Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
The surgical journey begins with precise preoperative marking. This is an art form in FDL surgery. The surgeon marks the patient while standing to gauge the full extent of the tissue laxity. The vertical wedge is drawn first, estimating the amount of central tissue to be excised to narrow the waist.
Then, the horizontal incision is marked low on the pubis, extending laterally towards the hips. The surgeon ensures that the vertical and horizontal markings intersect correctly to prevent “dog ears” (excess skin bunches) at the ends of the incisions. The future position of the umbilicus is also carefully planned.

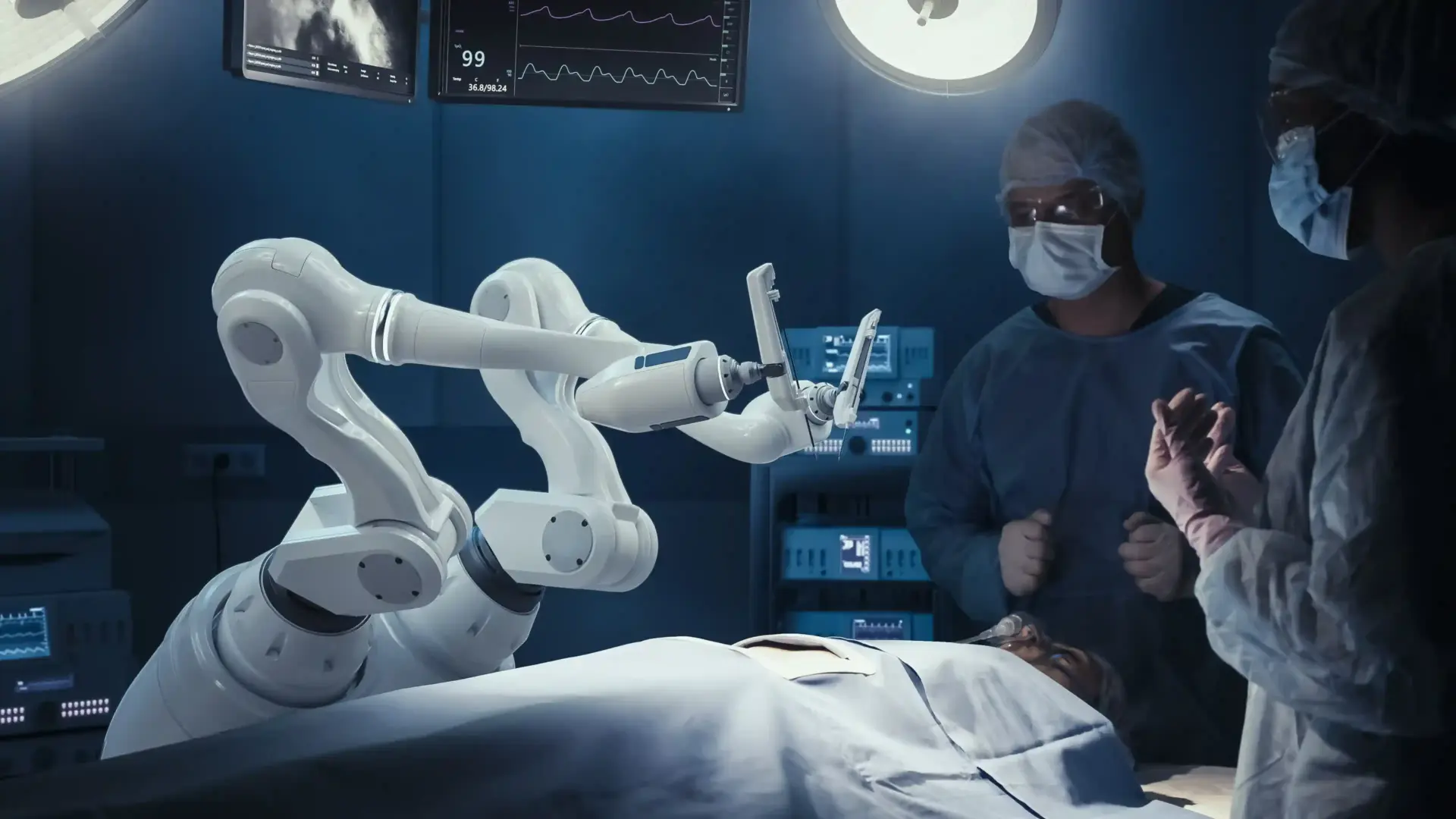
The surgery is performed under general anesthesia. The anesthesia team utilizes advanced protocols to maintain hemodynamic stability and prevent deep vein thrombosis (DVT). Sequential compression devices are placed on the legs, and the patient is kept warm to optimize clotting.
Safety is paramount during this extended procedure. The surgeon uses tumescent fluid containing epinephrine to infiltrate the surgical sites. This constricts blood vessels, significantly reducing blood loss and keeping the surgical field clear for precise dissection.

The incision is made, and the skin flaps are elevated. Surgeons often employ a technique that preserves Scarpa’s fascia, a deep layer of connective tissue in the lower abdomen. Preserving this layer protects the lymphatic drainage vessels, reducing the risk of later fluid accumulation (seroma).
The dissection is carried up to the xiphoid process to expose the entire length of the rectus muscles. The surgeon carefully cauterizes small blood vessels as they go, maintaining a dry field. This meticulous dissection is critical for the health of the large skin flaps being created.
With the muscles exposed, the repair of the diastasis recti begins. The surgeon uses heavy, permanent sutures to stitch the left and right rectus muscles together. This plication starts at the xiphoid and runs all the way down to the pubis.
In an FDL, this repair is often aggressive, as the vertical skin removal allows for significant tightening without bunching the skin. This step flattens the abdominal wall and creates the internal tension required for a stable core. It is the structural backbone of the surgery.
After the muscle repair, the patient is placed in a flexed position (beach chair) to relieve tension. The surgeon then excises the vertical skin wedge first, pulling the flanks inward to define the waist. Then, the horizontal excess is removed, pulling the upper abdomen downward.
The closure is the most technically demanding part. The surgeon uses a layered suturing technique to distribute tension deep into the tissues, relieving pressure on the skin edges. Special care is taken at the T junction where the incisions meet to ensure adequate blood flow.
A new opening is created in the draped skin for the belly button. The umbilicus is brought through and sutured into place. Surgeons use specific techniques to create a natural, hooded appearance, avoiding a circular, operated look.
The stalk of the umbilicus may be shortened to pull it flush against the abdominal wall. The scarring is hidden inside the navel depression. This level of detail is essential for a natural-looking result.
Many surgeons use drains to remove fluid that accumulates beneath large flaps. These tubes are placed through small incisions and stay in for a week or more. However, some surgeons use “drainless” techniques involving progressive tension sutures.
These quilting sutures secure the skin flap to the muscle, closing the dead space where fluid would otherwise collect. While this takes longer in surgery, it can make recovery easier for the patient by eliminating the need to manage drains. The choice depends on the surgeon’s preference and the extent of the dissection.
The first few days after surgery are the most difficult. Patients will feel tight and sore, particularly from the muscle repair. Walking will be done in a hunched-over position to protect the incisions.
Pain is managed with a multimodal approach, including muscle relaxants, nerve blocks (such as Exparel), and oral pain medication. Early ambulation is encouraged to prevent blood clots. Patients typically stay in the hospital for one night or go to a recovery center for monitoring.
Swelling can persist for months. Patients wear a compression binder for 6 to 8 weeks to support the tissues and control edema. Heavy lifting and strenuous exercise are restricted for 6 to 8 weeks to allow the muscle repair to heal securely.
The vertical scar will be initially red and raised. It takes 12 to 18 months for the scars to mature and fade fully. Patients are educated on patience, as the final contour and scar quality are not visible for a year.
Send us all your questions or requests, and our expert team will assist you.
The muscle repair causes the most discomfort, feeling like a very intense abdominal workout. The skin incisions themselves are numb. We use long-acting local anesthesia and muscle relaxants to keep the pain manageable. Most patients switch to Tylenol within a week.
If you have drains, you will likely be instructed to sponge bath until they are removed. Once cleared to shower, you can use a lanyard to hold the drains around your neck so they don’t pull on your neck.
You will walk hunched over for the first week or two to keep tension off the incision. As the skin relaxes and heals, you will gradually be able to stand straighter. Please do not force it; let your body dictate the pace.
The T junction is the spot where the vertical and horizontal scars meet. It is the slowest-healing area because the blood supply is lowest there. We monitor it closely. Sometimes a small scab forms there, which usually heals with simple wound care.
Yes, the skin of the lower abdomen will be numb after surgery because the sensory nerves are cut during the skin lift. Sensation often returns slowly over the next year as nerves regrow, but some numbness may be permanent.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)