Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
The initial consultation is a critical diagnostic session where the surgeon evaluates the nature of the defect and the biological quality of the remaining tissue. It begins with a thorough examination of the lip structure, including the vermilion border, the mucosa, and the surrounding cheek tissue. The surgeon assesses the cause of the defect whether it is an acute injury, a tumor, or a scar as this dictates the reconstructive approach.
During this phase, the surgeon performs a functional assessment. The patient is asked to smile, pucker, and speak to evaluate the integrity of the orbicularis oris muscle and the facial nerve. This dynamic evaluation helps identify any underlying weakness or paralysis that must be addressed during the reconstruction.

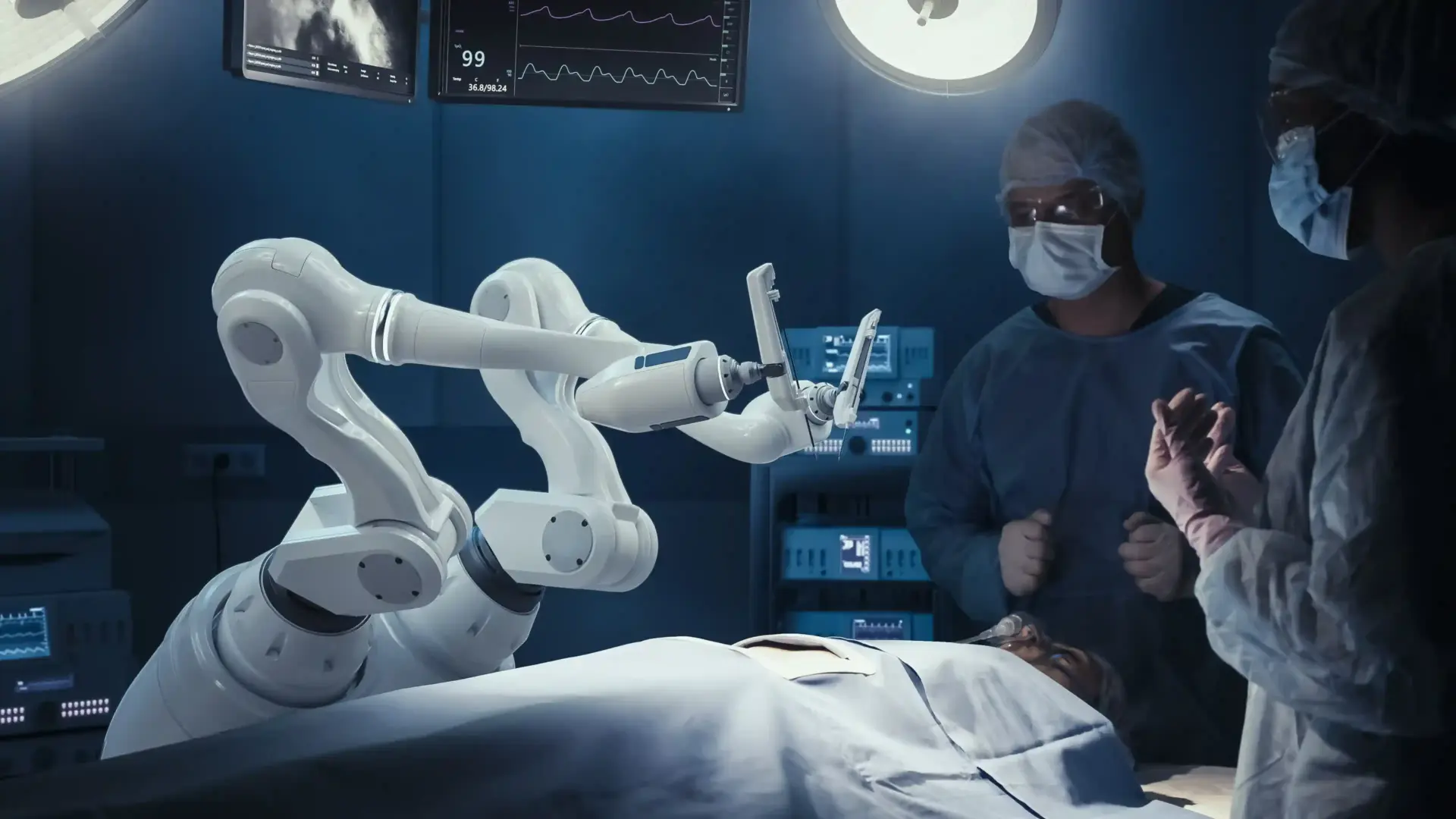
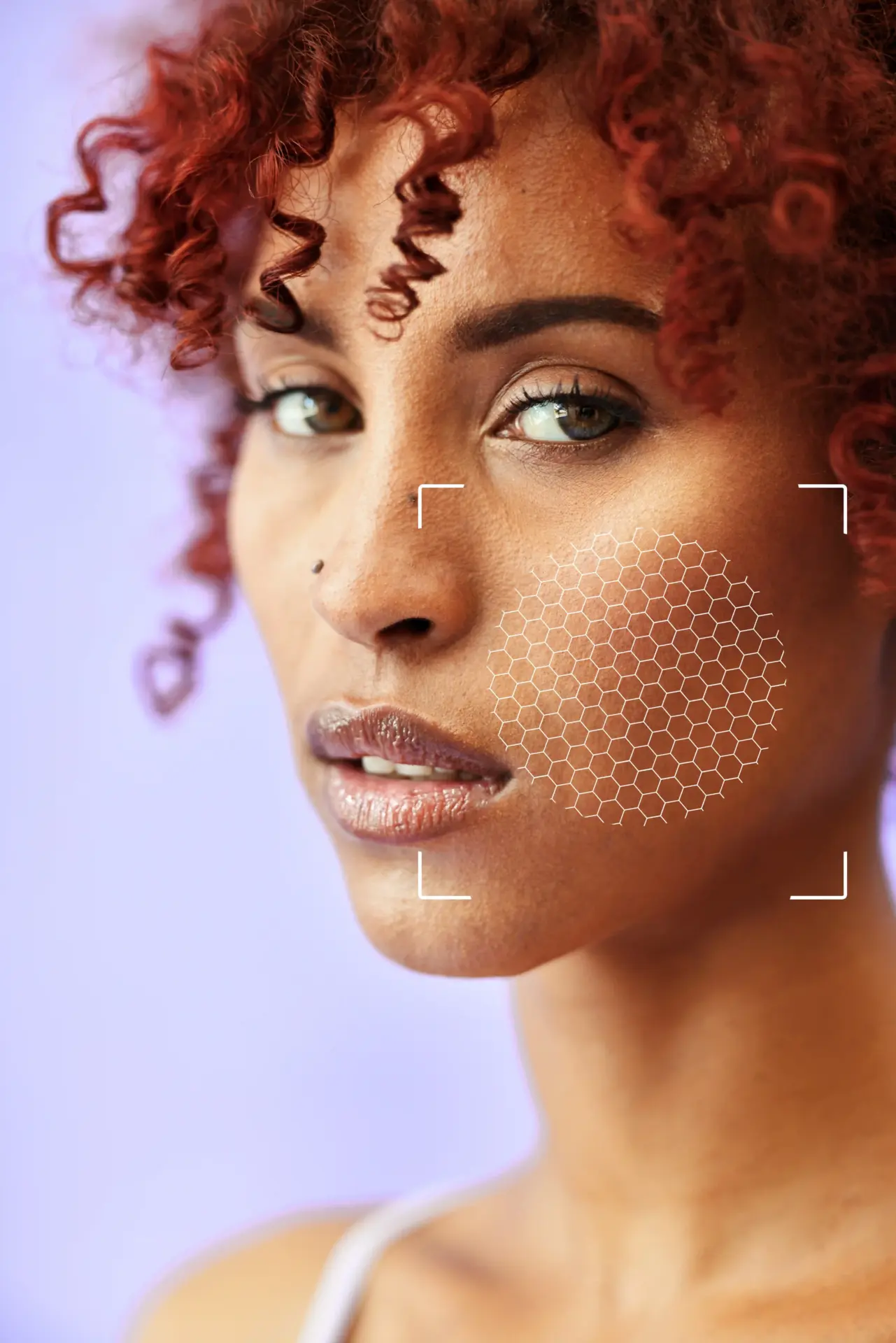
For complex defects or planned resections, modern technology plays a vital role. 3D imaging systems capture high-resolution topographic maps of the face. This allows the surgeon to measure the defect area precisely and plan the geometry of the flaps needed to cover it.
Digital mapping is beneficial for planning symmetry. The surgeon can mirror the healthy side of the lip onto the defective side in the 3D model to calculate the exact amount of tissue required for restoration. This data-driven approach minimizes the risk of asymmetry and ensures precise flap design.

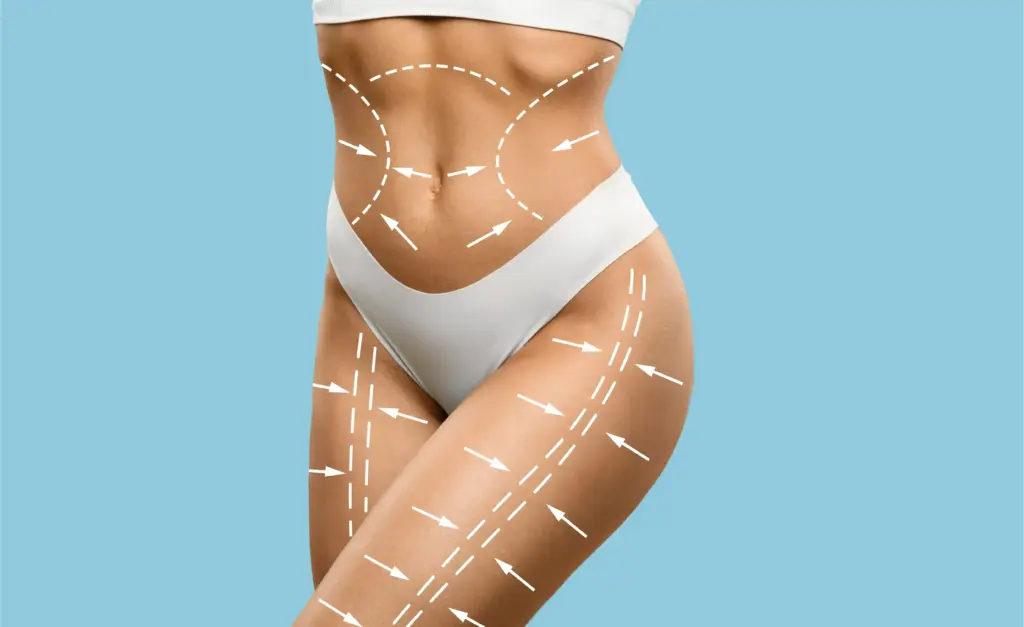
The success of local flaps depends on the laxity of the surrounding skin. The surgeon performs manual tests, pinching and moving the skin of the cheeks and chin to gauge how much it can stretch. This is known as the “pinch test.”
Patients with loose, elastic skin (often older patients) may be candidates for larger local flaps without causing distortion. Younger patients with tight skin may require more complex designs to recruit tissue without pulling the mouth open or distorting the nose. This biomechanical assessment determines the feasibility of the chosen technique.
Blood supply is the lifeline of any reconstruction. For flaps like the Abbe or Estlander, which rely on the labial artery, ensuring the labial artery remains intact is mandatory. The surgeon may use a handheld Doppler probe to detect the arterial pulse in the lip audibly.
This mapping marks the exact location of the vessel on the skin, allowing the surgeon to safely design the flap around this pivot point. It confirms that the donor tissue has a robust blood supply, which is critical for preventing tissue death (necrosis) after the transfer.
The mouth is a bacteria-rich environment. To reduce the risk of infection, oral hygiene must be optimized before surgery. Patients are examined for active dental infections, gum disease, or severe plaque buildup.
The surgeon may require a professional dental cleaning before the procedure. Patients are instructed to start an antiseptic mouthwash regimen (such as chlorhexidine) in the days leading up to surgery. A clean oral cavity is essential for the healing of mucosal incisions.
Nicotine is a potent vasoconstrictor that jeopardizes the survival of reconstructive flaps. It shrinks the tiny blood vessels that feed the healing tissue. In lip reconstruction, where tissue is rotated and stretched, adequate blood flow is non-negotiable. Smoking significantly increases the risk of flap loss, wound breakdown, and scarring.
A strict cessation protocol is enforced. Patients must stop all nicotine products vapes, patches, gum, and smoke for at least 4 to 6 weeks before and after surgery. Urine cotinine tests are frequently used to verify compliance and ensure the safety of the reconstruction.
Send us all your questions or requests, and our expert team will assist you.

Healing requires building blocks. A nutritional assessment ensures the patient has adequate protein and vitamin stores to support tissue regeneration. This is especially important for cancer patients or elderly patients who may have nutritional deficits.
Surgeons may check albumin and prealbumin levels. Patients are encouraged to consume a high-protein diet and may be prescribed supplements like Zinc and Vitamin C to boost collagen synthesis and immune function before surgery.
Lip surgery affects the face’s most communicative feature. The recovery period can include swelling, difficulty speaking clearly, and temporary deformity. The surgeon assesses the patient’s psychological resilience and support system.
Patients need to be mentally prepared for the “ugly duckling” phase of healing. Understanding that the immediate post-op appearance is not the final result is crucial. Support from family is vital, especially if the patient will be on a liquid diet or have difficulty speaking for a few weeks.
If the lip defect involves nerve damage, a detailed neurological exam is performed. The surgeon tests the strength of the lip muscles by asking the patient to whistle or blow air. This helps map out which branches of the facial nerve are functioning.
This evaluation determines if nerve grafts or muscle transfers will be needed. It establishes a functional baseline to measure recovery against. Understanding the extent of paralysis helps the surgeon plan dynamic versus static reconstruction.
Lip surgery often involves instruments working near the teeth. The surgeon assesses the patient’s dentition to identify loose teeth or crowns that might be at risk during intubation or surgery.
Protective measures, such as dental guards, are planned. For patients with dentures, instructions are given regarding when they can be worn post-surgery to avoid pressure on the healing lip.
Recovery from lip reconstruction often requires dietary modifications. Patients are advised to purchase a blender and stock up on nutritional shakes, soups, and soft foods.
Logistics also involve communication. Patients may need a whiteboard or text-to-speech app if their speech will be restricted. Planning time off work and arranging for transportation is essential, as the patient may be on pain medication or feel self-conscious appearing in public initially.
To minimize infection, the skin around the mouth is prepped. Patients may be instructed to wash their faces with an antibacterial soap (such as Hibiclens) the night before and the morning of surgery.
Men are usually asked to shave their facial hair closely to allow for sterile surgical prep and secure dressing application. The goal is to create the most sterile field possible in an area that is naturally colonized by bacteria.
If you have gum disease, cavities, or loose teeth, yes. Bacteria from your mouth can infect the lip surgery site. We often recommend a professional cleaning a week or two before the operation to ensure your mouth is as clean as possible.
You can eat normally in the weeks leading up to surgery. However, you must stop eating and drinking (fasting) starting at midnight the night before surgery to prevent complications with anesthesia.
You must stop smoking and using all nicotine products for at least 4 weeks before surgery and 4 weeks after. Nicotine kills the blood supply to the flaps we use to fix your lip. If you smoke, the reconstruction is very likely to fail and turn black.
Yes, standard pre-operative blood work is required to check your blood count (for anemia) and your clotting ability. We need to make sure you are healthy enough for anesthesia and that your blood clots normally.
If you feel a cold sore coming on, call us immediately. We will prescribe an antiviral medication. If you have an active blister on the day of surgery, we will likely have to reschedule to prevent the virus from spreading into the surgical wound.



Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)