Last Updated on October 21, 2025 by mcelik
Myelodysplastic syndromes (MDS) affect thousands of people worldwide. They cause a big burden on patients and healthcare systems. A diagnosis of MDS can be daunting, because it has a high risk of turning into acute myeloid leukemia.
For many patients, stem cell transplant is a potentially curative treatment. Recent advances in transplant techniques and supportive care have made outcomes better for MDS patients.
Key Takeaways
- MDS is a group of disorders caused by poorly formed or dysfunctional blood cells.
- Stem cell transplant is considered a potentially curative treatment for MDS.
- Recent advances in transplant techniques have improved patient outcomes.
- Understanding the risks and benefits is key for MDS patients considering transplant.
- Eligibility for transplant depends on various factors, including patient health and MDS subtype.
Understanding Myelodysplastic Syndrome (MDS)
Myelodysplastic syndrome (MDS) is a disorder that affects the bone marrow. It makes it hard for the bone marrow to produce healthy blood cells.
What is MDS and the Myelodysplastic Process
Myelodysplastic syndromes happen when the bone marrow can’t make enough healthy blood cells. This leads to problems like anemia, infections, and bleeding. The myelodysplastic process is when blood cells in the bone marrow grow abnormally.
Common Symptoms and Progression Patterns
Symptoms of MDS can differ but often include feeling tired, short of breath, and getting sick more easily. The disease can progress in different ways. Some people stay stable for a long time, while others quickly get worse and turn into leukemia.
- Fatigue and weakness
- Shortness of breath
- Pale skin
- Increased infections
- Bleeding or bruising easily
Risk Factors and Causes of MDS
The exact cause of MDS is not always known. But, some risk factors for MDS have been found. These include being exposed to chemicals like benzene, having certain genetic disorders, and having had chemotherapy or radiation therapy before.
| Risk Factor | Description |
| Age | MDS is more common in older adults. |
| Chemical Exposure | Exposure to chemicals like benzene. |
| Genetic Disorders | Certain genetic conditions can increase the risk. |
| Previous Treatment | Previous chemotherapy or radiation therapy. |
Conventional Treatment Options for MDS
Conventional MDS treatments aim to ease symptoms and improve life quality. They are tailored to each patient’s condition and risk level.
Supportive Care and Blood Transfusions
Supportive care is key in managing MDS. It aims to improve life quality. Blood transfusions help manage anemia and low platelet counts, common in MDS. Regular transfusions keep blood cell counts stable, reducing complications.
The need for blood transfusions varies by patient condition and severity of anemia or low platelet counts. Transfusions offer temporary relief but don’t cure MDS.
Growth Factors and Medication-Based Treatments
Growth factors boost blood cell production in MDS patients. Erythropoietin reduces the need for red blood cell transfusions. Other growth factors, like G-CSF, increase white blood cell counts.
Medications like hypomethylating agents and lenalidomide are used in MDS treatment. Hypomethylating agents change gene expression to slow cell growth. Lenalidomide is effective for patients with a specific chromosomal deletion.
| Treatment | Mechanism of Action | Primary Use in MDS |
| Erythropoietin | Stimulates red blood cell production | Reducing red blood cell transfusion need |
| G-CSF | Stimulates white blood cell production | Boosting white blood cell counts |
| Hypomethylating Agents | Alters gene expression to slow disease progression | Treatment of MDS, mostly in high-risk patients |
| Lenalidomide | Modulates immune response and inhibits abnormal cell proliferation | Treatment of MDS with del(5q) abnormality |
When to Consider Transplantation as a Curative Approach
While conventional treatments manage MDS symptoms, stem cell transplantation is the only potentially curative option. The decision to transplant depends on the patient’s risk category, health, and donor availability.
Transplantation is considered for high-risk MDS patients or those not responding to conventional treatments. The risks of transplantation, like graft-versus-host disease and infections, must be weighed against its benefits.
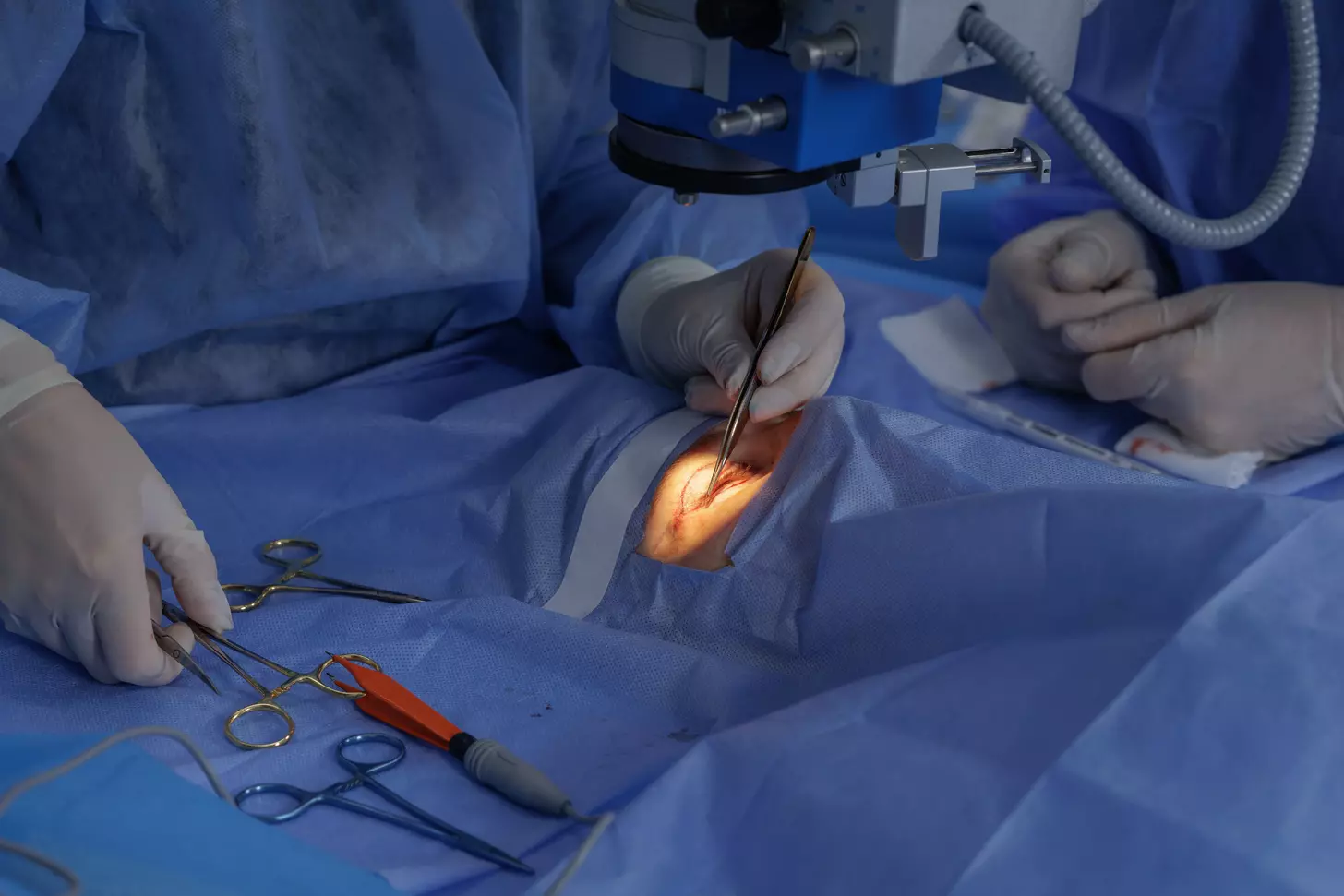
The Procedure: Stem Cell Transplant Explained
Stem cell transplantation is a complex procedure that offers a cure for Myelodysplastic Syndrome (MDS) patients. It replaces damaged stem cells in the bone marrow with healthy ones. This helps the body make normal blood cells again.
How hematopoietic stem cell transplantation works
The process starts with conditioning the patient’s bone marrow. This is done through chemotherapy and/or radiation. It kills the diseased stem cells and weakens the immune system to prevent rejection.
After conditioning, healthy stem cells are infused into the patient’s bloodstream. These stem cells then go to the bone marrow. There, they start making new blood cells.
Key steps in the process include:
- Pre-transplant conditioning
- Stem cell infusion
- Post-transplant recovery and monitoring
Allogeneic vs. autologous transplants for MDS
There are two main types of stem cell transplants: allogeneic and autologous. Allogeneic transplants use stem cells from a donor, often a sibling or unrelated donor. Autologous transplants use the patient’s own stem cells, collected, stored, and then re-infused after conditioning.
| Characteristics | Allogeneic Transplant | Autologous Transplant |
| Donor Source | Donor (related or unrelated) | Patient’s own cells |
| Graft-vs-Host Disease Risk | Yes | No |
| Graft-vs-Leukemia Effect | Yes | No |
Pre-transplant evaluation and preparation
Before a stem cell transplant, patients get a detailed evaluation. This checks their health and if they’re ready for the procedure. This includes:
- Medical history and physical examination
- Laboratory tests (blood work, HLA typing)
- Cardiac and pulmonary function tests
- Infectious disease screening
Understanding the stem cell transplant procedure is key for MDS patients. Knowing how it works, the differences between allogeneic and autologous transplants, and the pre-transplant evaluation helps patients make informed decisions. This way, they can better navigate their care.
Is Stem Cell Transplant the Same as Bone Marrow Transplant?
The terms “stem cell transplant” and “bone marrow transplant” are often used together. But they have different histories and ways of being done. It’s important to know about their past, how they are collected today, and the main differences in their methods.
Historical Context of Bone Marrow Transplantation
Bone marrow transplantation has a long history, starting in the mid-20th century.
Over time, bone marrow transplantation has gotten better. New techniques and care have improved patient results. These changes have also let doctors treat more diseases.
Modern Collection Methods and Terminology
Recently, the term “stem cell transplant” has become more common. This change shows how collection methods have changed. Now, stem cells are often taken from the blood, not directly from the bone marrow. This is done through apheresis, using growth factors to move stem cells into the blood for collection.
This change to blood collection is because it’s less invasive than bone marrow harvesting. But, bone marrow stem cells are sometimes used too. This is when blood collection isn’t possible or when specific stem cells are needed.
Key Differences in Collection Procedures
The main difference is where the stem cells come from. Bone marrow transplants take marrow directly from bones. Stem cell transplants can use marrow or blood stem cells.
| Characteristics | Bone Marrow Transplant | Stem Cell Transplant (Peripheral Blood) |
| Source of Stem Cells | Directly from bone marrow | From peripheral blood after mobilization |
| Collection Method | Surgical extraction under anesthesia | Apheresis after growth factor stimulation |
| Recovery Time | Typically longer due to surgical recovery | Generally shorter as it’s less invasive |
Knowing these differences helps patients and doctors choose the best treatment for conditions like MDS.
Stem Cell Transplant for Myelodysplastic Syndrome: Patient Selection
Choosing the right patients for stem cell transplant in MDS is a detailed process. It looks at the patient’s health, the type of MDS they have, and other important factors. This helps decide if a stem cell transplant is the best treatment.
Determining Transplant Eligibility
Checking if a patient can get a transplant is complex. It looks at their physical health, age, and any other health issues. Eligibility depends on how well the patient can handle the transplant and recover. Doctors carefully evaluate these factors to make sure the patient can safely go through the transplant.
“Choosing to do a stem cell transplant is a big decision,” says a top hematologist. “It needs a detailed check to make sure the benefits are worth the risks for the patient.”
Risk Stratification in MDS
It’s key to figure out who will get the most from a stem cell transplant in MDS. The Revised International Prognostic Scoring System (IPSS-R) helps sort patients by risk level. It looks at things like genetic changes, how many bad cells there are, and if the patient has low blood counts.
Timing of Transplantation in Disease Course
When to do the transplant is also very important. Some patients might need it early, while others might wait until their disease gets worse or doesn’t respond to other treatments. The choice depends on the patient’s risk level and overall health.
Donor Selection and Compatibility Factors
Choosing the right donor is key for stem cell transplants in Myelodysplastic Syndrome (MDS). Several important factors help match the donor and recipient.
HLA Typing and Matching Process
Human Leukocyte Antigen (HLA) typing is essential for finding compatible donors. HLA genes control the immune system. Matching them reduces the risk of complications and boosts transplant success.
The HLA typing process tests the donor and recipient for specific genes. A good match between their HLA genes increases transplant success chances.
Key considerations in HLA typing include:
- The number of HLA loci tested
- The degree of matching required for a successful transplant
- The impact of HLA mismatching on transplant outcomes
Related vs. Unrelated Donor Considerations
Donors can be related or unrelated to the recipient. Siblings, being related, often share more genetic material, improving HLA matching.
Unrelated donors are found through registries. They may not share a genetic background but HLA typing advancements have improved transplant success from them.
“The use of unrelated donors has become increasingly common, thanks to the growth of donor registries worldwide.”
Haploidentical and Cord Blood Options
Haploidentical donors share half of the recipient’s HLA genes, often family members. Advances in transplant techniques have made this option more viable
.

Cord blood transplantation uses stem cells from umbilical cord blood. It’s a good choice when a fully matched donor isn’t available.
Haploidentical and cord blood donors offer alternatives when a fully matched donor isn’t available. Each option has its benefits and risks, including GVHD and immune recovery speed.
Factors to consider for haploidentical and cord blood transplants:
- The degree of HLA mismatch and its impact on GVHD risk
- The cell dose and its effect on engraftment and immune recovery
- The conditioning regimen used to prepare the recipient for the transplant
Stem Cell Transplant Donor Procedure in Detail
The stem cell transplant donor procedure is a detailed process. It starts with checking the donor’s health and if they match the recipient. This step is key for a successful transplant and keeping both the donor and recipient safe.
Donor Evaluation and Clearance Process
The first step is a detailed check to see if the donor is a good match. This includes medical tests, blood work, and looking at the donor’s health history. The goal is to find any risks and make sure the donor is healthy enough for the transplant.
Key components of the donor evaluation include:
- Infectious disease screening
- Blood tests to determine blood type and compatibility
- Medical history review
- Physical examination
Mobilization and Collection Methods
After the donor is cleared, the next step is to get the stem cells ready. This means giving the donor medicine to make more stem cells. These cells then go into the bloodstream and are collected through apheresis.
The collection process takes several hours. The donor might need to be on an apheresis machine for days.
Post-Donation Recovery and Follow-Up
After giving the donation, the donor is watched closely for any problems. The body naturally makes more stem cells over time. It’s important to keep up with follow-up care to make sure the donor is okay.
Post-donation care includes:
- Monitoring for any side effects
- Appointments with the medical team
- Advice on getting back to normal
The stem cell transplant donor procedure is a big deal. It needs careful planning, execution, and follow-up. Knowing the process helps donors prepare for their important role in saving a life.
The Transplantation Process for MDS Patients
The process to transplant MDS patients is complex. It aims for long-term remission. It includes several stages, from preparation to aftercare.

Conditioning Regimens: Myeloablative vs. Reduced-Intensity
Before the transplant, MDS patients go through a conditioning regimen. This prepares their body for the new stem cells. There are two main types: myeloablative and reduced-intensity.
- Myeloablative Conditioning: This intense regimen clears out the old bone marrow. It’s for younger patients with fewer health issues.
- Reduced-Intensity Conditioning: This gentler method is for older patients or those with more health problems. It weakens the immune system to let the new stem cells in.
| Conditioning Regimen | Intensity | Typical Patient Profile |
| Myeloablative | High | Younger, fewer comorbidities |
| Reduced-Intensity | Lower | Older, more comorbidities |
The Stem Cell Infusion Procedure
The stem cell infusion is like a blood transfusion. The stem cells go to the bone marrow. There, they start making new blood cells.
“The stem cell infusion is a painless procedure, and patients typically do not experience significant side effects during the infusion itself.” – Hematologist
Immediate Post-Transplant Hospital Care
After infusion, patients stay in the hospital for weeks. They are watched closely for any problems and helped to recover.
- Monitoring for graft-versus-host disease (GVHD)
- Managing infections and other complications
- Supporting the patient’s nutritional and emotional needs
Knowing the transplant process helps MDS patients prepare. They understand what to expect at each step of their treatment.
MDS Bone Marrow Transplant Survival Rate and Outcomes
Bone marrow transplantation is a promising treatment for MDS. But, its success depends on several factors. These include the disease’s risk category, the patient’s age, and other individual factors.
Statistical Outcomes by Disease Risk Category
The disease risk category greatly affects the outcome of a bone marrow transplant for MDS patients. Research shows that patients with lower-risk MDS tend to have better survival rates. This is compared to those with higher-risk disease.
Survival Rates by Disease Risk:
| Disease Risk Category | 1-Year Survival Rate | 3-Year Survival Rate |
| Low Risk | 80% | 60% |
| Intermediate Risk | 70% | 50% |
| High Risk | 50% | 30% |
Age-Related Survival Considerations
Age is a key factor in the survival rate of MDS patients undergoing bone marrow transplants. Older patients generally have lower survival rates. This is due to comorbidities and reduced tolerance to the transplant procedure.
Age-Related Survival Insights:
- Patients under 60 years: Higher survival rates and better tolerance to the transplant.
- Patients between 60-70 years: Moderate survival rates with careful patient selection.
- Patients over 70 years: Lower survival rates due to increased comorbidities and reduced physical reserve.
Factors Influencing Long-Term Success
Several factors contribute to the long-term success of bone marrow transplants in MDS patients. These include the patient’s overall health, the presence of comorbidities, the donor’s compatibility, and the conditioning regimen used.
Understanding these factors is key to optimizing treatment outcomes. It helps improve the quality of life for MDS patients undergoing bone marrow transplantation.

When MDS Transforms to AML: Transplant Considerations
The change from MDS to AML is a big deal. It means looking at new treatment options, like stem cell transplants. This change affects how well the patient will do and what treatment they need.
MDS Progression to Acute Myeloid Leukemia
When MDS turns into AML, more abnormal cells show up in the bone marrow. This makes it harder for the body to make healthy blood cells. The disease also gets more serious with new genetic changes.
How likely MDS is to turn into AML varies. It depends on the type of MDS, any genetic changes, and other factors.
Acute Myeloid Leukemia Bone Marrow Transplant Approach
Turning to stem cell transplant is key when MDS becomes AML. Choosing between two types of transplant regimens is important. This choice depends on the patient’s age, health, and how the disease is doing.
AML Stem Cell Transplant Prognosis Compared to MDS
The outlook for stem cell transplant in AML from MDS is not as good as for other types of AML or MDS. Several things can affect how well the transplant works. These include how long the MDS lasted, any bad genetic changes, and how well the patient responds to initial treatments.
| Disease State | Transplant Outcome | Prognostic Factors |
| MDS without transformation | Generally better | Cytogenetics, blast percentage |
| AML secondary to MDS | Generally poorer | Duration of MDS, response to chemotherapy |
| De novo AML | Variable | Molecular mutations, cytogenetics |
Knowing these factors helps doctors and patients make better choices. It’s all about understanding the disease and what treatments might work best.
Potential Complications and Management
It’s key for MDS patients to know about the risks of stem cell transplant. This treatment can cure some, but it comes with dangers that need careful handling.
Graft-Versus-Host Disease: Acute and Chronic
Graft-versus-host disease (GVHD) is a big risk with allogeneic stem cell transplant. Here, the donor’s immune cells attack the host’s body. GVHD can be acute or chronic, each with its own symptoms and treatment plans.
- Acute GVHD happens early, within 100 days after transplant. It shows as skin rash, liver issues, or stomach problems.
- Chronic GVHD starts later, after 100 days. It affects many parts of the body, like skin, mouth, eyes, and liver. It needs long-term treatment to keep it under control.
Infections and Immune Reconstitution
Infections are a big worry after stem cell transplant because the immune system is weak. The risk is highest in the early days after transplant. This means patients need antibiotics and close watch.
- The immune system starts to get better over time, but it’s different for everyone.
- Patients should stay safe from germs. This means avoiding crowded places and keeping clean.
Organ Toxicities and Long-Term Effects
Stem cell transplant can cause long-term problems, like damage to organs. These issues come from the treatment itself. Some common problems are:
- Cardiac complications, like heart failure or irregular heartbeats, from chemo or radiation.
- Secondary malignancies, which are rare but can happen long after.
It’s important to keep up with follow-up care to deal with these issues.
Bone Marrow Transplant Age Restrictions and Special Considerations
Medical technology is getting better, and so are the rules for bone marrow transplants. Before, older people faced higher risks and worse results. But now, thanks to new techniques and care, more people can get transplants.
Traditional Age Limits and Current Perspectives
Older than 55-60 used to be too old for transplants. But now, doctors are looking at people up to 70 or more. It depends on their health and the type of transplant.
Doctors check a lot before deciding on a transplant for older adults. They look at the person’s health, other diseases, and the disease itself. Reduced-intensity conditioning regimens help make transplants safer for older patients.
Reduced-Intensity Conditioning for Older Adults
Reduced-intensity conditioning is a gentler way to prepare for a transplant. It doesn’t wipe out the bone marrow like old methods. This is better for older adults because it’s less harsh.
- Lower risk of organ toxicity
- Reduced risk of severe infections
- Potential for quicker recovery
Studies show RIC works well for older patients with myelodysplastic syndrome (MDS). It offers a chance for a cure with fewer side effects.
Comorbidity Assessment and Geriatric Evaluation
Checking for other health problems is key for older transplant candidates. Conditions like heart disease or diabetes can affect how well they do. A geriatric assessment helps doctors understand the patient’s overall health.
“A geriatric assessment is essential in identifying older adults who are likely to benefit from bone marrow transplantation while minimizing the risk of adverse outcomes.” –
Expert in Hematology and Oncology
Using comorbidity and geriatric assessments helps tailor transplant plans for older adults. It makes sure the benefits outweigh the risks.
Conclusion: The Curative Potential of Stem Cell Transplantation for MDS
Stem cell transplantation is a promising treatment for Myelodysplastic Syndrome (MDS). It offers hope to those diagnosed with this complex condition. This treatment can replace bad bone marrow with healthy stem cells, possibly curing the disease.
We’ve looked at how stem cell transplant works for MDS. This includes who can get it, finding a good match, and the transplant process. Knowing these details helps patients and doctors make better choices.
Stem cell transplant is a key treatment for MDS. It can be a cure for those who qualify. As research grows, more people will have access to this treatment. This means a better future for those with MDS.
FAQ
What is Myelodysplastic Syndrome (MDS) and how is it related to stem cell transplant?
Myelodysplastic Syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells. This often leads to bone marrow failure. Stem cell transplant is a treatment that aims to replace the diseased bone marrow with healthy stem cells.
Is stem cell transplant the same as bone marrow transplant?
Stem cell transplant and bone marrow transplant are similar but not the same. Both involve transplanting stem cells. The main difference is where the stem cells come from. Bone marrow transplant traditionally uses stem cells from the bone marrow. Stem cell transplant can use stem cells from the blood or bone marrow.
What are the conventional treatment options for MDS before considering stem cell transplant?
Treatments for MDS include supportive care like blood transfusions. Medications are used to manage symptoms and improve quality of life. Growth factors help stimulate healthy blood cell production.
How is a donor selected for a stem cell transplant?
Donor selection is based on HLA typing for compatibility. Donors can be related or unrelated. Other options include haploidentical donors and cord blood.
What is the process for a stem cell transplant donor?
The donor process starts with evaluation and clearance. Then, stem cells are mobilized and collected. After donation, donors receive care and follow-up to monitor their recovery.
What are the possible complications of stem cell transplant for MDS?
Complications include graft-versus-host disease (GVHD), infections, and long-term effects like organ toxicities. It’s important to manage these risks.
Are there age restrictions for bone marrow transplant, and how are older adults evaluated?
Age limits for bone marrow transplant have changed. Reduced-intensity conditioning regimens make transplant more accessible to older adults. Geriatric evaluation and comorbidity assessment are key in determining eligibility.
How does MDS progression to AML affect transplant considerations?
MDS transforming into Acute Myeloid Leukemia (AML) can change transplant approaches. The prognosis can also differ. Understanding these implications is important for treatment decisions.
What are the survival rates and outcomes for MDS patients undergoing bone marrow transplant?
Survival rates depend on disease risk category, age, and other factors. Statistical outcomes help understand the success of bone marrow transplant for MDS. This information aids in making informed decisions.
What is the significance of stem cell transplant in treating MDS?
Stem cell transplant offers a potentially curative approach for MDS. It provides a new immune system and healthy stem cells. This can improve survival and quality of life.