
Did you know that medical technology has made a big difference for people with pacemakers? At 70, getting a pacemaker can change your life. It gives you a second chance at living fully.
Pacemaker surgery death rate is low. Get best survival facts. 70-year-olds can live amazing, long lives with this vital heart device.
We’ll look at what affects life expectancy with a pacemaker for 70-year-olds. The pacemaker mortality statistics are encouraging. With the right care, many people stay active for years after getting a pacemaker.
It’s important to know the risks and benefits of getting a pacemaker. We’ll talk about the 70-year-old life expectancy and how pacemakers affect health. This will give you a better idea of what to expect.
Key Takeaways
- Pacemaker implantation can significantly improve life expectancy.
- Individual health factors play a critical role in longevity.
- Understanding pacemaker mortality statistics helps in making informed decisions.
- Proper post-implantation care is essential for a healthy life.
- Advancements in pacemaker technology continue to improve outcomes.
Understanding Pacemakers and Their Function
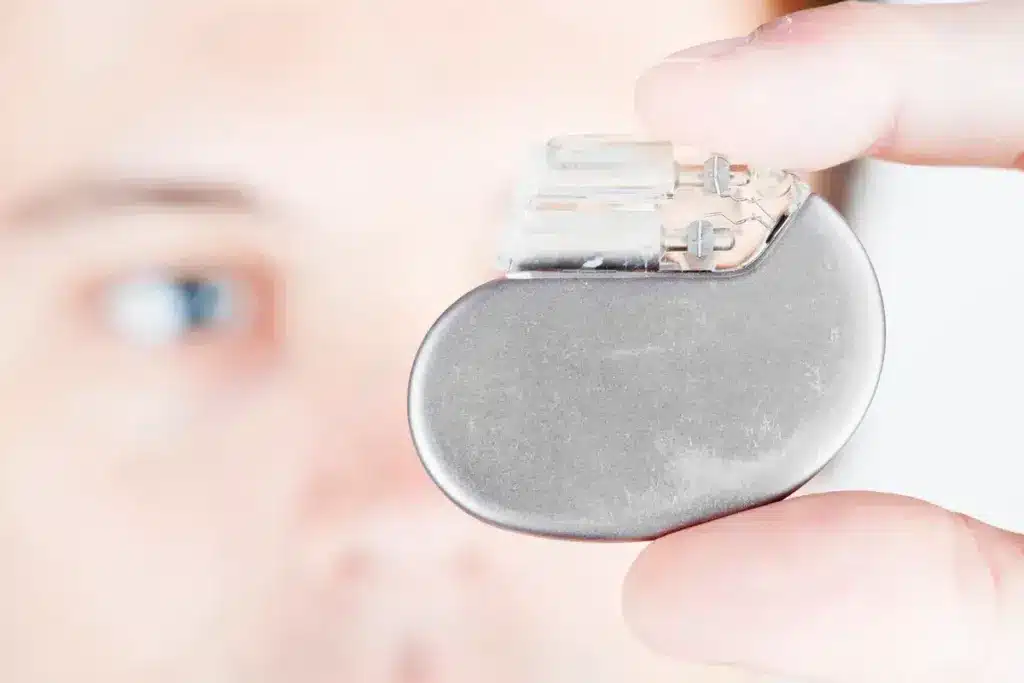
For elderly patients and their caregivers, knowing about pacemakers is key. These devices manage heart rhythm disorders. A pacemaker is a small device that controls the heartbeat by sending electrical impulses. We’ll look at pacemaker basics, types, and when they’re used in elderly patients.
What is a Pacemaker and How Does it Work?
A pacemaker has two main parts: the pulse generator and the leads. The pulse generator is a small metal box with the battery and circuitry. The leads are wires that connect the pulse generator to the heart.
When implanted, it checks the heart’s rhythm and sends impulses as needed. This keeps the heartbeat proper.
Pacemakers can adjust to the patient’s needs. They change the heart rate based on activity or other factors. This helps keep quality of life high for those with heart rhythm disorders.
Types of Pacemakers Available Today
There are many pacemaker types, each for different heart conditions. The main types are:
- Single-Chamber Pacemakers: One lead in the right atrium or ventricle.
- Dual-Chamber Pacemakers: Two leads, one in each chamber, for better pacing.
- Biventricular Pacemakers: Three leads for coordinating left and right ventricles.
Each pacemaker type addresses specific heart rhythm issues. The right pacemaker depends on the patient’s condition and needs.
Indications for Pacemaker Implantation in Elderly Patients
Pacemakers are often suggested for elderly patients with symptoms like dizziness or shortness of breath. Common reasons include:
- Bradycardia: A slow heart rate.
- Heart Block: Delayed or blocked electrical signals.
- Sick Sinus Syndrome: A faulty heart pacemaker.
Choosing to implant a pacemaker involves many tests. These include electrocardiograms and echocardiograms to find the cause of symptoms.
Life Expectancy with a Pacemaker at Age 70

At 70, getting a pacemaker can change your life. It’s important to know how it affects your life span. As we get older, our hearts change, which can affect how well they work. A pacemaker helps the heart beat right, but it also adds new things to think about when it comes to living longer.
Average Life Expectancy Statistics
Research shows that a 70-year-old with a pacemaker can live for 10 to 15 more years. This depends on many health factors. It’s key to remember that these numbers are averages, and life spans can vary.
Factors That Influence Longevity
Many things can affect how long a 70-year-old with a pacemaker will live. These include:
- Other health issues, like heart disease or diabetes
- How healthy the person is, including diet and exercise
- The kind of pacemaker used and how well it works
- How well the person takes care of themselves after the surgery
Managing other health problems well and living a healthy lifestyle can help a lot. It’s also important to see doctors regularly. This helps keep an eye on the pacemaker and the person’s health.
Comparing Life Expectancy With and Without a Pacemaker
Looking at life expectancy with and without a pacemaker is complex. People get pacemakers for heart rhythm problems, which can affect life span. Studies show that people with pacemakers usually live as long as or a bit longer than those without. This is because the pacemaker helps manage serious heart rhythm issues.
New pacemaker technology is making devices better and longer-lasting. This helps people who get them live better lives.
Pacemaker Surgery Death Rate: Understanding the Risks
It’s key for patients and doctors to know the risks of pacemaker surgery. This procedure helps manage heart issues but has its own set of risks and complications.
Immediate Surgical Mortality Statistics
Immediate surgical mortality is about deaths right after or during the pacemaker implantation. The rates are usually low, between 0.1% to 0.5%. These numbers can change based on the patient’s health, other health issues, and the doctor’s skill.
Several factors affect immediate mortality. These include the patient’s age, heart condition, and other serious health problems. For example, those with severe heart failure or other big health issues might face higher risks.
30-Day Mortality Rates
The 30-day mortality rate is another key risk factor for pacemaker surgery. It counts deaths within 30 days of the surgery. Studies show this rate is usually around 1-2%. But, it can be higher for older patients or those with big health problems.
Many factors affect these mortality rates. These include the patient’s health at the time of surgery and the quality of care after surgery.
Long-term Survival Rates After Implantation
Long-term survival after pacemaker implantation is important for patients and their families. Studies show patients with pacemakers often live longer and have a better quality of life than those without. The survival rate depends on the heart condition, age, and other health issues.
Research shows patients with pacemakers can live for many years. For instance, one study found the median survival time is about 8-10 years. But, this can vary a lot based on individual factors.
Age-Related Considerations for Pacemaker Recipients
When older adults get pacemakers, it’s important to understand how age affects results. As people get older, their health, other health issues, and physical state can change how well a pacemaker works. These changes can also affect the risks of using a pacemaker.
How Age Affects Pacemaker Outcomes
Age is a big factor in how well a pacemaker works. Older adults might face more risks because their bodies are not as strong. Research shows that while pacemakers can greatly improve life, older patients might face more problems after the procedure.
Doctors need to know about these age-related issues to help manage what patients expect. For example, older patients might need closer watch and more follow-up care to catch and fix problems early.
Special Considerations for Patients Over 70
People over 70 often have special challenges, like more health problems. These issues can make putting in a pacemaker and taking care of it after harder. Older adults might also be more likely to have problems with their pacemaker, like it not working right or getting infected.
- Doctors should carefully check patients’ health before the procedure to see what risks there are.
- They should set up the pacemaker just right for each person’s needs.
- They should keep a close eye on patients after the procedure to catch and fix any problems fast.
Managing Expectations for Elderly Patients
It’s key to manage what older patients expect when they get a pacemaker. Doctors should talk a lot with patients and their families about what a pacemaker can do and what risks there are. They should talk about how it might make life better, help with symptoms, and maybe even cut down on hospital stays for heart problems.
It’s also important to think about how a pacemaker might affect someone’s mind. Older adults might worry about their device, making lifestyle changes, and future problems. Giving them all the information they need and supporting them can help ease these worries and improve their health.
Common Complications After Pacemaker Implantation
Getting a pacemaker is a big help, but it comes with risks. We’ll look at the short and long-term problems that can happen. It’s key to know about these issues.
Short-term Complications
These problems happen right after or soon after the pacemaker is put in. They include:
- Infection at the site of the pacemaker implantation, which can show as redness, swelling, or drainage.
- Bleeding or hematoma at the site, which might need more surgery.
- Pneumothorax, or a collapsed lung, which is very serious.
- Cardiac perforation, though rare, is a serious issue that can cause tamponade.
Long-term Complications
These problems can show up months or years later. Some include:
- Lead malfunction or displacement, which might need more surgery to fix.
- Pacemaker syndrome, causing dizziness, fatigue, and shortness of breath because of bad pacing.
- Twiddler’s syndrome, where the patient moves the pacemaker, possibly causing lead problems or malfunction.
- Venous thrombosis, or blood clots in veins, which can lead to pulmonary embolism.
Infection Risks and Mortality
Infection is a big risk with pacemakers, leading to more sickness and death. Signs of infection are:
- Redness and swelling at the pacemaker site
- Purulent discharge
- Fever
- General malaise
Managing infection often means antibiotic therapy and, in bad cases, taking out the pacemaker. The risk of dying from pacemaker infection is high. This shows how important it is to catch and treat infections fast.
Knowing about these problems helps set the right expectations for patients. Healthcare workers can then work to lessen these risks. This ensures the best care for those with pacemakers.
Recognizing Heart Problems with a Pacemaker
Knowing the signs of heart trouble is key for pacemaker users. It helps ensure you get help fast. As someone with a pacemaker, knowing the signs of heart problems is vital. This includes signs of a heart attack or cardiac arrest.
Warning Signs of Heart Attack in Pacemaker Patients
Heart attack signs can be hard to spot, but catching them early is critical. Look out for chest pain or discomfort, shortness of breath, nausea, and feeling very tired. It’s important to remember that not all heart attacks cause chest pain.
If you have a pacemaker, watch for these signs closely. If you notice any, get medical help right away.
Gender Differences in Heart Attack Symptoms
Studies show heart attack signs can vary by gender. Women often feel short of breath, nauseous, or very tired. Men usually feel chest pain. Knowing these differences helps doctors and patients get the right treatment fast.
“The symptoms of a heart attack can be different for women than for men. Women are more likely to experience symptoms other than chest pain, such as shortness of breath, nausea, or extreme fatigue.”
When to Seek Emergency Care
If you think you might be having a heart attack, get emergency care right away. Don’t wait; call emergency services or get someone to take you to the hospital.
- Call emergency services if you have severe chest pain or discomfort.
- Go to the hospital right away if you’re having trouble breathing or severe symptoms.
- If you’re not sure about your symptoms, it’s safer to get medical help.
Your health is our main concern as a pacemaker patient. Knowing the signs and acting fast can greatly improve your health and life quality.
Pacemaker Longevity and Replacement Considerations
Modern pacemakers are made to last a long time. But, how long they last depends on several things. Knowing these factors helps manage patient care and expectations.
How Long Do Modern Pacemakers Last?
The life of a pacemaker depends on its type, the patient’s health, and how it’s set up. On average, a pacemaker can last from 5 to 15 years. Thanks to new technology, batteries last longer and devices work better.
Things that affect how long a pacemaker lasts include how often it’s used and how much energy it needs. Regular checks help see how the device is doing and when it might need to be replaced.
The Battery Replacement Procedure
When a pacemaker’s battery is almost gone, it needs to be replaced. This is a less invasive procedure than when it was first put in. The old generator is taken out and a new one is put in, usually under local anesthesia.
The replacement surgery is usually simple and has a low risk of problems. But, as with any surgery, there are risks like infection or a bad reaction to the anesthesia.
Risks Associated with Replacement Surgeries
Even though pacemaker replacement surgeries are mostly safe, there are risks. These include infection, bleeding, and damage to nearby tissue or the pacemaker leads. Choosing a skilled healthcare provider can lower these risks.
Patients should carefully follow the instructions after surgery to avoid complications. Regular check-ups are also key to watching the new device and heart health.
Quality of Life After Pacemaker Implantation
Getting a pacemaker can change your life for the better. It brings hope and energy back. We look at how it affects your life, including physical, mental, and lifestyle changes.
Physical Improvements and Limitations
A pacemaker can make you feel better physically. You might not get tired as easily or feel dizzy. This means you can be more active.
Regular physical activity becomes possible again. Some people can even do things they couldn’t do before.
But, there are also things you can’t do. Avoiding strong magnetic fields or certain equipment is important. Knowing these limits helps keep your pacemaker working right.
Psychological Impact of Living with a Pacemaker
The mental side of having a pacemaker is big. Knowing it helps your heart can give you peace of mind. But, some might feel anxious or sad about it.
Doctors should help with these feelings. They can offer counseling, support groups, and teach about living with a pacemaker. This helps patients adjust and do well.
Daily Activities and Lifestyle Adjustments
Having a pacemaker means making some changes in your life. Simple steps, like being careful during medical tests, can make a big difference. Patients are advised to eat well and exercise to keep their heart healthy.
New pacemaker tech makes it easier to stay active. Many modern pacemakers work well with daily life. They can even be checked from afar, cutting down on hospital visits.
Monitoring and Follow-up Care for Pacemaker Patients
Monitoring and follow-up care are key for pacemaker patients. They help ensure the device works right and fix any problems fast. We’ll talk about the important parts of follow-up care for pacemaker users.
Regular Check-up Schedule
Pacemaker patients need regular check-ups with their doctor. These visits are usually every 3 to 6 months. It depends on the pacemaker type and the patient’s health.
At these visits, the doctor will:
- Check the pacemaker’s battery life
- Adjust the device settings as needed
- Look for any complications
- Check the patient’s heart health
Remote Monitoring Technologies
Remote monitoring has changed follow-up care for pacemaker patients. It lets doctors watch the device and heart rhythm all the time. This helps find problems early.
Some good things about remote monitoring are:
- Less need for in-person visits
- Finding device or heart rhythm problems early
- Better patient outcomes with quick help
The table below shows what remote monitoring can do:
|
Feature |
Description |
Benefit |
|---|---|---|
|
Continuous Monitoring |
Always watching pacemaker function and heart rhythm |
Finding problems early |
|
Automated Alerts |
Healthcare providers get alerts for odd readings |
Quick help for better results |
|
Data Analysis |
Looking at all device and heart rhythm data |
Better decisions for patient care |
Signs That Require Immediate Medical Attention
Pacemaker patients should know when to get help fast. Look out for:
- Heart attack symptoms like chest pain or trouble breathing
- Dizziness or fainting
- Irregular heartbeats or palpitations
- Infection signs at the pacemaker site, like redness, swelling, or fever
Seeing these signs and getting emergency care is key. It helps avoid serious problems and keeps outcomes good.
Impact of Underlying Heart Conditions on Survival
Heart conditions can greatly affect how long elderly patients with pacemakers live. It’s important to know how these conditions can change a 70-year-old’s life with a pacemaker.
How Different Heart Conditions Affect Outcomes
Heart conditions like heart failure or coronary artery disease can change survival rates. We will look at how these conditions affect patients and what it means for their care.
- Heart Failure: Patients with heart failure may have lower survival rates because the disease gets worse over time.
- Coronary Artery Disease: This disease can make pacemaker treatment harder, which might affect how long a patient lives.
- Atrial Fibrillation: This condition raises the risk of stroke and heart failure, which can shorten a patient’s life.
Managing Comorbidities in Elderly Pacemaker Recipients
Managing other health issues is key to helping elderly pacemaker patients live longer. This means using the right medicines, making lifestyle changes, and keeping an eye on their health.
Important steps include:
- Adjusting medicines to handle heart problems and other health issues.
- Helping patients make healthy lifestyle choices like eating right, exercising, and quitting smoking.
- Regular check-ups to watch how the pacemaker and heart are doing.
The Role of Comprehensive Cardiac Care
Comprehensive cardiac care is essential for better survival rates in pacemaker patients. It involves a team of doctors working together to care for the patient.
The benefits of this care are:
- Better handling of heart conditions and other health problems.
- More support and education for patients.
- Improved results thanks to team care and regular checks.
By understanding heart conditions’ impact and using complete cardiac care, we can help elderly pacemaker patients live better lives.
Technological Advancements in Pacemaker Technology
Pacemaker technology is changing fast, bringing hope to people all over the world. We’re making big strides in cardiac care. This is great news for the elderly.
Recent Innovations Improving Outcomes
In recent years, pacemakers have gotten a lot better. They last longer, work smarter, and keep a closer eye on your heart. These changes mean better lives for patients.
- Enhanced Battery Life: New pacemakers last longer, so you don’t need to get them replaced as often.
- Advanced Programming: These pacemakers can adjust to your heart’s rhythm better, fitting your needs perfectly.
- Remote Monitoring: Now, doctors can check on you from afar. This means fewer trips to the hospital and quicker help when you need it.
MRI-Compatible Pacemakers
One big leap forward is MRI-compatible pacemakers. These let patients safely get MRI scans, something old pacemakers couldn’t handle.
Benefits of MRI-Compatible Pacemakers:
- They let you get MRI scans, giving doctors more info to help you.
- They lower the risk of problems that MRI scans can cause with old pacemakers.
- They help doctors diagnose more conditions accurately.
Leadless Pacemakers and Their Benefits for Elderly Patients
Leadless pacemakers are another big step forward, great for older patients. They go straight into your heart, avoiding the need for leads that can cause issues.
- Reduced Risk of Lead-Related Complications: Without leads, there’s less chance of them breaking or moving out of place.
- Minimally Invasive Procedure: Getting one of these pacemakers is less invasive than the old way.
- Improved Cosmetic Outcome: You won’t have a visible pacemaker pocket, making it look better under your skin.
These new pacemaker technologies are changing how we treat heart rhythm problems. They offer better care, a better life, and more peace of mind for the elderly.
Lifestyle Factors Affecting Pacemaker Longevity and Patient Survival
The life of a pacemaker and a patient’s health are closely tied to lifestyle. As we get older, our lifestyle choices become more critical. They help keep our health and pacemaker working well.
Diet and Nutrition Recommendations
Eating right is key for pacemaker users. We suggest eating lots of fruits, veggies, whole grains, and lean proteins. It’s also good to watch sodium intake. Too much sodium can raise blood pressure and make the heart work harder.
Nutritional Tips:
- Eat more omega-3 fatty acids from fish like salmon and sardines.
- Go for low-fat dairy and lean meats.
- Stay away from foods high in sodium and preservatives.
The American Heart Association says, “A healthy diet is vital for heart health and pacemaker safety.”
Exercise Guidelines for Pacemaker Recipients
Exercise is key for heart health and feeling good. But, it’s important to follow safe and effective guidelines.
Exercise Recommendations:
- Do moderate-intensity activities like brisk walking, cycling, or swimming.
- Try to do at least 150 minutes of this exercise each week.
- Add strength training to your routine two times a week.
A study in the Journal of the American College of Cardiology found, “Exercise can greatly improve life quality and function in pacemaker users.”
Stress Management and Mental Health Considerations
Stress management and mental health are key for pacemaker users. Chronic stress can harm the heart. So, finding ways to manage stress is important.
Stress Management Tips:
- Try relaxation methods like deep breathing, meditation, or yoga.
- Do things that make you happy and reduce stress.
- If stress is too much, talk to a mental health expert.
“Reducing stress through mindfulness and relaxation can have a positive impact on heart health and overall well-being.” – A Cardiologist
By focusing on these lifestyle factors, pacemaker users can improve their health. They can also make their device last longer and lower the risk of problems.
Comparing Pacemakers to Other Cardiac Interventions for Seniors
Pacemakers are a common treatment for heart conditions in seniors. But how do they stack up against other treatments? As the population ages, it’s key to understand the various heart health options.
When looking at cardiac interventions for seniors, several factors matter. These include the patient’s health, the heart condition, and the risks and benefits of each treatment.
Pacemakers vs. Medication Management
Medication is often the first treatment for heart conditions. But for bradycardia or heart block, pacemakers might be better. Let’s compare these two to see their benefits.
|
Treatment Aspect |
Pacemakers |
Medication Management |
|---|---|---|
|
Effectiveness for Bradycardia |
Highly effective |
Moderately effective |
|
Risk of Complications |
Surgical risks, device malfunction |
Side effects, dosage management |
|
Long-term Management |
Battery replacement, monitoring |
Ongoing medication adjustments |
Pacemakers vs. ICDs in Elderly Patients
ICDs are used for patients at risk of dangerous arrhythmias. Pacemakers and ICDs are both implantable devices but serve different purposes. It’s important for elderly patients and their doctors to understand these differences.
Key differences between pacemakers and ICDs:
- Pacemakers mainly regulate heart rhythm to prevent it from beating too slowly.
- ICDs can prevent sudden death from dangerous arrhythmias by delivering an electric shock.
Combined Approaches for Optimal Outcomes
Often, a mix of treatments works best. For example, a patient might get a pacemaker and take medication for other heart health issues. We look at how combining treatments can lead to better results for seniors.
The future of cardiac care is in personalized plans tailored to each elderly patient’s needs. By mixing different interventions, doctors can provide more complete care. This improves quality of life and longevity.
Decision-Making Process: Is a Pacemaker Right for a 70-Year-Old?
Deciding if a 70-year-old needs a pacemaker is complex. It involves looking at their health, medical history, and what they prefer. This process needs a deep understanding of the patient’s situation.
Risk-Benefit Analysis for Elderly Patients
When thinking about pacemakers for seniors, weighing risks and benefits is key. We look at how a pacemaker can help the heart and ease symptoms. But we also consider possible surgery problems and issues with the device itself.
A cardiologist, says, “Choosing the right patient for a pacemaker is critical. It’s about picking those who will really benefit from it.”
“The decision to implant a pacemaker should be made on a case-by-case basis, taking into account the individual’s unique needs and circumstances.”
Discussing Options with Healthcare Providers
Talking to doctors about options is a big part of making a decision. Patients should openly discuss pacemaker implantation with their doctors. This helps them understand what it means for their health.
We suggest patients ask their doctors about the good and bad of pacemakers. They should also learn about other treatment choices. This talk helps make a choice that fits the patient’s life and values.
Considering Patient Preferences and Quality of Life
What patients want and how they live affects the decision. We think about their lifestyle, goals, and hopes when deciding on a pacemaker.
For example, someone who wants to stay independent might find a pacemaker helpful. But someone with many health issues might need a different approach. This depends on their health and how long they might live.
Conclusion: Living Well with a Pacemaker in Later Life
Living with a pacemaker at 70 can greatly improve heart health and quality of life. With the right care and lifestyle changes, people can live active and fulfilling lives. Knowing about the pacemaker surgery death rate and survival rate can ease worries and help make decisions.
Elderly patients can live longer and better by managing heart conditions and adopting healthy habits. Regular check-ups and care are key to keeping the pacemaker working right and handling any issues.
New advancements in pacemaker technology are making treatment better for patients. By staying updated and working with healthcare providers, people can get the most out of their treatment. This way, they can enjoy a long and healthy life with a pacemaker.
FAQ
What is the average life expectancy for a 70-year-old with a pacemaker?
The life expectancy for a 70-year-old with a pacemaker varies. It depends on their health, heart conditions, and pacemaker type. Studies show patients can live 10-15 years or more after getting a pacemaker.
What are the risks associated with pacemaker implantation?
Risks include surgery death, infection, and procedure complications. Death risk is less than 1% during surgery. But, overall complication risk is 2-5%.
How long do modern pacemakers last?
Modern pacemakers last 5-15 years. Battery life depends on pacing frequency, pacemaker type, and heart condition.
What are the signs of heart attack in patients with pacemakers?
Heart attack signs are the same as without pacemakers. They include chest pain, shortness of breath, and dizziness. Patients with pacemakers might also feel palpitations or heart rate changes.
Can a pacemaker prevent a heart attack?
Pacemakers regulate heart rhythm and prevent arrhythmias. But, they can’t prevent heart attacks. They’re not a substitute for heart disease prevention.
How often should a pacemaker be checked?
Check frequency varies by pacemaker type and patient condition. Usually, patients need check-ups every 3-6 months to ensure the device works right.
What lifestyle changes are recommended for patients with pacemakers?
Patients should eat well, exercise regularly, manage stress, and avoid smoking. They should also follow their doctor’s advice on physical activities and lifestyle.
Can I undergo an MRI with a pacemaker?
Some pacemakers are MRI-compatible. But, not all are. Always check with your doctor before getting an MRI.
What is the difference between a pacemaker and an ICD?
Pacemakers regulate heart rhythm. ICDs prevent sudden death by shocking the heart. They’re used for different heart conditions and patients.
How does age affect the outcome of pacemaker implantation?
Age can increase risks of complications and death. But, many older patients benefit from pacemakers. Age alone doesn’t mean you can’t get one.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/1258752/









