
Getting a cardiac device like a pacemaker is a big step in managing heart rhythm issues. But, the journey doesn’t stop there. It’s important to follow certain guidelines for a smooth recovery and to make sure the device works well. We know it can be tough to figure out what to do after getting a pacemaker, but knowing what to do is key to success.After pacemaker, what to avoid? Dangerous magnets and heavy lifting. Get best care tips. Following rules is vital for an amazing recovery.
After getting an artificial pacemaker, you need to take some precautions. This is to avoid problems and make sure the device does its job. It’s about making smart choices to keep your health safe and your heart rhythm in check.
Key Takeaways
- Understand the importance of post-pacemaker implantation guidelines.
- Learn what activities to avoid for a smooth recovery.
- Discover how to ensure optimal device function.
- Find out how to manage your heart rhythm effectively.
- Know when to seek medical attention post-implantation.
Understanding Your Pacemaker and Initial Recovery
Living with a pacemaker can be easier if you know how it works and what to expect at first. Getting a pacemaker is a big step in managing heart health. Knowing more can make the journey smoother.
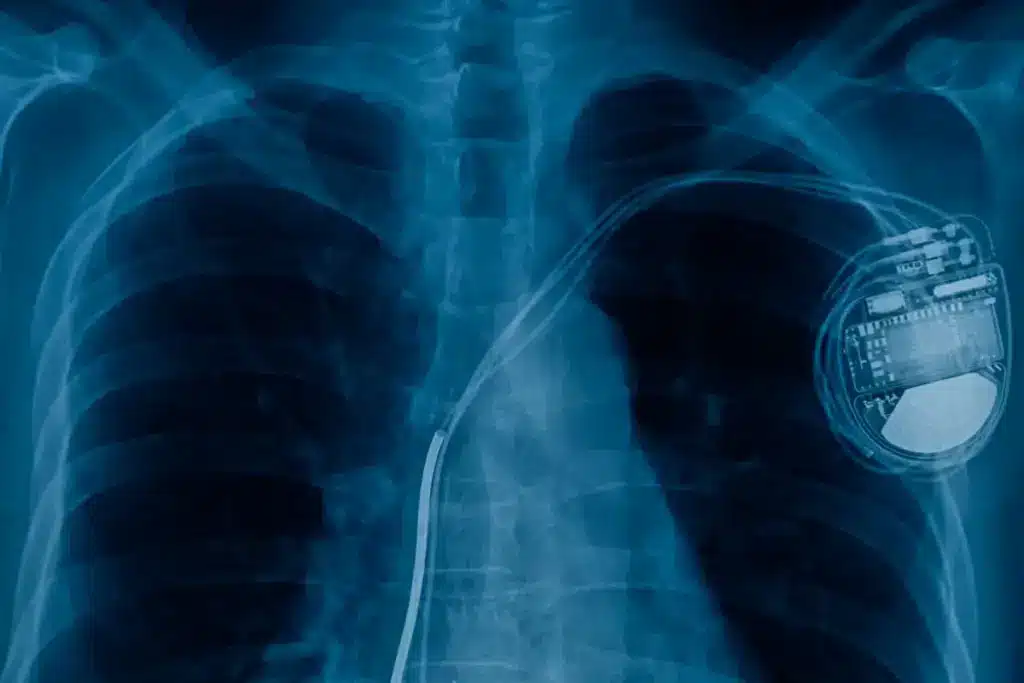
How Pacemakers Function in the Heart

A pacemaker is a small device that helps control your heartbeat. It sends electrical impulses to make the heart muscle contract. This implantable cardiac device is placed under the skin in your chest.
It has leads that connect to your heart. The pacemaker watches your heart’s rhythm and steps in when needed to keep a steady beat.
Knowing how a pacemaker works can ease worries. It’s a key arrhythmia treatment for those with irregular heartbeats.
Types of Pacemakers and Their Specific Considerations
There are many types of pacemakers, each with its own needs. Traditional pacemakers have a pulse generator and leads. Biventricular pacemakers or CRT devices help with heart failure by syncing the heartbeat.
Leadless pacemakers are smaller and go directly into the heart. They’re less invasive and may lower the risk of complications.
General Recovery Timeline Expectations
The first few weeks after getting a pacemaker are key for recovery. Most people can get back to normal in 7 to 10 days. But, they should avoid hard activities for longer.
It’s important to follow your doctor’s advice. They can give you personalized tips based on your situation and the procedure.
While recovering, watch for any signs of trouble like infection or pacemaker issues. Regular check-ups with a cardiology specialist are vital. They help make sure the pacemaker is working right and answer any questions.
Immediate Post-Surgery Restrictions
After getting a pacemaker, it’s key to follow certain rules for a smooth recovery. The first days after surgery are very important for a good outcome.
First 24-48 Hours Critical Care Guidelines
The first 24 to 48 hours after surgery are very important. Patients usually stay in the hospital to check if the pacemaker works right. Listening to the healthcare team’s guidance on rest, medication, and activity levels is crucial for recovery.
First Week Movement Limitations
In the first week, moving too much should be avoided to keep the pacemaker in place. Patients should not lift heavy things, bend, or stretch too much. Gentle movements are okay, but always check with the healthcare provider.
- Avoid lifting anything heavier than 5 pounds.
- Limit reaching or stretching overhead.
- Minimize bending or twisting.
Proper Incision Site Care and Monitoring
Keeping the incision site clean and dry is very important. This helps prevent infection and helps it heal. Watch for signs of infection, like redness, swelling, or more pain, and tell the healthcare provider right away.
a cardiovascular surgeon, says, “Taking care of the wound is key to avoid problems and help it heal.”
Physical Activities to Avoid with Your Pacemaker
After getting a pacemaker, it’s key to know which activities to skip. This helps your device work right and heals properly. Some activities might mess with your pacemaker or slow down healing.
Arm and Shoulder Movement Restrictions
Right after the surgery, don’t move the arm on the pacemaker side too much. Keep arm and shoulder movements calm for a few weeks. This stops the pacemaker leads from moving out of place.
- Avoid lifting your arm above your shoulder.
- Refrain from stretching or reaching out to the sides or backwards.
- Minimize heavy pulling or pushing actions.
Heavy Lifting and Strenuous Exercise Limitations
Heavy lifting and hard exercises can stress your pacemaker and the area around it. We suggest avoiding:
- Lifting objects heavier than 5 pounds (2.3 kg).
- Engaging in strenuous activities like weightlifting or high-intensity workouts.
- Participating in activities that involve sudden, jerky movements.
Some tests, like a nuclear stress test procedure or thallium stress test, might be suggested by your doctor. But, talk to your doctor about how they might affect your pacemaker.
Contact Sports and High-Impact Activities
Playing contact sports or doing high-impact activities can risk your pacemaker. Avoid:
- Contact sports like football, rugby, or hockey.
- High-impact aerobics or running.
- Any activity that could result in a direct blow to the pacemaker site.
Even though you should skip these, staying active is important. Always check with your doctor before starting or changing your exercise routine with a pacemaker.
Electronic Devices and Electromagnetic Interference Concerns
People with pacemakers often worry about using common devices. It’s normal to be concerned about how these activities might affect your health and pacemaker. We get it.
Household Appliances Safety Guidelines
Most household appliances are safe for pacemaker users. But, it’s key to follow some rules to avoid interference. Keep at least 6 inches away from things like microwaves and electric razors.
Also, don’t lean against or stand near big appliances when they’re on. They might make stronger fields. If you feel dizzy or your heart skips a beat, get away and talk to your doctor.
Cell Phones and Wireless Technology Precautions
Cell phones are usually okay to use. Just hold it on the ear away from your pacemaker. And don’t put it in a pocket near your pacemaker. Wireless tech like Wi-Fi and Bluetooth is also safe when used right.
But, to be safe, don’t lean against or stand too close to strong wireless devices. If you’re worried about a device, talk to your doctor.
Security Systems and Metal Detectors
When going through security, tell them you have a pacemaker. Ask for a manual search or an alternative if you can. Don’t stay near or lean against security systems to avoid interference.
Metal detectors, like those at airports or in industrial places, can be a problem. Tell the operator about your pacemaker. They might adjust the device or find another way to check you.
Medical Procedures Requiring Special Pacemaker Precautions
It’s very important for pacemaker patients to tell their doctors about their device before any medical procedure. Some procedures need special care to make sure the pacemaker works right and safely.
Compatibility Issues with MRI and Alternative Options
Magnetic Resonance Imaging (MRI) is a common tool for doctors, but it can be risky for pacemaker patients. The strong magnetic fields in MRI can be a problem. It’s key to check if your pacemaker is MRI-safe before getting an MRI.
If your pacemaker isn’t MRI-safe, you might need to use other imaging methods like CT scans or ultrasound instead.
“The MRI compatibility of a pacemaker is a critical factor in determining the safety of undergoing an MRI,” a study in a leading medical journal says.
“Patients with MRI-compatible pacemakers can safely undergo MRI scans under controlled conditions, but careful monitoring is necessary.”
Nuclear Stress Tests and Imaging Considerations
Nuclear stress tests use small amounts of radioactive material to see the heart. They help find coronary artery disease. It’s important to tell your cardiologist about your pacemaker before this test, as some medications might need to be changed.
Using Lexiscan in nuclear stress tests is usually safe for pacemaker patients. But, it’s best to have a healthcare professional who knows about cardiac devices guide the test.
- Inform your doctor about your pacemaker before the test.
- Discuss any concerns or risks related to your pacemaker and the stress test medication.
- Follow any pre-test instructions carefully.
Dental Procedures and Other Medical Treatments
Dental procedures, including those with ultrasonic devices, and other treatments like electrocautery need care when done on pacemaker patients. Most dental work is safe, but it’s wise to check with your cardiologist or the device maker for advice.
Some treatments might affect your pacemaker. So, it’s important to take the right precautions. For example, using bipolar cautery or taking special steps during electrocautery can help avoid problems with your pacemaker.
Knowing the precautions for different medical procedures helps pacemaker patients stay safe and ensures their device works well.
Travel Considerations for Pacemaker Patients
Traveling with a pacemaker requires some extra planning. But with the right info, you can handle these challenges well. As you plan your trip, think about a few key things to keep you safe and comfortable.
Airport Security Screening Procedures
At airports, you might face extra security checks because of your pacemaker. Tell the security team about your pacemaker before they start checking you. You can go through security, but try not to stand near scanners for too long.
Carrying a pacemaker ID card is a smart move. It can make the security process easier. Some airports have special rules for people with medical implants, so being ready can really help.
Flying with a Pacemaker: What to Know
Flying is usually safe for people with pacemakers. But, there are a few things to remember. Air pressure changes shouldn’t affect your pacemaker, but think about your overall health too.
When booking your flight, pick a seat that works for you. Think about what you might need during the flight. Drinking water and moving around can help avoid discomfort.
|
Flying Precautions |
Description |
|---|---|
|
Stay Hydrated |
Drink plenty of water during the flight to prevent dehydration. |
|
Move Periodically |
Get up and move around the cabin periodically to prevent blood clots. |
|
Choose a Suitable Seat |
Consider booking a seat that allows you more legroom or is closer to the lavatories. |
International Travel Preparations and Documentation
International travel needs careful planning. Make sure you have your pacemaker ID card, medical records, and your doctor’s contact info.
Look into the healthcare options at your destination. Also, know any local rules or advice for pacemaker users. This knowledge can make you feel safer and more prepared for your trip.
Also, think about the effects of traveling across time zones. It might change your medication schedule or pacemaker checks. Being organized and informed will make your trip smoother and more enjoyable.
Everyday Activities and Necessary Precautions
Knowing what to do after getting a pacemaker is key to a good recovery. It’s important to understand how daily tasks can affect your pacemaker and health. This knowledge helps you stay safe and healthy.
Driving Restrictions After Implantation
Many people wonder when they can drive again after getting a pacemaker. Usually, we tell patients to wait 24 to 48 hours before driving. This time helps your body heal and lowers the chance of driving problems.
- Make sure your doctor says it’s okay to drive again.
- Watch out for signs like dizziness or fainting that could mean trouble.
Bathing, Swimming, and Water Activities
Enjoying baths and swims is common, but they need caution after a pacemaker. You should wait for your doctor’s okay before getting the implant site wet. It’s best to avoid baths or swims until the incision is fully closed.
Tips for Safe Water Activities:
- Wait for your doctor’s green light.
- Keep the pacemaker area dry until it heals.
- Be careful of strong currents or activities that might strain it.
Recommended Sleeping Positions
Getting a good night’s sleep is important for healing. We advise against sleeping on the side of the pacemaker for a few weeks. This helps avoid discomfort and irritation at the site.
Returning to Work After Pacemaker Implantation
Getting back to work after a pacemaker implant is more than just going back to your job. You need to think about your work environment. This ensures your safety and the best performance of your pacemaker.
Workplace Environment Assessment
Checking your workplace is key. Look for hazards like strong magnetic fields or high-voltage equipment. These could mess with your pacemaker. Do a detailed walk-through to find any risks.
|
Workplace Hazard |
Potential Risk |
Mitigation Strategy |
|---|---|---|
|
Strong Magnetic Fields |
Interference with pacemaker function |
Avoid areas with MRI machines or strong magnets; use alternative equipment when possible. |
|
High-Voltage Equipment |
Potential for electrical shock or interference |
Maintain a safe distance from high-voltage equipment; ensure proper grounding of devices. |
Occupational Hazards to Avoid
Some jobs can be risky for people with pacemakers. Know these risks and how to avoid them. Jobs that require heavy lifting or lots of exercise might need changes to keep you safe.
- Avoid heavy lifting or bending.
- Minimize strenuous activities.
- Be cautious with equipment that could potentially interfere with your pacemaker.
Communicating with Employers and Colleagues
Talking to your employer and coworkers is important. Tell them about your needs and any changes you might need. This could mean adjusting your job or work area for your safety and comfort.
“Open communication is key to successfully returning to work after pacemaker implantation. By discussing your needs and limitations with your employer, you can create a supportive work environment that fosters your recovery and productivity.”
— Medical Professional
Going back to work after a pacemaker implant is a big step. By checking your workplace, avoiding job hazards, and talking openly with your employer and coworkers, you can make a smooth transition back to work.
Diet and Lifestyle Adjustments for Optimal Pacemaker Function
To get the most out of your pacemaker, making some key changes is essential. These adjustments help ensure your device works well and supports your heart health.
Dietary Considerations and Heart-Healthy Eating
Eating heart-healthy is key for pacemaker users. Focus on foods low in saturated fats, cholesterol, and sodium. Here are some good choices:
- Fruits and vegetables rich in antioxidants and fiber
- Whole grains like brown rice, quinoa, and whole-wheat bread
- Lean proteins such as poultry, fish, and legumes
- Low-fat dairy products and calcium-rich foods
Try to avoid foods high in added sugars, saturated fats, and sodium. Staying hydrated with plenty of water is also important.
Alcohol, Caffeine, and Tobacco Effects
Alcohol, caffeine, and tobacco can harm your heart and pacemaker. While some alcohol might be okay, always check with your doctor. Caffeine can change your heart rate and rhythm, so watch how it affects you. Tobacco use is very bad for your heart.
Here are some important points:
- Limit alcohol to what your doctor says is safe
- Watch how caffeine affects your heart rate
- Avoid tobacco to protect your heart
Medication Interactions and Precautions
Some medicines can affect your pacemaker or heart health. For example, metoprolol might need a different dose after a pacemaker is put in. Always:
- Tell your doctor about all medicines and supplements
- Discuss any possible effects on your pacemaker
- Keep your medication list up to date and adjust as needed
Also, tell your doctor about your pacemaker before a nuclear stress test or other tests like a PET scan with Lexiscan (regadenoson). This ensures safety.
By making these dietary and lifestyle changes, you can help your pacemaker work better and keep your heart healthy. Regular check-ups with your doctor are key to making sure your plan stays on track.
When to Contact Your Doctor Immediately
Knowing when to act fast is key after getting a pacemaker. While problems are rare, knowing the signs can help your recovery. It also makes your treatment more effective.
Warning Signs of Complications or Infection
Watch how your body reacts to the pacemaker. Look out for signs of trouble or infection like:
- Redness, swelling, or bleeding at the incision site
- Increasing pain or discomfort
- Fever or chills
- Dizziness or fainting spells
- Shortness of breath or difficulty breathing
If you see these signs, call your doctor right away. Quick action can stop small problems from getting worse.
As one patient noted,
“I was diligent about monitoring my incision site and reported any concerns to my doctor. It made a huge difference in my recovery.”
Symptoms of Pacemaker Malfunction
A malfunctioning pacemaker can show in different ways. Watch for symptoms like:
- Irregular heartbeats or palpitations
- Dizziness or lightheadedness
- Fatigue or weakness
- Swelling in your legs or ankles
If you notice these signs, reach out to your healthcare provider. They might need to adjust your pacemaker or do more tests.
At times, a malfunction might be caught during a check-up or through remote monitoring. Regular visits are key to making sure your pacemaker works right.
Emergency Response Plan Development
It’s important to have a plan for emergencies. Talk to your doctor or a family member about what to do in an emergency. Your plan should include:
- Contact information for your healthcare team
- Nearest hospital or emergency room location
- Any specific instructions related to your pacemaker
Also, keep a list of your medicines and medical history handy. In an emergency, having this info can be very helpful.
Being ready for emergencies can make you feel less worried. It ensures you get the care you need quickly.
For those getting a nuclear stress test, knowing what to expect is important. A nuclear stress test uses a small amount of radioactive dye to see how your heart works under stress. Understanding how is a nuclear stress test done can ease your worries.
A cardiac stress test with dye is done in a medical setting. The test itself takes about 1-2 hours. But, you should plan for more time for getting ready and after the test.
Long-term Care and Maintenance of Your Pacemaker
To get the most from your pacemaker, stick to a long-term care plan. This includes regular check-ups, knowing when the battery needs to be replaced, and using remote monitoring systems.
Regular Check-up Schedule and Importance
Regular visits are key to keeping your pacemaker working right. These appointments let your doctor check the device, make any needed changes, and spot any problems early.
Follow-up visits are usually:
- Every 3 to 6 months for most pacemaker patients
- More often if your doctor thinks it’s needed for your situation
At these visits, your doctor might do tests like a nuclear stress test. This helps check how well your heart works under stress.
|
Check-up Frequency |
Purpose |
|---|---|
|
Every 3-6 months |
Routine assessment of pacemaker function |
|
As needed |
Adjustments or troubleshooting |
Battery Life Expectations and Replacement Procedure
Knowing how long your pacemaker battery will last is important. It helps plan for ongoing support for your heart.
Pacemaker batteries usually last 5 to 15 years. When it’s almost time for a new battery, your doctor will tell you what to expect.
“Pacemaker battery replacement is a relatively straightforward procedure, often less complicated than the initial implantation.”Cardiologist
Remote Monitoring Systems and Technology
Remote monitoring lets your healthcare team keep an eye on your pacemaker and heart from afar. This tech can spot problems early, cutting down on hospital visits.
Some benefits of remote monitoring include:
- Early detection of device or heart-related issues
- Reduced need for in-person follow-ups
- Enhanced peace of mind knowing your condition is being monitored
By sticking to your long-term care plan, you can keep your pacemaker working well for your heart.
Emotional and Psychological Aspects of Living with a Pacemaker
Getting a pacemaker is a big deal, not just a medical step. It changes your life and how you feel. Learning about its impact on your daily life and emotions is key.
Coping with Lifestyle Changes and Limitations
Life with a pacemaker means making changes. You might avoid some activities or be careful with electronics. Knowing what to avoid before tests is also important.
Finding a balance between safety and living fully is important. Talk to your doctor about managing your life with a pacemaker.
Managing Anxiety About Device Dependence
Having a pacemaker can make you worry about needing it all the time. Worrying about its work, battery, or breaking down is common. Learning about your pacemaker and how it’s checked can help.
Knowing about regular checks and remote monitoring can ease worries. Also, learning about tests like nuclear stress tests can help with medical anxiety.
Support Groups and Resources for Pacemaker Patients
Support groups and resources are key for pacemaker patients. They offer emotional support and advice from others who get it.
Understanding tests, like what to eat before a stress test, can help. Being ready can make you feel less anxious.
|
Resource |
Description |
Benefit |
|---|---|---|
|
Support Groups |
Online or in-person groups for sharing experiences |
Emotional support, practical advice |
|
Patient Education Materials |
Brochures, websites, and videos about living with a pacemaker |
Informed decision-making, reduced anxiety |
|
Healthcare Provider Guidance |
Personalized advice and monitoring from healthcare professionals |
Reassurance, tailored care plans |
Using these resources and understanding pacemaker life can help patients manage better. It can improve their life quality.
Conclusion: Living Confidently with Your Pacemaker
An artificial pacemaker is a life-changing device that needs careful care. Knowing how it works helps you keep it running well. This ensures you stay healthy and happy.
We’ve covered important things to avoid after getting a pacemaker. This includes what to do right after surgery and how to take care of it later. By following these tips, you can avoid problems and live confidently with your pacemaker.
Having a pacemaker means being careful with your daily life. But it shouldn’t stop you from doing things you love. With the right steps and regular doctor visits, you can stay active and enjoy life. Your doctors are always there to help, giving advice and answering your questions.
By working with your doctors and following their advice, you can get the most out of your pacemaker. This leads to better heart health and a happier life.
FAQ
What is a pacemaker and how does it work?
A pacemaker is a small device implanted under the skin. It helps control the heartbeat. It sends electrical impulses to keep the heart beating at a normal rate.
How long does it take to recover from pacemaker implantation?
The recovery time varies, but most people can get back to normal in a few days to a week. Always follow your doctor’s specific guidelines.
What are the restrictions after pacemaker implantation?
After implantation, avoid heavy lifting, bending, or strenuous activities for a few days to a week. Also, don’t raise your arm above your shoulder on the side of the implant.
Can I undergo a nuclear stress test with a pacemaker?
Yes, you can have a nuclear stress test with a pacemaker. Tell your doctor about your pacemaker and follow their guidelines. Some pacemakers may need to be reprogrammed before the test.
Are there any electronic devices that I should avoid using with a pacemaker?
Most household appliances are safe, but avoid devices with strong magnetic fields like MRI machines. Be cautious with security systems and metal detectors too.
Can I travel with a pacemaker?
Yes, you can travel with a pacemaker. Carry a pacemaker identification card and tell your airline or travel provider about it before you go.
When can I drive after pacemaker implantation?
Follow your doctor’s advice on driving after implantation. Usually, you’ll need to avoid driving for a few days to a week.
How often should I have my pacemaker checked?
The check-up frequency depends on your pacemaker type and needs. Your doctor will tell you when to come back for follow-up appointments.
Can I bathe or swim after pacemaker implantation?
Avoid submerging the incision site in water until it heals, usually in a few days to a week. After healing, you can bathe or swim, but follow your doctor’s advice.
What are the signs of pacemaker malfunction?
Signs of malfunction include dizziness, fainting, irregular heartbeat, or swelling at the implant site. If you notice these symptoms, contact your doctor right away.
How can I manage anxiety related to my pacemaker?
To manage anxiety, talk to your doctor, join a support group, or try relaxation techniques like deep breathing or meditation.
Are there any dietary restrictions with a pacemaker?
There are no specific dietary restrictions for pacemaker patients. Eating a heart-healthy diet is recommended. This includes fruits, vegetables, and whole grains.
Can I consume alcohol or caffeine with a pacemaker?
Moderate alcohol and caffeine consumption is usually okay. But, it’s important to discuss your situation with your doctor, as too much can affect your heart.
Reference
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMcp1215180









