Last Updated on October 21, 2025 by mcelik

Did you know that polycythemia vera, a rare blood disorder, can lead to an overproduction of red blood cells? This can cause serious complications if not treated. We’re here to help you understand this condition.
Polycythemia vera means your body makes too many red blood cells. This can make your blood thick and increase your risk of blood clots. The early signs can be hard to spot because they’re not very specific.
It’s important to know the early signs of polycythemia vera. We’ll look at the first symptoms and what they mean.
Key Takeaways
- Polycythemia vera is a rare blood disorder that leads to an overproduction of red blood cells.
- Early symptoms can be nonspecific and challenging to diagnose.
- Understanding the initial signs is key for timely medical help.
- Untreated polycythemia vera can lead to serious complications, including blood clots.
- Spotting the condition early can greatly improve patient outcomes.
Understanding Polycythemia Vera

Polycythemia vera is a complex condition that affects many people. It’s a type of myeloproliferative neoplasm. This means it causes too many red blood cells, white blood cells, and platelets. If not treated, it can cause serious health problems.
Definition and Classification
Polycythemia vera (PV) is a blood cancer. It’s part of the myeloproliferative neoplasms (MPN) group. These diseases make the bone marrow produce too many blood cells. PV leads to too many red blood cells, which can harm the heart and blood vessels.
The World Health Organization (WHO) has clear guidelines for diagnosing PV. They look at both clinical signs and genetic markers. A diagnosis is made if certain genetic changes, like the JAK2 V617F mutation, and high blood counts are present.
“The diagnosis of polycythemia vera requires a thorough check of both clinical and molecular signs.” -World Health Organization
Prevalence and Demographics
Polycythemia vera is rare, with about 0.4 to 2.8 cases per 100,000 people each year. It mostly affects people over 60. The average age at diagnosis is 60. Men are slightly more likely to get PV than women.
| Age Group | Incidence Rate (per 100,000) |
| 40-59 | 0.8-1.4 |
| 60-79 | 2.4-4.8 |
| 80+ | 4.8-6.2 |
Knowing who gets polycythemia vera helps doctors catch it early. It’s key for healthcare providers to know the signs and risk factors. This way, they can give the best care possible.
The Pathophysiology of Polycythemia
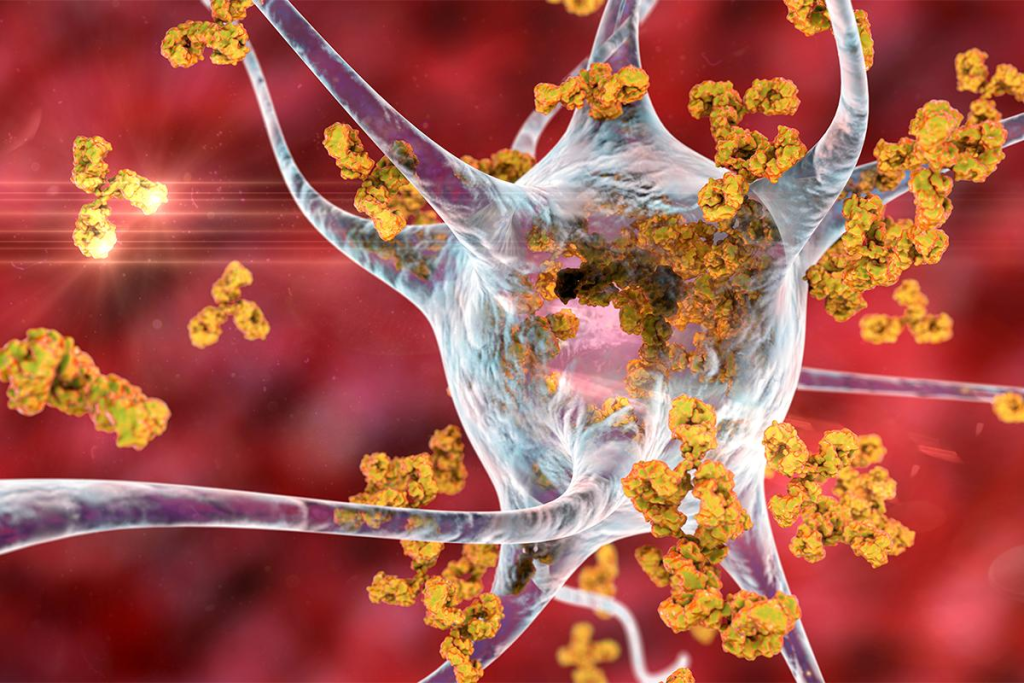
In polycythemia vera, the body makes too many red blood cells. This happens because the normal control over blood cell production is broken.
Blood Cell Production Under Normal Conditions
The body makes red, white blood cells, and platelets in a balanced way. This balance is key to staying healthy.
Many factors control how blood cells are made. For example, a hormone called erythropoietin helps make red blood cells. The body adjusts how many cells it makes based on oxygen levels.
Disruption in Polycythemia Vera
In polycythemia vera, a genetic problem disrupts this balance. This problem, often in the JAK2 gene, causes too many red blood cells.
Having too many red blood cells makes blood thicker and more sticky. This can lead to serious problems. Knowing how this happens helps doctors treat it better.
| Aspect | Normal Condition | Polycythemia Vera |
| Blood Cell Production Regulation | Tightly regulated by hormones and growth factors | Disrupted due to genetic mutations |
| Red Blood Cell Count | Within normal range | Elevated, leading to erythrocytosis |
| Blood Viscosity | Normal | Increased due to excess red blood cells |
Understanding polycythemia vera’s cause is key to knowing its symptoms and risks. It guides how doctors treat it. They aim to prevent problems caused by thick blood and too many red blood cells.
Early Warning Signs of Polycythemia Vera
Spotting polycythemia vera early is key. We’ll look at the first signs that might show this condition. We’ll also talk about when you should worry about your health.
Subtle Initial Symptoms
The first signs of polycythemia vera are often hard to spot. Common signs include headaches, dizziness, and feeling very tired. These happen because the blood gets thicker, making it harder for it to flow.
Headaches and dizziness are common early signs. Thicker blood can cut down on blood flow to the brain, causing these issues. Feeling very tired is another sign, as the body works harder to move the thicker blood.
When to Be Concerned
If you keep getting headaches, dizziness, or feeling very tired, see a doctor. These symptoms don’t always mean you have polycythemia vera. But, they’re signs that you should get checked out.
| Early Warning Sign | Possible Cause |
| Headaches | Increased blood viscosity reducing blood flow to the brain |
| Dizziness | Impaired blood circulation |
| Fatigue | Increased effort to circulate thicker blood |
Thick Blood Symptoms: The Hallmark of Polycythemia
Polycythemia vera makes blood thick, which can cause problems if not treated. This condition has more red blood cells, making blood thicker and stickier.
Understanding Blood Viscosity
Blood viscosity is how thick and sticky blood is. In polycythemia vera, more red blood cells make blood thicker and stickier. This can slow down blood flow and lead to serious health problems.
Normal blood viscosity is key for good circulation. If blood gets too thick, it can’t flow well to important organs. This raises the risk of blood clots and heart problems.
How Thick Blood Affects the Body
Thick blood can affect the body in many ways. It can:
- Make blood flow poorly to hands and feet, causing them to feel cold
- Make blood clots more likely, leading to heart attacks, strokes, or deep vein thrombosis
- Damage kidneys by reducing blood flow
- Put extra strain on the heart, which could lead to heart failure
Recognizing Blood Thickness Symptoms
It’s important to know the signs of thick blood for early treatment. Common symptoms include:
| Symptom | Description |
| Headaches | Frequent or severe headaches due to reduced blood flow |
| Dizziness | Feeling dizzy or lightheaded, potentially leading to falls |
| Vision Changes | Blurred vision, double vision, or loss of vision due to reduced blood flow to the eyes |
If you notice these symptoms, see a doctor right away. They can help figure out what’s wrong and how to treat it.
Circulatory Symptoms: The First Red Flags
Circulatory symptoms often signal the start of polycythemia vera. This condition makes red blood cells multiply too much. The blood gets thicker and more difficult to flow, causing various circulatory problems.
Headaches and Dizziness
Headaches and dizziness are common signs of polycythemia vera. These happen because the blood’s thickness hinders its flow to the brain.
People with this condition often face persistent headaches. These headaches can really disrupt their daily lives.
Vision Changes
Vision changes are another key symptom of polycythemia vera. The thick blood can cut off blood flow to the eyes. This might cause blurred vision, double vision, or even temporary blindness.
It’s very important for those with these symptoms to see a doctor. These signs can point to a serious condition.
Tinnitus (Ringing in the Ears)
Tinnitus, or ringing in the ears, is a less common but important symptom. The blood’s thickness and reduced flow can harm the inner ear. This leads to the annoying condition of tinnitus.
The table below lists the main circulatory symptoms of polycythemia vera:
| Symptom | Description | Possible Cause |
| Headaches | Persistent and often severe headaches | Increased blood viscosity impairing brain blood flow |
| Dizziness | Feeling of lightheadedness or unsteadiness | Reduced blood flow to the brain |
| Vision Changes | Blurred vision, double vision, or temporary blindness | Reduced blood flow to the eyes |
| Tinnitus | Ringing or other sounds in the ears | Affected blood flow to the inner ear |
Skin Manifestations of Polycythemia Vera
The skin can show signs of health issues in people with polycythemia vera. It displays symptoms that help in diagnosing and managing the condition.
Facial Redness and Plethora
Facial redness, or plethora, is a key sign of polycythemia vera. It happens because of more red blood cells, making the skin look reddish. People might also feel warm or flushed.
Itching (Pruritus)
Itching, or pruritus, is common in those with polycythemia vera. It can be all over or in one spot. It gets worse when exposed to warm water, like in a shower. The cause of itching is not clear, but it might be linked to histamine from abnormal blood cells.
Easy Bruising
Easy bruising is a big worry for those with polycythemia vera. The condition can mess with blood cell balance, affecting platelets. This leads to bruising and bleeding issues. It shows why managing the condition is so important to avoid these problems.
Cardiovascular Symptoms in Early Polycythemia Vera
Polycythemia vera is a condition where the body makes too many red blood cells. This can cause several heart-related symptoms. It’s important to know how these symptoms affect our health.
Hypertension
Hypertension, or high blood pressure, is a symptom of polycythemia vera. The thick blood puts extra pressure on the heart. Keeping an eye on blood pressure is key to avoiding heart problems.
Hypertension Management: Changing diet and exercise habits can help control blood pressure. Sometimes, medication is also needed.
Chest Pain
Chest pain is another symptom of early polycythemia vera. It happens because the heart has to work harder with thick blood. Knowing the different types of chest pain and their causes is important.
- Angina: Chest pain or discomfort caused by reduced blood flow to the heart.
- Other causes: Including but not limited to pericarditis or myocarditis.
Thrombotic Events
Thrombotic events, like deep vein thrombosis (DVT) and pulmonary embolism (PE), are serious. Thick blood can cause dangerous blood clots. These can be deadly if not treated quickly.
| Thrombotic Event | Description | Symptoms |
| Deep Vein Thrombosis (DVT) | A blood clot in a deep vein, typically in the legs. | Leg pain or swelling, warmth, redness. |
| Pulmonary Embolism (PE) | A blockage of an artery in the lungs by a blood clot. | Shortness of breath, chest pain, cough. |
It’s vital to understand these symptoms to catch polycythemia vera early. Regular check-ups and monitoring can help manage these risks.
Gastrointestinal Manifestations
Polycythemia vera can cause a variety of gastrointestinal symptoms. These include discomfort in the abdomen and issues with digestion. While it mainly affects blood cells, it can also impact digestion, affecting a person’s quality of life.
Abdominal Discomfort
Many people with polycythemia vera experience abdominal discomfort. This can range from mild bloating to severe pain. Splenomegaly, or an enlarged spleen, can cause this discomfort by pressing on the stomach and other organs.
Early Satiety
Feeling full quickly after eating is another symptom of polycythemia vera. This can be due to an enlarged spleen or other digestive changes. Early satiety can lead to reduced food intake, which can affect nutrition and health.
Unexplained Weight Loss
Unexplained weight loss is a concerning symptom for those with polycythemia vera. It can be caused by early satiety, changes in metabolism, and increased energy use. It’s important for those experiencing weight loss to see their doctor for evaluation and management.
Gastrointestinal symptoms can greatly affect the management and quality of life for those with polycythemia vera. Recognizing these symptoms early can help tailor treatment plans to address both blood and digestive issues.
Neurological Symptoms of Polycythemia Vera
Polycythemia vera causes too many red blood cells, leading to neurological problems. These include changes in thinking and a higher risk of stroke. It’s important to know how these symptoms affect patients and how to manage them.
Cognitive Changes
Cognitive changes are common in polycythemia vera. Symptoms include trouble focusing, memory problems, and feeling less clear-headed. It’s vital for patients to tell their doctors about these issues, as they can greatly affect daily life.
Studies link the thick blood in polycythemia vera to these thinking problems. Treating the condition can help improve these symptoms.
Paresthesia (Tingling and Numbness)
Paresthesia, or tingling and numbness, is another symptom. It can make daily tasks hard. This feeling can be uncomfortable and sometimes gets in the way of everyday activities.
The exact reason for paresthesia in polycythemia vera is not known. But it’s thought to be due to thick blood and possible nerve damage. Treating the condition can help lessen paresthesia.
Stroke Risk
Polycythemia vera also raises the risk of stroke. The high number of red blood cells makes blood thicker and more likely to clot. Stroke is a serious emergency that needs quick action.
Knowing the signs of stroke is key. These include sudden weakness, trouble speaking, or vision changes. Patients with polycythemia vera should be aware of these risks and work with their doctors to lower their stroke risk.
When to See a Doctor: Red Alerts
It’s important to know the red alerts for polycythemia vera. This helps you get medical help on time. Some symptoms need quick attention to avoid serious problems.
Urgent Symptoms Requiring Immediate Attention
If you have any of these symptoms, get medical help right away:
- Severe headache or dizziness, which could mean a stroke or serious brain problems.
- Chest pain or shortness of breath, which might show heart issues.
- Vision changes, like blurred or double vision, could be from blood issues affecting your eyes.
- Severe abdominal pain, which might mean an enlarged spleen or other stomach problems linked to polycythemia vera.
Symptoms That Warrant a Check-up
These symptoms are not life-threatening but should get you to see a doctor:
- Persistent itching, often after bathing, which is a common symptom of polycythemia vera.
- Unexplained weight loss or early satiety, possibly due to an enlarged spleen.
- Fatigue or weakness, which can really affect your daily life.
- Frequent bruising or bleeding, showing possible blood problems.
Preparing for Your Doctor’s Appointment
To get the most from your visit, prepare well:
- List your symptoms, including when they started and how often they happen.
- Note any medications you’re taking, including how much.
- Prepare questions for your doctor, like what might be causing your symptoms and the best treatments.
- Bring a friend or family member for support and to help remember the conversation.
Being informed and ready helps you and your healthcare team manage your polycythemia very well.
Distinguishing Polycythemia Vera from Secondary Polycythemia
It’s important to know the difference between Polycythemia Vera and Secondary Polycythemia. Both lead to more red blood cells, but they have different causes and treatments. This knowledge helps doctors give the right care to patients.
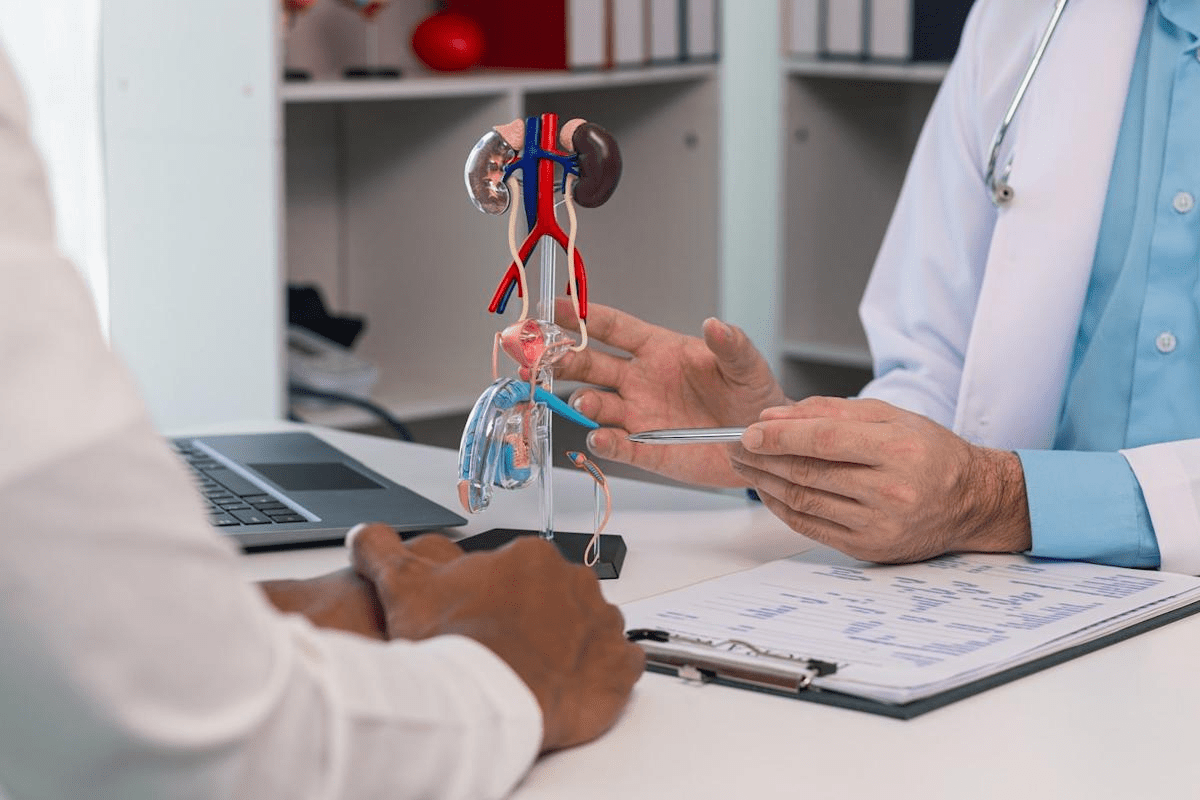
Causes of Secondary Polycythemia
Secondary Polycythemia isn’t a bone marrow disease like Polycythemia Vera. It happens when something outside the body makes more red blood cells. This can be due to not getting enough oxygen, like in COPD or sleep apnea.
Other reasons include:
- Kidney or liver problems that make too much of a hormone for red blood cells.
- Using testosterone or certain medicines that help make more red blood cells.
Symptom Differences
Both conditions can cause headaches and dizziness because of more red blood cells. But, there are key differences. Secondary Polycythemia symptoms often match the cause, like breathing problems in COPD patients.
On the other hand, Polycythemia Vera might cause itching and an enlarged spleen. These symptoms are less common in Secondary Polycythemia.
Is Polycythemia Vera Cancer? Understanding the Classification
Polycythemia vera is a condition where too many red blood cells are made. It raises a big question: is it cancer? To answer this, we need to look at its classification and related disorders.
Polycythemia vera falls under myeloproliferative neoplasm. This is a group of blood cancers that make too many blood cells. These conditions are chronic and can turn into more serious blood cancers, like acute myeloid leukemia (AML).
Myeloproliferative Neoplasms Explained
Myeloproliferative neoplasms are diseases where the bone marrow makes too many blood cells. This can make blood thicker, raising the risk of blood clots and heart problems. The main types are polycythemia vera, essential thrombocythemia, and primary myelofibrosis.
Being classified as a myeloproliferative neoplasm means polycythemia vera has some cancer-like traits. But it’s mainly known for making too many red blood cells.
Progression and Prognosis
How fast polycythemia vera gets worse can vary a lot. Some people might not show symptoms for years, while others might see it get worse quickly. With the right treatment, the outlook for polycythemia vera is usually good. This can help manage symptoms and lower the chance of serious problems.
Things that can affect how well someone does include certain genetic changes, like the JAK2 mutation. How well someone responds to treatment also plays a big role. Keeping a close eye on the disease and adjusting treatment plans is key to managing it well.
Knowing that polycythemia vera is a blood cancer helps both patients and doctors. It lets them understand how it can progress and why personalized treatment plans are so important.
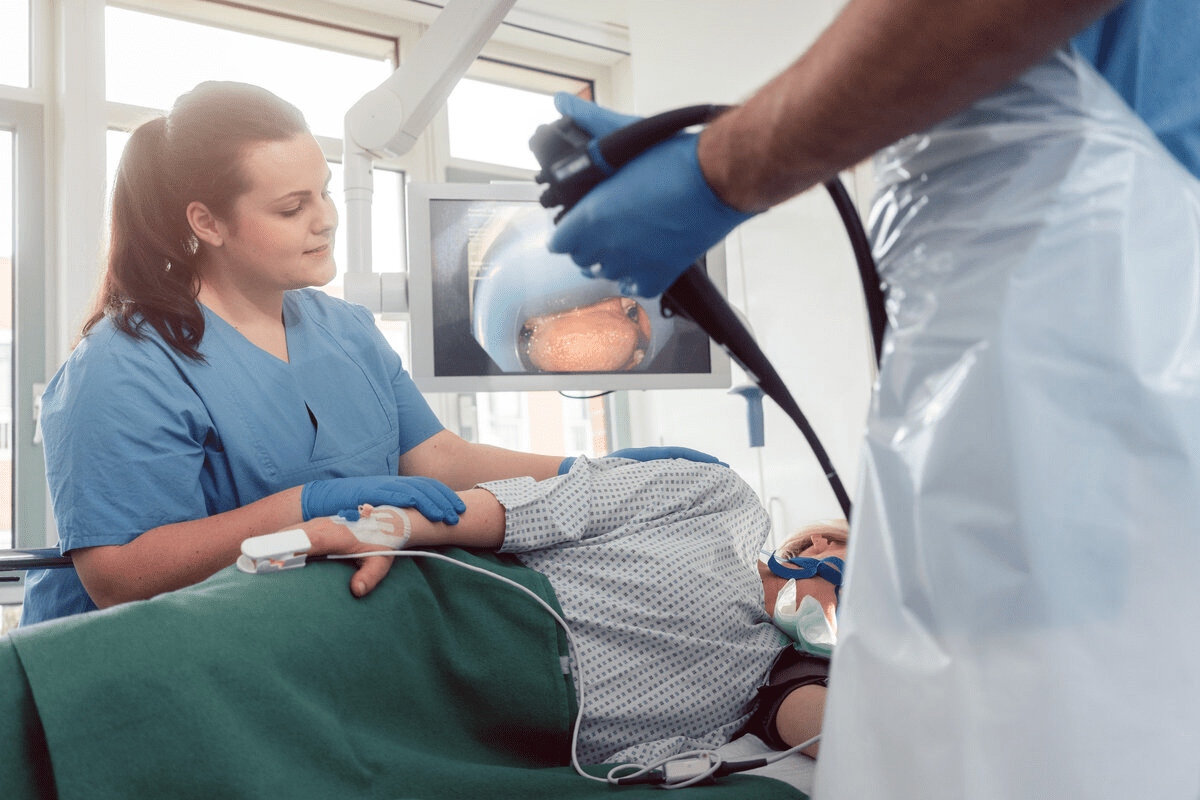
Diagnostic Journey for Polycythemia Vera
To find out if you have polycythemia vera, doctors use blood tests, bone marrow exams, and more. This mix of tests is key to correctly identifying the condition and telling it apart from others.
Blood Tests
Blood tests are the first step in diagnosing polycythemia vera. They check the levels of red and white blood cells, and platelets. A high hematocrit or hemoglobin level is a sign of too many red blood cells. Blood tests also look for odd counts of white blood cells and platelets, which are common in this condition.
Bone Marrow Biopsy
A bone marrow biopsy is a vital test. It looks at bone marrow tissue to see how blood cells are made. In polycythemia vera, the bone marrow shows signs like too many cells and megakaryocytes.
Other Diagnostic Tests
Other tests are used to help confirm the diagnosis and check for other causes. These include genetic tests for JAK2 mutations and imaging to look for blood clots or other problems.
Doctors use all these test results to accurately diagnose polycythemia vera. Then, they create a treatment plan that fits the patient’s needs.
Treatment Approaches for Polycythemia Vera
We focus on controlling symptoms and preventing blood clots for polycythemia vera. We use a mix of treatments that fit each patient’s needs.
Phlebotomy
Phlebotomy is a key treatment for polycythemia vera. It involves removing blood to lower red blood cell count. This reduces the risk of blood clots.
It also helps with symptoms like headaches and dizziness. Regular phlebotomy sessions are important for managing the condition.
The number of sessions needed varies based on the patient’s condition and how well they respond to treatment.
Medications
Medications are also vital in treating polycythemia vera. They include:
- Hydroxyurea: To slow down red blood cell production
- Interferon alfa: To control the immune system
- Aspirin: To prevent blood clots
We choose medications based on the patient’s needs and medical history. Our goal is to reduce symptoms and prevent complications while keeping quality of life high.
Lifestyle Modifications
Lifestyle changes are also key in managing polycythemia vera. We suggest:
- Drinking plenty of water to thin blood
- Avoiding extreme temperatures
- Eating healthy and exercising regularly
These changes help patients manage their symptoms better and improve their overall health.
| Treatment Approach | Purpose | Benefits |
| Phlebotomy | Reduce red blood cell mass | Lowers risk of thrombosis, alleviates symptoms |
| Medications | Regulate blood cell production, prevent clots | Reduces symptoms, prevents complications |
| Lifestyle Modifications | Improve overall health | Enhances symptom management, improves quality of life |
Conclusion
Polycythemia vera is a rare blood cancer. It causes too many red and white blood cells and platelets. We’ve looked at what it is, its symptoms, how it’s diagnosed, and how it’s treated. Knowing the early signs of polycythemia vera is key. Symptoms like headaches and dizziness can signal the condition. It’s also important to know the difference between polycythemia vera and secondary polycythemia. Even though it’s a blood cancer, polycythemia vera isn’t always deadly. With the right treatment, like phlebotomy and medications, symptoms can be managed. This reduces the risk of serious problems. If symptoms get worse, it’s important to see a doctor.
In summary, treating polycythemia vera needs a team effort. By understanding the condition, patients and doctors can work together. This helps improve life quality and outcomes.
FAQ
What is polycythemia vera?
Polycythemia vera is a rare blood disorder. It causes the bone marrow to make too many red and white blood cells and platelets.
What are the symptoms of polycythemia vera?
Symptoms include headaches and dizziness. You might also see vision changes and tinnitus. Facial redness, itching, and easy bruising are common too. Other symptoms are hypertension, chest pain, and thrombotic events.
Is polycythemia vera a form of cancer?
Yes, it’s classified as a myeloproliferative neoplasm. This is a type of blood cancer that affects how blood cells are made in the bone marrow.
How is polycythemia vera diagnosed?
Doctors use blood tests to check for too many red blood cells. They also do a bone marrow biopsy. Other tests help rule out secondary polycythemia.
What is the difference between polycythemia vera and secondary polycythemia?
Polycythemia vera is a primary condition caused by a genetic mutation. Secondary polycythemia is caused by external factors like chronic hypoxia or tumors.
How is polycythemia vera treated?
Treatment includes phlebotomy to lower red blood cell count. Medications help manage symptoms and prevent complications. Lifestyle changes also reduce the risk of thrombotic events.
What are the risks associated with polycythemia vera?
Risks include thrombotic events and cardiovascular complications. There’s also a risk of transforming into more aggressive blood cancers.
Can polycythemia vera be cured?
There’s no cure, but treatment can manage symptoms and prevent complications. This improves quality of life.
How often should I have check-ups if I have polycythemia vera?
Regular check-ups with your healthcare provider are key. They help monitor your condition and adjust treatment as needed.
What lifestyle changes can help manage polycythemia vera?
Stay hydrated and avoid extreme temperatures. Manage stress and avoid activities that increase injury or bleeding risk.
References
- Miller, J. W. (2024). Excess folic acid and vitamin B12 deficiency. Current Medicinal Chemistry, 31(20), 2587“2598. https://journals.sagepub.com/doi/10.1177/03795721241229503
- National Institutes of Health Office of Dietary Supplements. (2025, October 6). Vitamin B12 – Health Professional Fact Sheet. https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
What is polycythemia vera?
Polycythemia vera is a rare blood disorder. It causes the bone marrow to make too many red and white blood cells and platelets.
What are the symptoms of polycythemia vera?
Symptoms include headaches and dizziness. You might also see vision changes and tinnitus. Facial redness, itching, and easy bruising are common too. Other symptoms are hypertension, chest pain, and thrombotic events.
Is polycythemia vera a form of cancer?
Yes, it’s classified as a myeloproliferative neoplasm. This is a type of blood cancer that affects how blood cells are made in the bone marrow.
How is polycythemia vera diagnosed?
Doctors use blood tests to check for too many red blood cells. They also do a bone marrow biopsy. Other tests help rule out secondary polycythemia.
What is the difference between polycythemia vera and secondary polycythemia?
Polycythemia vera is a primary condition caused by a genetic mutation. Secondary polycythemia is caused by external factors like chronic hypoxia or tumors.
How is polycythemia vera treated?
Treatment includes phlebotomy to lower red blood cell count. Medications help manage symptoms and prevent complications. Lifestyle changes also reduce the risk of thrombotic events.
What are the risks associated with polycythemia vera?
Risks include thrombotic events and cardiovascular complications. There’s also a risk of transforming into more aggressive blood cancers.
Can polycythemia vera be cured?
There’s no cure, but treatment can manage symptoms and prevent complications. This improves quality of life.
How often should I have check-ups if I have polycythemia vera?
Regular check-ups with your healthcare provider are key. They help monitor your condition and adjust treatment as needed.
What lifestyle changes can help manage polycythemia vera?
Stay hydrated and avoid extreme temperatures. Manage stress and avoid activities that increase injury or bleeding risk.