Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
The consultation is the foundational step in the journey toward aesthetic neck contouring. It is a detailed process where the surgeon evaluates the patient’s unique anatomy to determine the underlying causes of their aesthetic concerns. This is not a one-size-fits-all assessment; it requires a tactile and visual analysis of the neck’s layers.
The surgeon will assess the skin quality, checking for elasticity, sun damage, and thickness. They will palpate the neck to distinguish between subcutaneous fat (above the muscle) and subplatysmal fat (below the muscle). The position of the hyoid bone and the size of the submandibular glands are also evaluated to set realistic expectations.
During this session, the patient’s goals are discussed in depth. The surgeon uses a mirror to simulate potential results, pulling the skin back to show what a lift might achieve compared with what liposuction alone might do. This visual communication helps align the patient’s expectations with surgical possibilities.

A thorough medical history is critical for patient safety. The surgeon reviews all current medical conditions, previous surgeries, and medications. Specific attention is paid to conditions that affect wound healing, such as diabetes, autoimmune disorders, or connective tissue diseases.
Hypertension (high blood pressure) is a significant risk factor in neck surgery, as it can lead to hematomas (blood collections) postoperatively. The surgeon will ensure that blood pressure is well controlled before proceeding. Smoking history is also a significant factor, as nicotine compromises blood flow and skin survival.
Patients are asked about their use of supplements and over-the-counter medications. Many common supplements, such as fish oil, Vitamin E, and ginkgo biloba, act as blood thinners and must be discontinued weeks before surgery to minimize bleeding and bruising.

One of the most critical aspects of the preparation phase is managing expectations. The surgeon explains the limitations imposed by the patient’s anatomy. For example, a patient with a low hyoid bone may never achieve a harsh 90-degree neck angle, regardless of the technique used.
The discussion includes a frank conversation about scarring. While incisions are placed strategically to be hidden, they are permanent. The surgeon explains where the scars will be located typically behind the ears and under the chin and how they mature over time.
The concept of facial harmony is reinforced. A neck that is too tight on an aging face can look unnatural. The surgeon may suggest adjunctive procedures, such as a facelift or chin implant, to ensure the neck contour balances with the rest of the features.
Depending on the patient’s age and health status, preoperative testing may be required. This typically includes blood work to check for anemia and clotting ability. An electrocardiogram (EKG) may be needed for patients over a certain age to ensure heart health.
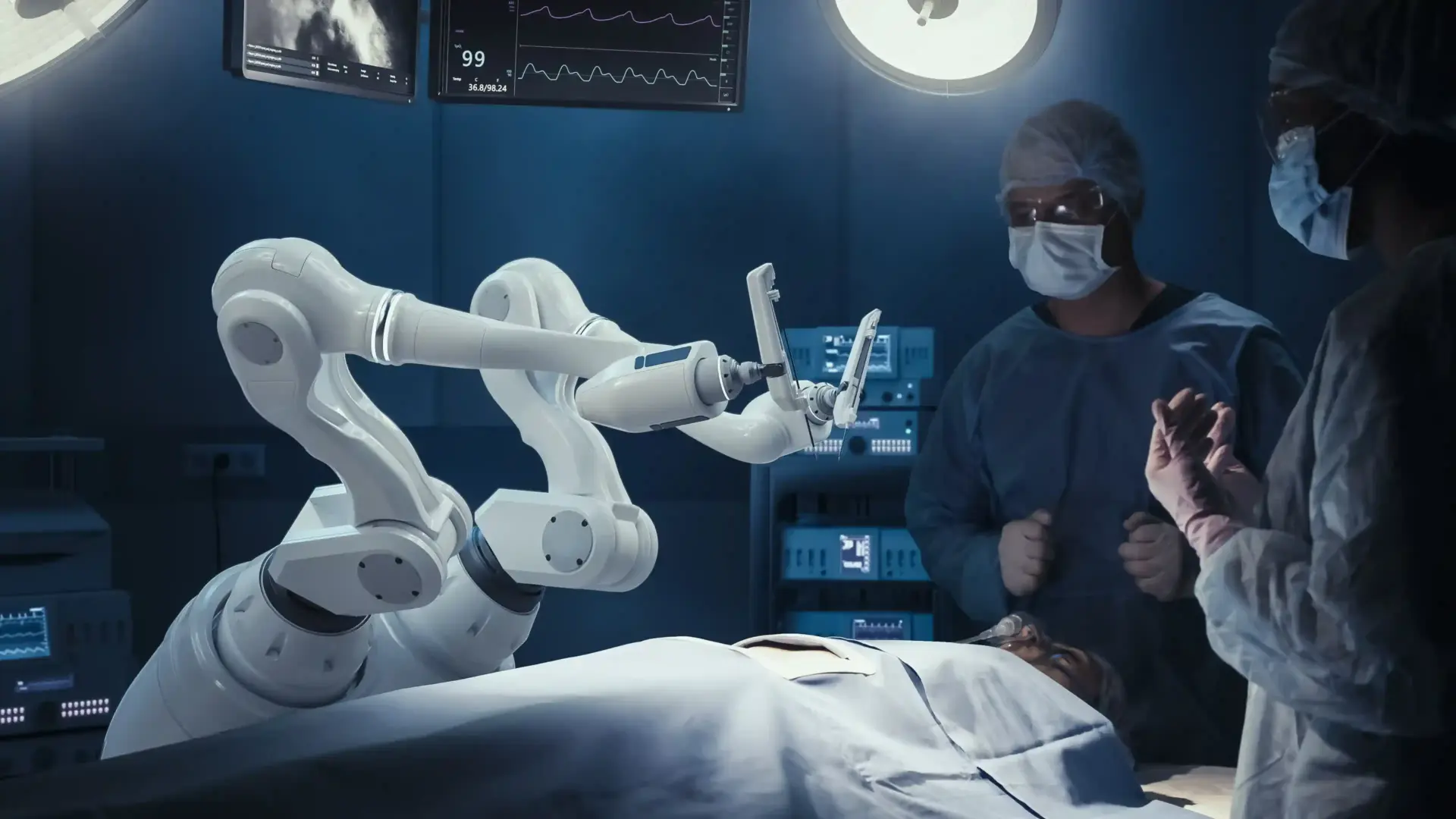
Medical clearance from the patient’s primary care physician is often requested to confirm the patient’s fitness for anesthesia. This collaborative approach ensures that all medical bases are covered before the patient enters the operating room.
Preparation involves specific lifestyle changes to optimize results. Patients are advised to maintain a stable weight before surgery. Significant weight fluctuations after surgery can compromise the aesthetic outcome.
A skincare regimen may be prescribed to prepare the skin. Retinoids or antioxidants can improve skin quality and vascularity leading up to the procedure. Sun protection is emphasized to reduce inflammation and damage to the skin cells.
For smokers, a strict cessation protocol is enforced. Nicotine causes vasoconstriction, which can lead to skin flap necrosis (skin death) and poor wound healing. Patients are typically required to stop all nicotine products for at least four to six weeks before and after surgery.
This is a non-negotiable safety requirement for most surgeons. Urine tests for nicotine metabolites may be performed to ensure compliance. The goal is to maximize oxygen delivery to the healing tissues.
A successful recovery requires planning. Patients are instructed to arrange for a responsible adult to drive them home and stay with them for the first 24 to 48 hours.
The home environment should be prepared with necessary supplies: ice packs, gauze, prescribed medications, and comfortable pillows to keep the head elevated. Planning time off work and social activities is essential to ensure adequate rest without stress.
Patients receive specific instructions on how to manage their medications. Blood thinners must be stopped under the guidance of the prescribing doctor.
A regimen of preoperative medications might include antibiotics to prevent infection or medications to minimize bruising (like Arnica Montana). Patients are given a list of prohibited substances to avoid accidental ingestion of blood thinners.
Instructions for the day before surgery are precise. Patients are typically asked to wash with an antimicrobial soap to reduce bacteria on the skin. Fasting instructions (NPO – nothing by mouth) are provided to ensure an empty stomach for anesthesia safety.
Clothing choices are discussed; patients should wear loose-fitting shirts that button in the front to avoid pulling clothing over the head and disturbing the fresh incisions.
Finally, the surgeon assesses the patient’s psychological readiness. Surgery is a physical and emotional journey. Patients should have a stable support system and a positive mindset.
Understanding the “emotional rollercoaster” of recovery—where swelling and bruising can temporarily affect mood—is helpful. Being mentally prepared for the downtime helps patients navigate the healing process with resilience.

Send us all your questions or requests, and our expert team will assist you.
Ask about their board certification, how many neck contouring procedures they perform annually, and to see before-and-after photos of patients with similar anatomy to yours. Ask about their specific plan for your deep fat and muscle, not just the skin.
No, you do not need to cut your hair. In fact, having longer hair can be beneficial as it can hide the incisions around the ears while they heal. The surgical team will band your hair back to keep it out of the surgical field.
No, you must arrive with a clean face, free of makeup, lotions, or creams. This reduces the risk of infection. You should also remove all jewelry and contact lenses.
This depends on the surgeon’s schedule, but typically you should plan 1 to 3 months. This gives you ample time to complete medical clearance, stop medications, and arrange your recovery logistics.
If you develop a cold, flu, or any infection in the week leading up to surgery, you must notify the office immediately. Elective surgery requires you to be in optimal health. It is safer to reschedule than to undergo anesthesia with an active illness.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)