For patients with chronic medical conditions, implanted ports are a lifeline. They ensure safe and repeated vascular access. At Liv Hospital, we focus on a precise and sterile port a cath access procedure. This is to reduce complications and discomfort. Master the port a cath access procedure. Our simple, step-by-step guide ensures a safe and sterile connection every time.
An implanted port, like a Port-A-Cath, is a device inserted under the skin. It has a portal and a catheter. This setup makes it easy to access veins for medication, transfusions, or blood draws.
We follow international standards and prioritize patient wellbeing in our mediport access procedure. In this guide, we’ll show you the step-by-step process. This will empower patients and caregivers to handle this critical procedure.
Key Takeaways
- Understanding the importance of sterile technique in Port-A-Cath access.
- Knowledge of the equipment and preparation required for the procedure.
- Familiarity with the step-by-step process of accessing a Port-A-Cath.
- Awareness of the necessary aftercare to minimize complications.
- The role of patient education in safe Port-A-Cath management.
Understanding Port-A-Cath Devices

Port-A-Cath devices have changed how we give medicines and treatments for long-term health issues. They offer a safe way to get to the blood, making life better for those on long-term treatments.
What is a Port-A-Cath?
A Port-A-Cath, or implanted port, is a central venous access device (CVAD) put under the skin, usually in the chest or arm. It has a portal and a catheter. These help put medicines, blood products, and nutrition straight into the blood.
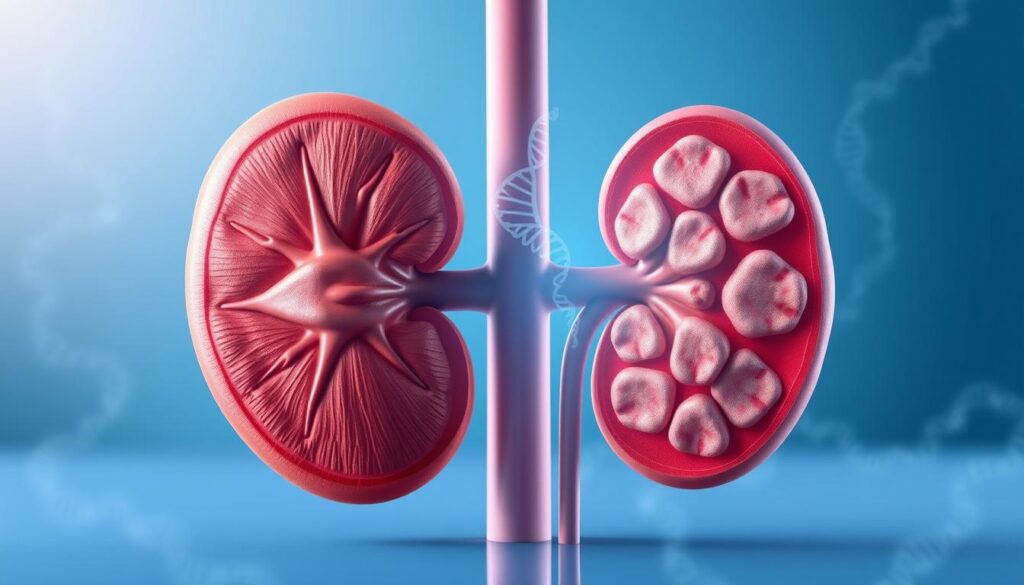
Types of Implanted Ports
There are many types of implanted ports, each with its own benefits. The right port depends on the patient’s needs, treatment type, and how long they’ll need it. Some are for high-pressure shots, while others are for ongoing or occasional drips.
Indications for Port-A-Cath Use
Port-A-Cath devices are for patients needing long-term access to their blood for treatments. They’re great for those with chronic conditions, like cancer, who need treatments often.
Knowing about Port-A-Cath devices helps healthcare workers give the best care. They ensure safe and effective access to the blood for patients with these implants.
Essential Equipment for Port Access
The right equipment is key for safe and successful Port-A-Cath access. We must make sure all needed supplies are ready for healthcare professionals.
Required Supplies Checklist
To safely access a Port-A-Cath, we need these essential supplies:
- Port Access Kit
- Non-coring (Huber) needles
- Antiseptic solutions (e.g., chlorhexidine)
- Sterile gloves
- Sterile drape
- Syringes and needles for medication administration
Having these supplies ready helps keep the environment clean. It also lowers the chance of problems during the procedure.
| Supply | Purpose |
| Port Access Kit | Contains necessary components for accessing the Port-A-Cath |
| Non-coring (Huber) needles | Designed to prevent damage to the port septum |
| Antiseptic solutions | Reduces the risk of infection |
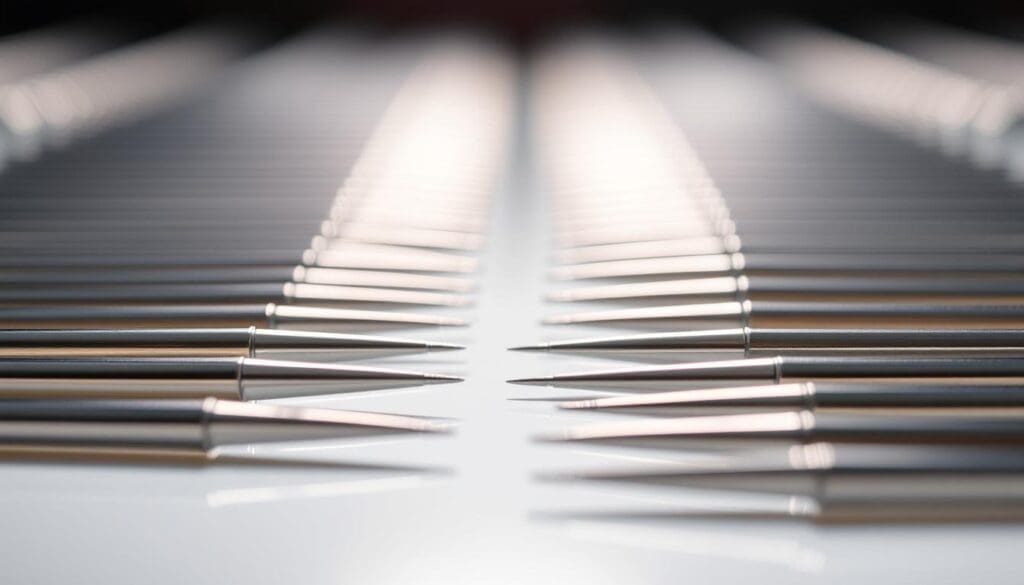
Understanding Non-Coring Huber Needles
Non-coring Huber needles are made for accessing implanted ports. They have a special tip that prevents damage to the port’s septum. This reduces the risk of problems.
Using non-coring needles is very important for Port-A-Cath access. It helps keep the device working well for a long time.
Antiseptic Solutions and Their Efficacy
Antiseptic solutions are key in preventing infection during Port-A-Cath access. Chlorhexidine is a top choice because it fights many kinds of germs well.
Using chlorhexidine for skin prep before accessing the Port-A-Cath is recommended. It’s very good at cutting down the risk of infections from central lines.
Preparation Before Accessing a Port
Before we access a Port-A-Cath, we need to prepare well. This means getting everything ready for the patient and the equipment.
Patient Assessment and Identification
Assessing the patient is key before we start. We check the patient’s health, look for any signs of infection, and make sure we have the right person.
We look at the patient’s medical history and why they need the port. We also check their current health. This helps us prepare for any challenges.
Gathering and Organizing Supplies
We also need to gather all the supplies we’ll need. They must be clean, ready, and easy to find.
| Supply | Purpose |
| Non-coring Huber needle | Access the Port-A-Cath without damaging it |
| Antiseptic solution | Clean and disinfect the skin |
| Sterile gloves | Maintain asepsis during the procedure |
Proper Hand Hygiene Techniques
Keeping hands clean is very important to avoid infections. We must wash our hands with soap and water or use hand sanitizer.
Key hand hygiene practices include:
- Performing hand hygiene before and after patient contact
- Using sterile gloves during the procedure
- Ensuring that all healthcare personnel follow hand hygiene protocols
By focusing on patient assessment, supply preparation, and hand hygiene, we can ensure a safe and successful Port-A-Cath access procedure.
Setting Up a Sterile Field
A sterile field is key to reducing infection risk during Port-A-Cath access. We must follow strict rules to keep the area clean during the procedure.
Principles of Aseptic Technique
Aseptic technique stops microorganisms from entering the sterile field. Key principles include using only sterile tools, keeping the area clean, and avoiding contact with dirty surfaces.
- Use sterile gloves and gowns to prevent skin bacteria from getting into the field.
- Employ sterile drapes to block the sterile area from the outside.
- Make sure all tools are sterilized as the maker says.
Creating and Maintaining Sterility
To set up a sterile field, we first get ready the necessary sterile items, like drapes, gloves, and tools. It’s important to handle these items carefully to keep them sterile.
Keeping the field sterile is an ongoing task. We must watch out for any contact with non-sterile surfaces or objects.
Common Contamination Pitfalls
Even with careful planning, contamination can happen. Common mistakes include touching non-sterile areas with sterile gloves, not properly sterilizing tools, and letting drafts or movement disturb the field.
Knowing these risks helps us avoid them. This way, we can make sure the Port-A-Cath access goes well.
The Port-A-Cath Access Procedure: Step-by-Step Guide
To ensure safe and effective Port-A-Cath access, a systematic approach is essential. This involves several key steps that healthcare professionals must follow carefully. These steps help minimize complications and ensure patient comfort.
Patient Positioning and Comfort
Proper patient positioning is key for successful Port-A-Cath access. We start by making sure the patient is comfortable and relaxed, usually lying down. The patient’s arm on the side of the Port-A-Cath should be relaxed and slightly raised.
“Comfort is key to reducing anxiety and ensuring a smooth procedure,” as emphasized by medical professionals. We then check that the patient is comfortable and ready for the procedure. We explain each step to ease any concerns they may have.
Locating and Palpating the Port
Next, we locate the Port-A-Cath by palpation. Using our fingertips, we gently feel for the reservoir under the skin. This step is critical for accurate needle placement.
Once located, we mark the center of the port with a sterile marker. This guides our needle insertion.
Chlorhexidine Skin Preparation Protocol
Effective skin preparation is vital to prevent infections. We use a chlorhexidine-based antiseptic solution, applying it in a back-and-forth motion for at least 30 seconds. The area is allowed to air dry completely before proceeding.
Chlorhexidine preparation is a critical step in reducing the risk of catheter-related bloodstream infections.
Proper Needle Insertion Technique
With the skin prepared, we insert the non-coring Huber needle at a 90-degree angle to the skin. The needle is advanced through the skin and into the port septum until it reaches the bottom of the reservoir. A slight “give” or “pop” may be felt as the needle penetrates the septum.
As one medical expert notes, “Proper needle insertion technique is fundamental to successful Port-A-Cath access and minimizing patient discomfort.”
Verifying Proper Placement
The success of a Port-A-Cath procedure depends on accurate placement. It’s key to make sure the needle is in the right spot for safe use.
Blood Return Assessment
Checking for blood return is a main way to confirm placement. We try to get blood into the syringe to see if the needle is in the right place.
Getting blood back smoothly means the needle is in the right spot. Trouble getting blood could mean a problem with the needle or port.
Saline Flushing Protocols
Saline flushing is another important step. We use saline to check if the port works well and if there are any blockages.
This method also helps us make sure the port is in the right place. It ensures the port is clear and working right.
| Verification Method | Indicators of Proper Placement | Potential Issues |
| Blood Return Assessment | Smooth, easy flow of blood | Difficulty in obtaining blood return |
| Saline Flushing | Easy flow without resistance | Resistance or leakage during flushing |
Troubleshooting Placement Issues
If we run into problems, like trouble with blood return or saline flushing, we need to figure out what’s wrong.
Issues might include the needle being in the wrong place, the port being blocked, or the catheter not working. We might need to adjust the needle, use more imaging, or get help from other doctors.
By checking the Port-A-Cath’s placement carefully and being ready to solve problems, we can make sure it’s used safely and effectively for our patients.
Securing the Needle and Dressing Application
After accessing a Port-A-Cath, securing the needle and applying a dressing are key steps. These actions help keep the site safe and prevent problems.
Needle Stabilization Techniques
Securing the needle is very important. We use special methods to keep it in place. The main ways include:
- Using a securement device made for this purpose
- Putting a sterile dressing over the needle site
- Making sure the needle is firmly in place
Keeping the needle stable stops it from moving out of place. This could cause infections or other issues.
Types of Dressings and Selection Criteria
Choosing the right dressing is key for Port-A-Cath care. There are many dressings, each with its own benefits. We pick based on several things, like:
| Dressing Type | Characteristics | Selection Criteria |
| Gauze Dressing | Breathable, absorbent | Ideal for sites with drainage or bleeding |
| Transparent Film Dressing | Permeable to moisture vapor, allows visualization of the site | Suitable for sites with minimal drainage, allows for easy inspection |
| Chlorhexidine Gluconate (CHG) Dressing | Antimicrobial properties | Recommended for patients at high risk of infection |
Dressing Change Frequency and Documentation
How often to change dressings is important. We follow rules to decide when to change them, usually:
- Every 7 days for transparent dressings
- Every 48 hours for gauze dressings
- Right away if the dressing gets dirty, comes loose, or gets wet
Keeping accurate records of dressing changes is vital. It helps keep patients safe and ensures care is consistent.
Administering Medications Through a Port-A-Cath
Using a Port-A-Cath to give medications needs careful thought. We must know which medicines work well together, how to flush them out, and the types of infusions. This ensures treatments are safe and effective.
Medication Compatibility Considerations
When giving many medicines through a Port-A-Cath, it’s key to check if they mix well. Some medicines don’t get along and can cause problems. We must test each medicine before we give it.
Table: Medication Compatibility Chart
| Medication | Compatible With | Incompatible With |
| Antibiotics | Saline, Heparin | Certain Chemotherapy Agents |
| Chemotherapy | Specific Agents Vary | Some Antibiotics, Steroids |
| Nutritional Supplements | Most IV Fluids | Certain Medications |
Flushing Between Medications
Flushing between medicines is vital to avoid bad reactions and make sure each medicine works right. Saline is usually the best choice for flushing because it goes well with most medicines.
Proper flushing technique involves:
- Using a push-pause method to create turbulence
- Flushing with 10-20 mL of saline
- Checking for blood return before and after flushing
Continuous vs. Intermittent Infusions
Choosing between continuous and intermittent infusions depends on the medicine and treatment plan. Continuous infusions give a steady flow of medicine, while intermittent infusions give medicine at set times.
It’s important to know the differences between these infusion types for good treatment planning. We must think about the medicine’s half-life, the patient’s health, and the treatment goals. This helps decide between continuous and intermittent infusions.
Blood Sampling From a Port-A-Cath
Getting blood from a Port-A-Cath needs careful steps to avoid contamination and get accurate lab results. Healthcare pros must follow strict rules to keep the sample safe and the patient safe too.
Discard Volume Considerations
Choosing the right discard volume is key when taking blood from a Port-A-Cath. The discard volume is the blood thrown away before getting the sample for tests. Enough discard volume stops the sample from getting diluted or contaminated. It’s usually 3-5 mL, but can change based on the device and patient.
We must think about the dead space in the Port-A-Cath system. Getting the discard volume right helps get a sample that really shows the patient’s health.
Preventing Sample Contamination
Stopping sample contamination is very important when taking blood from a Port-A-Cath. Contamination can happen from bad technique, not cleaning the skin well, or not using sterile tools. To avoid contamination, we must stick to strict aseptic techniques. This means wearing sterile gloves, cleaning the skin right, and not touching the needle to non-sterile things.
Using a new, sterile needle for the blood sample also helps. It’s also key to handle the sample tubes carefully to avoid contamination.
Post-Draw Flushing Requirements
After taking the blood, flushing the Port-A-Cath well is very important. Flushing with saline solution and heparin lock, if needed, keeps the catheter open. How much and how to flush is important to keep the catheter working right.
Flushing right also cuts down infection risk and keeps the Port-A-Cath working longer. We should write down the flushing steps in the patient’s file, including what solutions were used and how the patient did.
Infection Prevention During Port-A-Cath Access Procedure
Accessing Port-A-Cath devices carries a risk of infection. We must follow strict infection control measures to keep patients safe. This includes following detailed protocols to avoid complications.
Evidence-Based Infection Control Practices
Starting with evidence-based practices is key. This includes hand hygiene, aseptic technique, and the right personal protective equipment (PPE). Training all healthcare workers is vital to keep the environment clean during Port-A-Cath access.
Hand hygiene is the foundation of preventing infections. We use alcohol-based hand rubs or soap and water before and after touching the Port-A-Cath site. Sterile gloves and drapes also play a role in keeping things clean during the procedure.
Central Line-Associated Bloodstream Infections (CLABSIs)
Central Line-Associated Bloodstream Infections (CLABSIs) are a big worry for patients with Port-A-Cath devices. These infections can cause serious health problems, death, and higher healthcare costs. We use several methods to stop CLABSIs, like using sterile barriers during insertion and avoiding unnecessary access.
Watching for CLABSIs and tracking their rates is important. This helps us find ways to improve our infection control. We take action to keep our patients safe.
Site Rotation and Documentation
Changing the needle site and keeping detailed records are key to preventing infections. Rotating the site helps avoid skin problems and infection risks. We document each procedure, including the site used and any issues.
Good documentation helps with patient care and spotting problems early. We make sure all important information is in the patient’s medical record. This gives a clear view of their Port-A-Cath care.
Deaccessing the Port-A-Cath
Proper deaccessing of a Port-A-Cath is key for keeping the device working right and ensuring patient safety. This process involves taking out the needle and flushing the port with heparin to keep it open.
When to Deaccess
We decide to deaccess a Port-A-Cath when the treatment is done or the port is not needed for a long time. We check the patient’s medical needs and the port’s condition before we do it.
Safe Needle Removal Technique
Removing the needle from a Port-A-Cath needs a careful method to avoid problems. We hold the port steady with one hand and slowly pull out the needle with the other. It’s important not to press too hard or twist, as this could hurt the patient or damage the port.
Final Heparin Flushing Protocol
After taking out the needle, we flush the Port-A-Cath with heparin to keep it open. We use 10 mL of saline and then a heparin solution (usually 100-500 units/mL). The exact amount and type of heparin can change based on where we are and the type of Port-A-Cath.
| Step | Action | Volume/Concentration |
| 1 | Saline Flush | 10 mL |
| 2 | Heparin Flush | 100-500 units/mL |
“The use of heparin flushes has been a cornerstone in maintaining the patency of central venous catheters, including Port-A-Caths.”
Source: Journal of Vascular Access
By following these steps and guidelines, we can safely and effectively deaccess the Port-A-Cath. This keeps the patient comfortable and the device working well.
Conclusion
Proper care and management of a Port-A-Cath are key for patient safety and effective treatment. By following the guidelines in this article, healthcare professionals can ensure safe vascular access for patients. This is important for those with chronic medical conditions.
We’ve shown how understanding the Port-A-Cath device, proper technique, and infection prevention are vital. Effective vascular access management helps prevent complications. It also ensures the delivery of prescribed treatments.
By following best practices in port a cath care, healthcare providers can lower the risk of infections and complications. This improves patient outcomes. It’s important to keep educating and training healthcare professionals as we advance in vascular access management.
FAQ
What is a Port-A-Cath and how does it work?
A Port-A-Cath is a device implanted under the skin. It allows for easy access to a vein. This is for administering medications, nutrients, or blood sampling. It has a portal and a catheter for safe treatment delivery.
What are the indications for using a Port-A-Cath?
Port-A-Caths are used for long-term intravenous therapy. This includes chemotherapy, antibiotics, or nutritional support. They are also for patients with difficult venous access or frequent blood sampling needs.
How do I access a Port-A-Cath?
To access a Port-A-Cath, we follow a detailed procedure. This includes patient positioning and locating the port. We prepare the skin and insert a non-coring Huber needle.
After insertion, we check for blood return and flush with saline. This confirms proper placement.
What type of needle is used to access a Port-A-Cath?
A non-coring Huber needle is used. It prevents damage to the port septum. This minimizes the risk of complications.
How do I secure the needle and apply a dressing after accessing a Port-A-Cath?
After accessing, we stabilize the needle and apply a sterile dressing. The dressing type varies based on patient needs and facility policies.
How often should I change the dressing over a Port-A-Cath?
Dressing changes depend on the type and patient condition. Generally, they are changed every 7 days or as needed.
Can I administer medications through a Port-A-Cath?
Yes, medications can be administered through a Port-A-Cath. We follow guidelines for compatibility and infusion techniques. This ensures safe treatment.
How do I prevent infection when accessing a Port-A-Cath?
To prevent infection, we follow infection control practices. This includes hand hygiene, skin preparation, and using sterile equipment. We monitor the site for signs of infection.
What are the signs of infection or complications associated with a Port-A-Cath?
Signs of infection or complications include redness, swelling, or pain. Fever or difficulty accessing the port are also indicators. We closely monitor patients for these signs.
How do I deaccess a Port-A-Cath?
To deaccess a Port-A-Cath, we remove the needle and flush with heparin. We document the procedure to prevent complications and maintain patency.
What is the final heparin flushing protocol when deaccessing a Port-A-Cath?
The final heparin flushing protocol uses a heparin solution. This maintains patency and prevents clotting. The protocol varies based on facility policies and patient needs.
How do I perform blood sampling from a Port-A-Cath?
Blood sampling requires careful technique. We follow guidelines for discard volume and sample collection. Post-draw flushing prevents contamination and ensures accurate results.
References
- Erdemir, A., Altun, T., & Şenol, Y. (2023). Impact of central venous port implantation method and route on complications: A multicenter retrospective study. PMC (Article),https://pmc.ncbi.nlm.nih.gov/articles/PMC9846971/
- Samad, A. M. A., Annadurai, R., Chandrasekaran, V., & Kannan, S. (2015). Complications of Port-A-Cath implantation: A single centre experience. European Journal of Oncology Nursing, 19(3), 318-322.https://www.sciencedirect.com/science/article/pii/S0378603X15001242
- Suárez-Brito, A., Martín-Rodríguez, H. M., & Vázquez-Suárez, J. M. (2024). Clinical applications and research progress of totally implantable venous access port (TIVAP): A systematic review. Frontiers in Oncology, https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1519728/full