to maintain the ionic gradients essential for neuronal firing. Vascular neurology is fundamentally the study of this supply-demand relationship and the catastrophic consequences when it fails.
To practice vascular neurology, one must have a three-dimensional understanding of the cerebral vasculature. The brain is fed by two distinct systems: the anterior circulation (carotid arteries) supplying the frontal, parietal, and temporal lobes, and the posterior circulation (vertebral-basilar arteries) supplying the brainstem, cerebellum, and occipital lobes. These systems anastomose (connect) at the base of the brain to form the Circle of Willis.
The Circle of Willis is the brain’s primary insurance policy. If one major artery becomes occluded slowly over time, blood can shunt across the circle to keep the tissue alive. Vascular neurologists assess the integrity of these “collateral” pathways. Good collaterals can sustain a patient for hours during a stroke, expanding the treatment window, while poor collaterals lead to rapid, irreversible tissue death.
Modern vascular neurology has moved beyond viewing the blood vessel as a simple pipe. The focus is now on the “Neurovascular Unit” (NVU). This conceptual unit consists of the endothelial cell (lining the vessel), the pericyte (contractile cell wrapping the vessel), the astrocyte foot process, and the neuron itself. These components communicate chemically to regulate blood flow in real-time.
When neurons fire, they release signals (neurovascular coupling) that tell the local blood vessels to dilate, bringing more fuel to that specific active area. In diseases like chronic hypertension or Alzheimer’s, this coupling breaks down. The study of NVU dysfunction is central to understanding small vessel disease and vascular cognitive impairment.

Ischemia occurs when blood flow drops below a critical threshold. The biochemistry of ischemia is a rapid, destructive cascade. Within seconds of oxygen deprivation, oxidative phosphorylation in the mitochondria ceases. The neuron switches to anaerobic glycolysis, producing lactic acid. This fails to produce enough ATP to run the sodium-potassium pumps.
As the ion pumps fail, the neuron depolarizes, causing a massive release of glutamate. This excitatory neurotransmitter floods the synaptic cleft, overstimulating receptors on neighboring cells and causing a lethal influx of calcium. This “excitotoxicity” digests the cell from the inside out. Vascular neurology aims to intervene before this “ischemic core” expands into the salvageable “penumbra.”
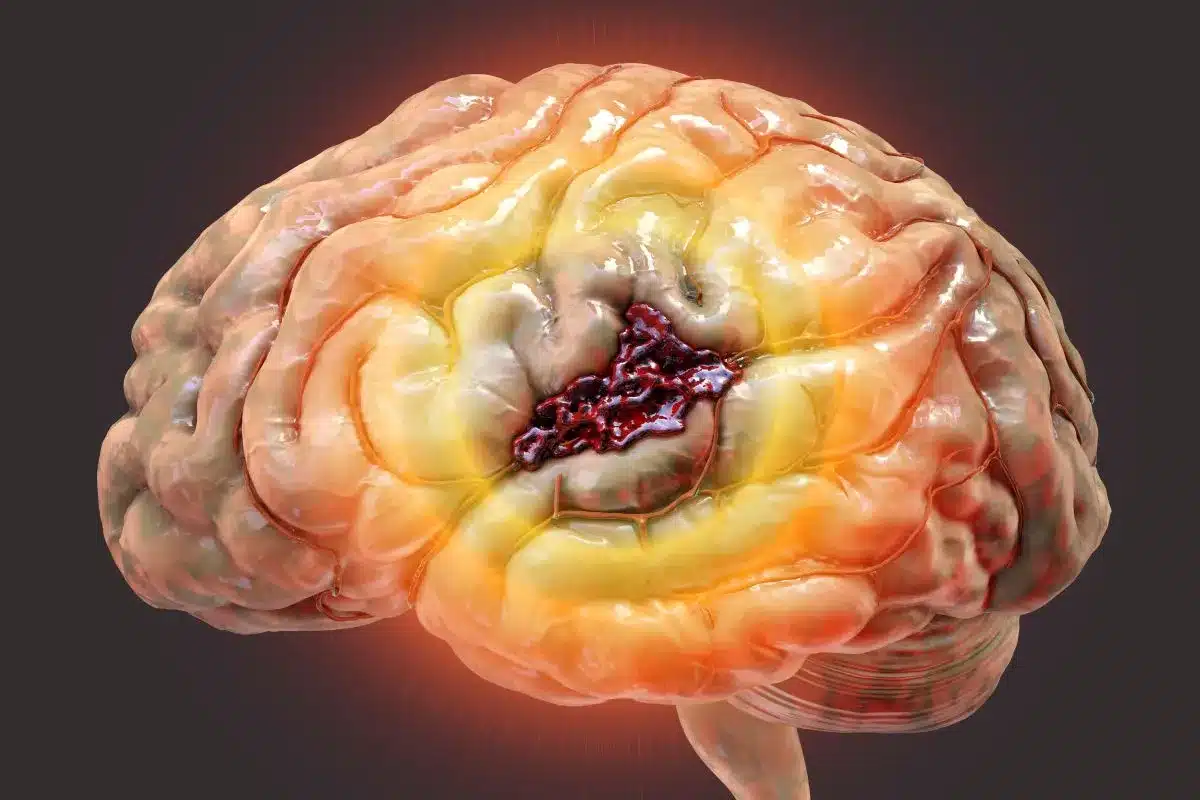
Hemorrhagic stroke involves the rupture of a vessel, leaking blood directly into the brain parenchyma (intracerebral) or the surrounding fluid spaces (subarachnoid). The pathology here is twofold: direct mechanical destruction and chemical toxicity. The high-pressure jet of blood tears through white matter tracts, creating a hematoma that acts as a rapidly expanding mass.
Secondary injury arises from the blood breakdown products. Hemoglobin releases iron, which is potent neurotoxin causing inflammation and edema (swelling). In subarachnoid hemorrhage, the blood bathing the outside of the vessels can irritate them, causing them to constrict days later. This phenomenon, known as vasospasm, causes delayed ischemic strokes and is a major focus of neurocritical care.

Send us all your questions or requests, and our expert team will assist you.
A stroke is an event where blood flow is blocked or a vessel bursts causing brain damage, whereas an aneurysm is a balloon-like weakness in a vessel wall that might burst and cause a hemorrhagic stroke.
Collaterals are backup blood vessels, like natural bypasses, that can open up to supply blood to a brain area if the main artery gets blocked, essentially buying time for the patient.
No, vascular dementia is caused by reduced blood flow or multiple small strokes damaging the brain’s white matter, whereas Alzheimer’s is primarily caused by the accumulation of toxic proteins (amyloid and tau).
It is the team of cells (blood vessel cells, support cells, and neurons) that work together to ensure the brain gets exactly the right amount of blood at the right time.
Yes, while rare, young people can suffer from vascular issues like arterial dissections (tears in the vessel wall), vasculitis, or genetic clotting disorders that lead to stroke.


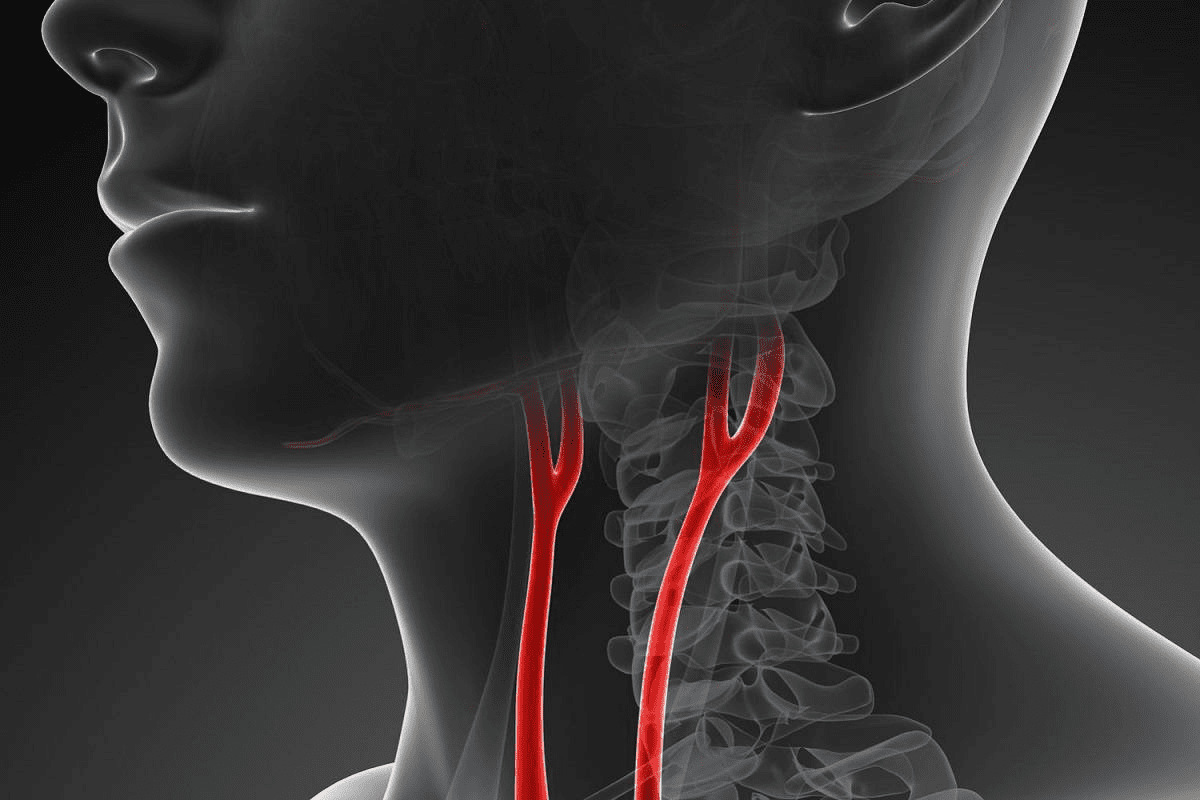
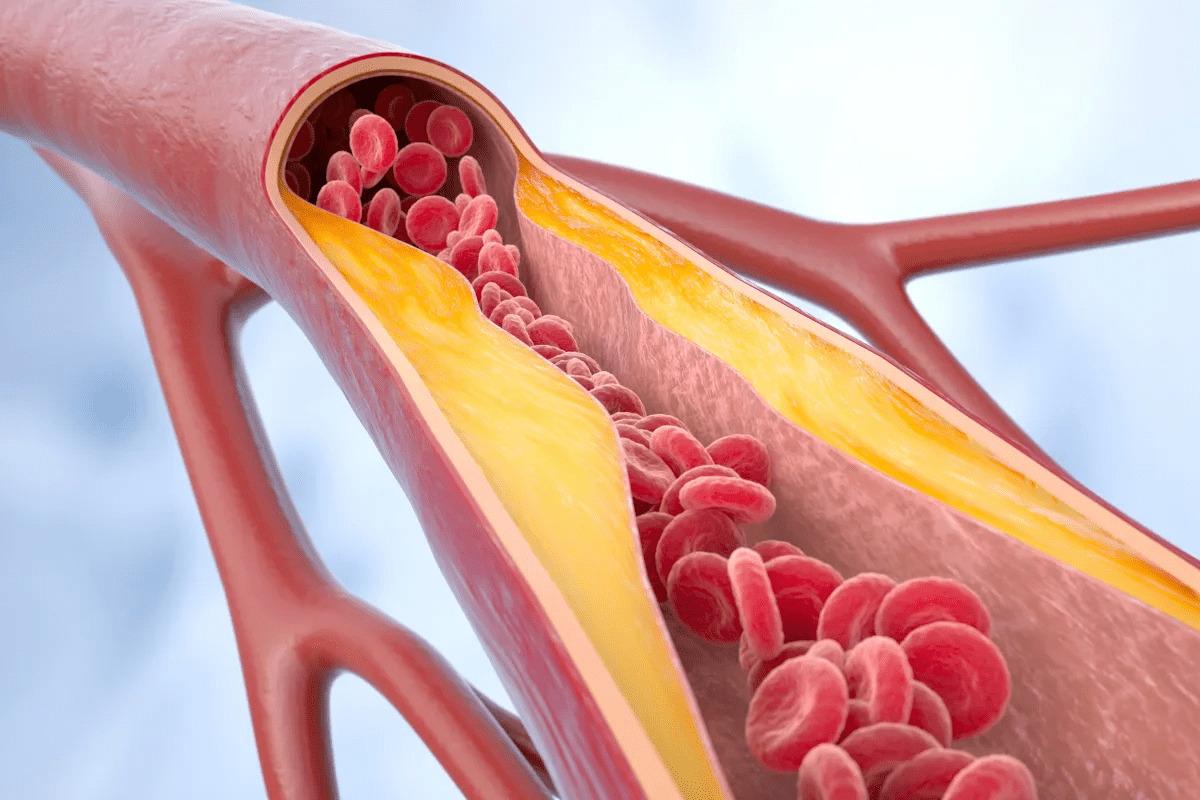
Nearly 1 in 5 adults over 65 have carotid artery stenosis. This is when plaque builds up in the carotid arteries. It can lead to

Flying can be scary, even more so for those with health issues like carotid stenosis or occlusion. A big worry is whether flying could lead
Nearly 800,000 Americans suffer from strokes each year. Carotid artery disease is a big reason for these strokes. carotid artery disease happens when plaque builds
Nearly 1 in 3 adults in the United States has high blood pressure. This is a big risk for heart disease, often caused by poor

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)