Last Updated on October 21, 2025 by mcelik
Megaloblastic anemia is when your body makes big red blood cells that don’t work right. Many people around the world have this problem. It’s often because they don’t have enough vitamin B12 or folate.
This condition, also known as macrocytic anemia, messes with how red blood cells are made. This can cause you to feel tired, weak, and have other issues. You can tell you have it if your bone marrow has megaloblasts.
Key Takeaways
- Megaloblastic anemia is characterized by the production of abnormally large red blood cells.
- Vitamin B12 deficiency is a common cause of megaloblastic anemia.
- Folate deficiency can also lead to megaloblastic anemia.
- Symptoms include fatigue, weakness, and shortness of breath.
- Treatment options vary depending on the underlying cause.
Understanding Megaloblastic Anemia
Megaloblastic anemia is a condition where red blood cells don’t form right. It’s caused by a lack of vitamin B12 or folate. These are key for making DNA. Without them, red blood cells can’t grow right, leading to megaloblasts.
Definition and Pathophysiology
Megaloblastic anemia happens when you don’t have enough vitamin B12 or folate. These vitamins are vital for DNA making. Without them, red blood cells can’t grow right, making megaloblasts.
This condition disrupts DNA synthesis in red blood cells. Vitamin B12 and folate are essential for DNA production, and without them, red blood cells develop abnormally, forming megaloblasts.
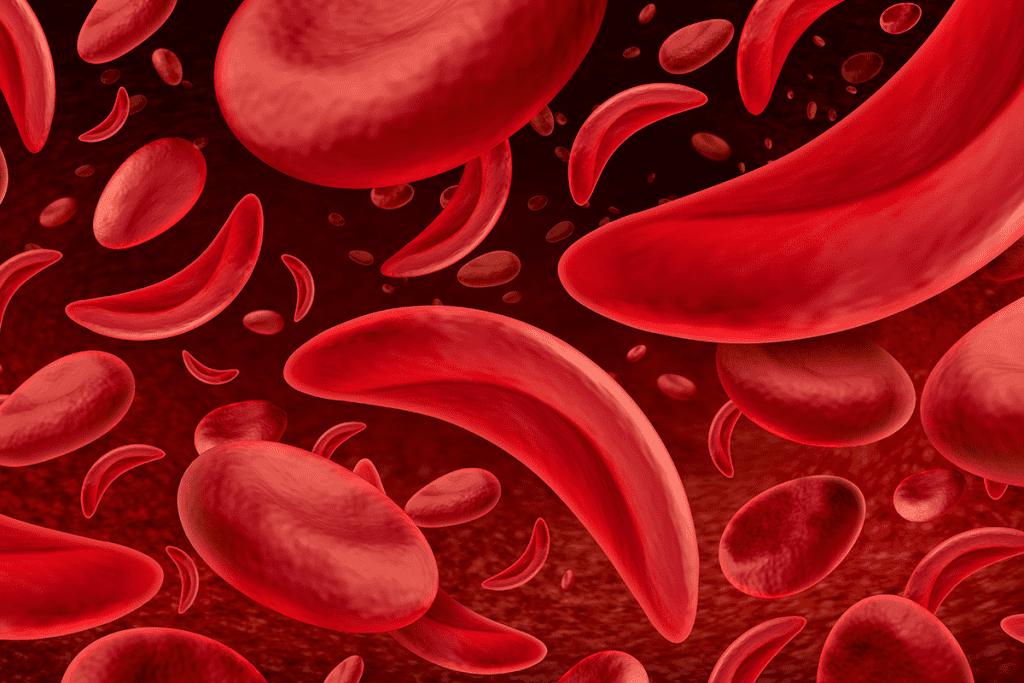
Megaloblasts and Blood Cell Formation
Megaloblasts are big, young red blood cells made in the bone marrow. They happen when you don’t have enough vitamin B12 or folate. These cells show that blood cell making is not working right.
| Characteristics | Normal Red Blood Cells | Megaloblasts |
| Size | 7-8 micrometers | Larger than 8 micrometers |
| Maturation | Properly matured | Immature |
| Functionality | Functional | Non-functional |
Types of Megaloblastic Anemia
It’s important to know the different types of megaloblastic anemia. This condition can be caused by nutritional deficiencies or certain medications.
Vitamin B12 Deficiency-Related Megaloblastic Anemia
Vitamin B12 is key for making DNA and red blood cells. Not having enough vitamin B12 can cause megaloblastic anemia. This is common in people who don’t eat meat or have trouble absorbing nutrients.
The main reasons for vitamin B12 deficiency are:
- Dietary deficiency, mainly in vegans and vegetarians
- Pernicious anemia, an autoimmune condition affecting intrinsic factor production
- Malabsorption due to gastrointestinal disorders or surgery
Folate Deficiency-Related Megaloblastic Anemia
Folate is also vital for DNA and red blood cell production. Not enough folate can cause megaloblastic anemia. This often happens when people don’t eat enough folate or need more during pregnancy.
Common reasons for folate deficiency are:
- Inadequate dietary intake, mainly in people with poor eating habits
- Increased demand during pregnancy or lactation
- Malabsorption due to conditions like celiac disease
Drug-Induced Megaloblastic Anemia
Some medicines can mess with DNA synthesis, causing megaloblastic anemia. This type usually goes away when you stop taking the drug.
Drugs that can cause megaloblastic anemia include:
- Antifolate drugs like methotrexate
- Anticonvulsants such as phenytoin
- Other medications that affect folate or vitamin B12 metabolism
| Type of Megaloblastic Anemia | Causes | Key Characteristics |
| Vitamin B12 Deficiency-Related | Dietary deficiency, pernicious anemia, malabsorption | Often associated with neurological symptoms |
| Folate Deficiency-Related | Inadequate dietary intake, increased demand, malabsorption | Common in pregnancy and malabsorption states |
| Drug-Induced | Antifolate drugs, anticonvulsants, other medications | Reversible upon discontinuation of the offending drug |
Pernicious Anemia: The Most Common Form of Megaloblastic Anemia
Pernicious anemia is the most common type of megaloblastic anemia. It’s caused by an autoimmune issue and a lack of intrinsic factor.
The immune system attacks the stomach cells that make intrinsic factor. This protein is key for vitamin B12 absorption. Without enough vitamin B12, the body can’t make red blood cells or keep the nervous system healthy.
Autoimmune Nature of Pernicious Anemia
Pernicious anemia happens when the immune system attacks the stomach’s parietal cells or intrinsic factor. This attack destroys these cells. As a result, the body can’t absorb vitamin B12 well.
Studies link pernicious anemia to other autoimmune diseases. This suggests a shared risk factor for these conditions.
Intrinsic Factor Deficiency
Intrinsic factor is a protein made by the stomach’s parietal cells. It’s vital for vitamin B12 absorption. It binds to vitamin B12 and helps the small intestine take it in.
In pernicious anemia, the lack of intrinsic factor stops vitamin B12 absorption. This leads to megaloblastic anemia.
Historical Perspective on Pernicious Anemia
Pernicious anemia has been a major health issue for centuries. It was first described as a “pernicious” form of anemia.
The discovery of vitamin B12 changed how we treat pernicious anemia. Before, it was often fatal. But with vitamin B12 injections, it became manageable.
Causes of Megaloblastic Anemia
Megaloblastic anemia happens when red blood cells aren’t made right. This is often because of certain causes. These include what we eat, how well our body absorbs nutrients, and our genes.
Dietary Deficiencies
Diet plays a big part in megaloblastic anemia. Vitamin B12 and folate are key for making DNA. Without enough, our red blood cells get too big. Vegans are at risk because vitamin B12 is mostly in animal products.
Folate is found in leafy greens, legumes, and fortified cereals. But, some people, like pregnant women, need more folate. If they don’t eat enough, they can get a deficiency.
Malabsorption Disorders
Malabsorption disorders also cause megaloblastic anemia. Conditions like celiac disease, Crohn’s disease, and atrophic gastritis make it hard to absorb vitamin B12 and folate. For example, celiac disease damages the small intestine, making it hard to absorb these nutrients.
Pernicious anemia is an autoimmune disease that leads to vitamin B12 deficiency. It happens when the immune system attacks the stomach cells that make intrinsic factor, needed for vitamin B12 absorption.
Genetic Factors
Genetics can also lead to megaloblastic anemia. Some genetic mutations affect how we process vitamin B12 or folate. For instance, a MTHFR gene mutation can lead to high homocysteine levels and problems.
Knowing about these genetic factors is key. It helps us find who’s at risk and how to help them. Genetic tests can spot these issues early, helping us prevent or manage megaloblastic anemia.
Risk Factors for Developing Megaloblastic Anemia
Several factors can increase the risk of getting megaloblastic anemia. These include age, medical conditions, and lifestyle choices. Knowing these risk factors helps identify who might need early screening or preventive steps.
Age-Related Risk Factors
Age is a big risk factor for megaloblastic anemia. Older people are more likely to get it. This is because they might not eat enough essential nutrients, their bodies don’t absorb nutrients as well, and they often have chronic diseases.
- Older adults face a higher risk because their stomach acid levels drop. This is key for vitamin B12 absorption.
- As people get older, their gut changes. This can make it harder to absorb folate and vitamin B12.
Medical Conditions That Increase Risk
Some medical conditions can raise the risk of megaloblastic anemia. These usually affect the gut or how the body uses nutrients.
Common medical conditions that increase the risk:
- Celiac disease damages the small intestine, making it hard to absorb nutrients.
- Crohn’s disease is an inflammatory bowel disease that can hit any part of the gut.
- Pernicious anemia is an autoimmune disease that causes vitamin B12 deficiency.
These conditions can make it tough for the body to absorb important nutrients like vitamin B12 and folate. These are key to avoiding megaloblastic anemia.
Lifestyle and Dietary Risk Factors
Lifestyle and diet choices also matter a lot. Eating a diet that lacks essential nutrients can lead to deficiencies over time.
- A vegetarian or vegan diet might lack vitamin B12 if not supplemented properly.
- Drinking too much alcohol can mess with nutrient absorption and up the risk of deficiencies.
- Not eating enough folate-rich foods, like leafy greens and legumes, is also a risk.
By knowing these risk factors, people can make better diet and lifestyle choices. This can help lower their chance of getting megaloblastic anemia.
Signs and Symptoms of Megaloblastic Anemia
Megaloblastic anemia shows many symptoms, from feeling very tired to neurological problems. It’s important to spot these signs early for treatment.
Common Physical Symptoms
People with megaloblastic anemia often feel very tired, weak, and short of breath. These physical symptoms make everyday tasks hard.
They might also have pale or yellowish skin, a smooth tongue, and less appetite. Some may feel dizzy or lightheaded because their body doesn’t get enough oxygen.
Neurological Manifestations
Megaloblastic anemia can cause neurological manifestations like numbness or tingling in hands and feet. This happens because of a lack of vitamin B12, which is key for the nervous system.
Severe cases might lead to trouble walking, balance issues, and brain function problems. Early treatment can help, but ignoring it can cause permanent damage.
Gastrointestinal Symptoms
Gastrointestinal symptoms include loss of appetite, diarrhea, and weight loss. Some might also have a sore mouth or tongue.
These symptoms can be very uncomfortable and might lead to more nutritional problems. A doctor can help manage them with diet changes and supplements.
In summary, megaloblastic anemia has many symptoms that affect physical, neurological, and gastrointestinal health. Spotting and treating these symptoms early is key to better health outcomes.
Diagnostic Approaches for Megaloblastic Anemia
To diagnose megaloblastic anemia, doctors use several methods. They look at symptoms, run lab tests, and sometimes do special exams.
Blood Tests and Complete Blood Count
Blood tests are key in diagnosing megaloblastic anemia. A complete blood count (CBC) is often the first step. It checks hemoglobin, hematocrit, and red blood cell sizes. In megaloblastic anemia, the CBC shows:
- Macrocytic anemia (elevated mean corpuscular volume, MCV)
- Low reticulocyte count
- Presence of hypersegmented neutrophils
The CBC gives important info on anemia’s severity. It helps tell megaloblastic anemia apart from other anemias.
Bone Marrow Examination
A bone marrow examination may be needed to confirm the diagnosis. This involves taking bone marrow from the hip or sternum. In megaloblastic anemia, the bone marrow shows:
- Megaloblasts, which are large, immature red blood cells
- Erythroid hyperplasia, indicating increased red blood cell production
- Giant metamyelocytes and band forms
This test helps see how much red blood cell production is increased. It also helps rule out other bone marrow issues.
Vitamin Level Testing
Vitamin level testing is vital to find the cause of megaloblastic anemia. Tests check vitamin B12 and folate levels. More tests might include:
- Methylmalonic acid (MMA) and homocysteine levels to assess vitamin B12 deficiency
- Folate levels in red blood cells
These tests help figure out if it’s a vitamin B12 or folate problem. This guides the right treatment.
Specialized Tests for Pernicious Anemia
For those thought to have pernicious anemia, specialized tests are done. These include:
- Intrinsic factor antibody test
- Gastric parietal cell antibody test
- Schilling test (though less used today)
These tests confirm pernicious anemia’s autoimmune cause. They help plan long-term care.
By using these methods, doctors can accurately diagnose megaloblastic anemia. They can find the cause and plan the right treatment.
Megaloblastic Anemia vs. Other Types of Anemia
It’s important to know the differences between megaloblastic anemia and other anemias. Anemia happens when there aren’t enough red blood cells or they’re not good enough. There are many types, each with its own cause and signs.
Comparison with Macrocytic Anemia
Macrocytic anemia means red blood cells are bigger than usual. Megaloblastic anemia is a type of macrocytic anemia. It’s marked by megaloblasts in the bone marrow. Not all macrocytic anemia is megaloblastic, though.
Other reasons for macrocytic anemia include drinking too much alcohol, liver disease, and some medicines. The main difference is the presence of megaloblasts and the reason for the anemia.
Differences from Iron Deficiency Anemia
Iron deficiency anemia happens when the body doesn’t have enough iron for hemoglobin. Hemoglobin is key for red blood cells. This type of anemia makes red blood cells smaller, not bigger like in megaloblastic anemia.
Treating iron deficiency anemia involves iron supplements. But megaloblastic anemia needs vitamin B12 or folate to fix it. Knowing the difference is key for the right treatment.
Distinguishing Features on Laboratory Tests
Lab tests are key in telling megaloblastic anemia apart from other anemias. A complete blood count (CBC) shows red blood cell size and number. Megaloblastic anemia often has bigger cells.
Blood smears can also show important signs, like hypersegmented neutrophils. Testing vitamin B12 and folate levels helps find the cause of megaloblastic anemia. This helps doctors treat it right.
In short, knowing how to spot megaloblastic anemia is vital. Doctors use lab tests and careful checks to find the right treatment. This makes sure patients get the care they need.
Treatment Options for Megaloblastic Anemia
Managing megaloblastic anemia needs a full plan. This includes supplements and changes in diet. The main goal is to fix the root cause of the problem.
Vitamin B12 Supplementation
For those with vitamin B12 deficiency, vitamin B12 supplementation is key. This can be given as injections or pills, based on the deficiency’s severity and how well the body absorbs it.
At first, patients often get injections often. As they get better, the injections might stop. Some people might need to take supplements for life, like those with pernicious anemia.
Folic Acid Therapy
Folic acid therapy is also vital, mainly for folate deficiency. Folic acid pills are taken by mouth, and the dose is higher than what’s in food.
It’s important to find out why someone has megaloblastic anemia. Taking folic acid can hide a vitamin B12 problem. This could lead to serious nerve issues if not treated.
Dietary Modifications
Dietary modifications are also key. Patients should eat foods rich in vitamin B12 and folate. Good sources include leafy greens, beans, nuts, and animal products.
For those who can’t eat certain foods, like vegans, there are fortified foods or supplements. These help meet nutritional needs.
| Treatment Approach | Description | Benefits |
| Vitamin B12 Supplementation | Injections or oral supplements to address deficiency | Rapid improvement in anemia symptoms |
| Folic Acid Therapy | Oral supplements to correct folate deficiency | Effective in treating megaloblastic anemia caused by folate deficiency |
| Dietary Modifications | Balanced diet rich in vitamin B12 and folate | Long-term management and prevention of recurrence |
Managing Pernicious Anemia Long-Term
Managing pernicious anemia long-term needs a full plan. This includes regular vitamin B12 shots and watching the patient closely. This condition stops the body from getting vitamin B12 because it can’t make intrinsic factor. So, lifelong care is needed to avoid problems and improve life quality.
Vitamin B12 Injection Protocols
Vitamin B12 shots are key for managing pernicious anemia. Patients usually start with shots often, then get them every 1-3 months later. How often they need shots can change based on how they do and what they need.
Key considerations for vitamin B12 injection protocols include:
- Initial dosing frequency: Often weekly or every other week for the first few months.
- Maintenance frequency: Typically every 1-3 months, adjusted based on patient response.
- Injection site rotation: To prevent discomfort and tissue damage.
Oral Supplementation Options
Some patients might use oral vitamin B12 instead of shots. High doses of oral vitamin B12 can work well, but it’s not for everyone. It’s important to watch how well it’s working and adjust as needed.
Oral supplementation considerations:
- High doses are required due to the limited absorption.
- Regular monitoring of vitamin B12 levels is critical.
- Patient compliance is essential for effectiveness.
Monitoring and Follow-up Care
Keeping an eye on the patient and adjusting treatment is vital. This means regular blood tests to check vitamin B12 and anemia levels. It also means watching for any signs of nerve problems.
Key aspects of monitoring and follow-up care:
- Regular blood tests to monitor vitamin B12 levels and anemia status.
- Assessment for neurological symptoms and complications.
- Adjustment of treatment protocols as necessary based on test results and patient symptoms.
By using vitamin B12 shots or pills and keeping a close eye on the patient, people with pernicious anemia can live well. This helps avoid serious problems in the long run.
Complications of Untreated Megaloblastic Anemia
If left untreated, megaloblastic anemia can cause serious health problems. It affects red blood cell production and overall health.
Neurological Complications
Untreated megaloblastic anemia can lead to serious neurological issues. Vitamin B12 deficiency is a common cause. It can cause neuropathy, leading to numbness, tingling, and pain in hands and feet.
It can also cause demyelination. This damages the myelin sheath around nerve fibers. It affects coordination, balance, and thinking.
Cardiovascular Complications
Megaloblastic anemia can also harm the heart if not treated. It can raise homocysteine levels. This increases the risk of heart attacks, strokes, and deep vein thrombosis.
The anemia can also put a strain on the heart. This can lead to heart failure in severe cases.
Psychological Effects
The mental health effects of untreated megaloblastic anemia are significant. Patients may feel depressed, anxious, and have cognitive impairment. This greatly affects their quality of life.
The fatigue and weakness can make people withdraw socially and decrease productivity. This worsens their mental health.
Increased Risk of Other Health Conditions
Untreated megaloblastic anemia can also raise the risk of other health issues. For example, osteoporosis may be more common due to nutritional deficiencies.
The causes of megaloblastic anemia, like malabsorption disorders, can lead to other nutrient deficiencies. This makes the situation even more complex.
Recent Advances in Megaloblastic Anemia Research
The field of megaloblastic anemia research has seen big steps forward. This is thanks to new tech and science. These changes are making a big difference in how we diagnose, treat, and care for patients.
One key area is genetic testing. New genetic sequencing tech lets us find specific genetic issues linked to megaloblastic anemia. This includes problems with vitamin B12 metabolism genes.
Genetic Testing Developments
Genetic testing has gotten better. Now, we can spot early signs of megaloblastic anemia. This means doctors can start treatments sooner.
Next-generation sequencing is helping us find rare genetic disorders. This leads to treatments that fit each patient’s needs.
Novel Treatment Modalities
New treatments for megaloblastic anemia are coming. There are novel vitamin B12 formulations and new ways to take them, like sublingual tablets and nasal sprays. These might work better for some people.
Research into gene therapy is also exciting. It could fix the root cause of megaloblastic anemia in some cases. This could lead to a cure.
Emerging Diagnostic Tools
New diagnostic tools are making it easier and faster to diagnose megaloblastic anemia. Things like advanced biomarkers and automated analyzers are helping patients get better sooner.
Point-of-care testing devices are being made. They can give quick diagnoses, which is great for places with limited healthcare or for patients who can’t get to a doctor easily.
Megaloblastic Anemia in Special Populations
Megaloblastic anemia is a big problem for pregnant women, kids, and older adults. It happens when red blood cells are too big. This can really affect these groups.
Megaloblastic Anemia in Pregnancy
Pregnancy makes women need more folate and vitamin B12. This is because the baby needs these nutrients to grow. If a woman doesn’t get enough, she might get megaloblastic anemia.
Key considerations for pregnant women:
- Increased folate requirements
- Risk of neural tube defects in the fetus if folate deficiency is not addressed
- Importance of prenatal vitamins that include folic acid and vitamin B12
| Risk Factor | Implication | Preventive Measure |
| Folate deficiency | Neural tube defects in the fetus | Folic acid supplementation |
| Vitamin B12 deficiency | Neurological issues in the mother | Vitamin B12 injections or oral supplements |
Pediatric Megaloblastic Anemia
Kids can get megaloblastic anemia from not eating enough, not absorbing nutrients, or genetic problems. This can slow down their growth and cause other problems if not treated right away.
Causes in children:
- Dietary deficiencies, like in vegan or vegetarian kids
- Malabsorption because of stomach problems
- Genetic conditions like transcobalamin II deficiency
Elderly Patients with Megaloblastic Anemia
Older people are more likely to get megaloblastic anemia. This is because they might not eat enough, can’t absorb nutrients well, or take medicines that mess with vitamins.
Management in the elderly:
- Regular screening for vitamin B12 deficiency
- Appropriate supplementation
- Monitoring for possible drug interactions
| Population | Common Causes | Management Strategies |
| Pregnant Women | Folate deficiency, increased demand | Folic acid supplementation, prenatal vitamins |
| Children | Dietary deficiencies, genetic disorders | Dietary adjustments, vitamin supplements |
| Elderly | Malabsorption, medication interactions | Vitamin B12 injections, monitoring medication |
Prevention Strategies for Megaloblastic Anemia
To stop megaloblastic anemia, we need to focus on diet, screening, and teaching patients. A good plan can lower the risk of getting this condition.
Dietary Recommendations
Eating foods rich in vitamin B12 and folate is key. Leafy greens, legumes, and animal products are good choices.
- Vitamin B12-rich foods: Meat, fish, poultry, eggs, and dairy products.
- Folate-rich foods: Dark leafy greens, beans, peas, and fortified cereals.
Vegetarians and vegans should eat fortified foods or take supplements to get enough vitamin B12.
Screening for High-Risk Individuals
Screening early is important for catching megaloblastic anemia in those at high risk. This includes:
- Pregnant women
- People with stomach problems
- Those on medicines that affect B12 or folate
| High-Risk Group | Recommended Screening |
| Pregnant Women | Complete Blood Count (CBC) and vitamin level testing |
| Individuals with Gastrointestinal Disorders | Vitamin B12 and folate level testing |
| Patients on Interfering Medications | Regular CBC and vitamin level monitoring |
Patient Education
Teaching patients about megaloblastic anemia is vital. This includes:
- Why a balanced diet matters
- Knowing the signs of anemia
- The need for regular check-ups
By teaching patients, we can prevent megaloblastic anemia and catch it early if it happens.
Living with Megaloblastic Anemia
Living with megaloblastic anemia means making big changes in your life. You’ll need to change your diet, find ways to deal with symptoms, and get support. These steps help manage symptoms and improve your life quality.
Lifestyle Adjustments
Making lifestyle adjustments is key for those with megaloblastic anemia. You’ll need to eat more foods rich in vitamin B12 and folate. Think leafy greens, citrus fruits, and fortified cereals. Also, avoid foods that make symptoms worse.
Adjusting your daily routine is also important. This helps manage fatigue, a common symptom. Pace yourself, take breaks, and get enough rest.
Coping with Symptoms
Dealing with symptoms of megaloblastic anemia is a big part of managing it. Fatigue is a big one, and it’s hard to fight. Try to prioritize tasks, stick to a sleep schedule, and do gentle exercises to fight fatigue.
Neurological symptoms like numbness or tingling can also happen. To manage these, you might need physical therapy, medication, or other treatments from your doctor.
Support Resources
Getting support resources is essential for those with megaloblastic anemia. Look for support groups, online or in-person, to share experiences and learn from others.
Healthcare providers are also key in supporting you. They offer regular check-ups, vitamin injections, and diet advice. These help a lot in managing the condition.
By making smart lifestyle changes, dealing with symptoms well, and using support resources, you can live a full and active life with megaloblastic anemia.
Conclusion
Megaloblastic anemia is a complex condition where red blood cells are abnormally large. It’s important to understand its causes, symptoms, diagnosis, and treatment to manage it effectively.
This article has highlighted the role of vitamin B12 and folate in megaloblastic anemia. Factors like dietary deficiencies, malabsorption disorders, and genetic factors play a part in it.
Diagnosing megaloblastic anemia involves blood tests and bone marrow exams. Treatment includes vitamin B12 supplements and folic acid therapy. These can help alleviate symptoms and prevent complications.
Knowing about megaloblastic anemia and its management can help prevent it. This summary gives a detailed look at the condition. It stresses the need for proper diagnosis and treatment.
FAQ
What is megaloblastic anemia?
Megaloblastic anemia is when your body makes big red blood cells that don’t work right. It’s often due to not enough vitamin B12 or folate.
What are the symptoms of megaloblastic anemia?
You might feel tired, weak, and have nerve problems. You could also have stomach issues.
What causes megaloblastic anemia?
It’s usually because you don’t get enough vitamin B12 or folate. This can happen if you don’t eat right, have trouble absorbing nutrients, or have a genetic issue.
How is megaloblastic anemia diagnosed?
Doctors use blood tests and look at your bone marrow. They also check for pernicious anemia with vitamin tests.
What is pernicious anemia?
Pernicious anemia is a common type of megaloblastic anemia. It’s caused by your body attacking itself and not making enough intrinsic factor.
How is pernicious anemia treated?
Treatment is vitamin B12 shots or pills. You’ll also need regular check-ups to make sure it’s working.
Can megaloblastic anemia be prevented?
Yes, you can prevent it by eating right and getting tested if you’re at risk. Learning about it helps too.
What are the complications of untreated megaloblastic anemia?
If you don’t treat it, you could have nerve damage, heart problems, and feel really down. It can also make you more likely to get other diseases.
How is megaloblastic anemia managed in special populations?
Pregnant women, kids, and older adults need special care. Their treatment plans are different because of their age or health status.
What lifestyle adjustments can help manage megaloblastic anemia?
Eating better, managing symptoms, and getting support can help. These changes can make your life better.
What are the recent advances in megaloblastic anemia research?
New research includes better genetic tests, new treatments, and tools for diagnosing the condition.
What is the difference between megaloblastic anemia and macrocytic anemia?
Both have big red blood cells. But megaloblastic anemia has specific cells in the bone marrow that are not normal.
Can folic acid therapy treat megaloblastic anemia?
Folic acid can help if you’re not getting enough folate. But it won’t fix a vitamin B12 problem.
Reference
- Carmel, R. (2008). Pernicious anemia: The expected findings of very low cobalamin levels, anemia, and macrocytosis are often lacking. Archives of Internal Medicine, 168(20), 2220“2227. https://pubmed.ncbi.nlm.nih.gov/19001197