
Recovering from a blood clot in the lungs needs careful medical care and a clear plan. At LivHospital, we know how important a safe and quick recovery is. The time it takes to get better can vary a lot, usually taking weeks to months.
Anticoagulant treatment is key in stopping new clots and helping dissolve old ones. Our goal is to offer top-notch, internationally recognized treatments to help you get better.

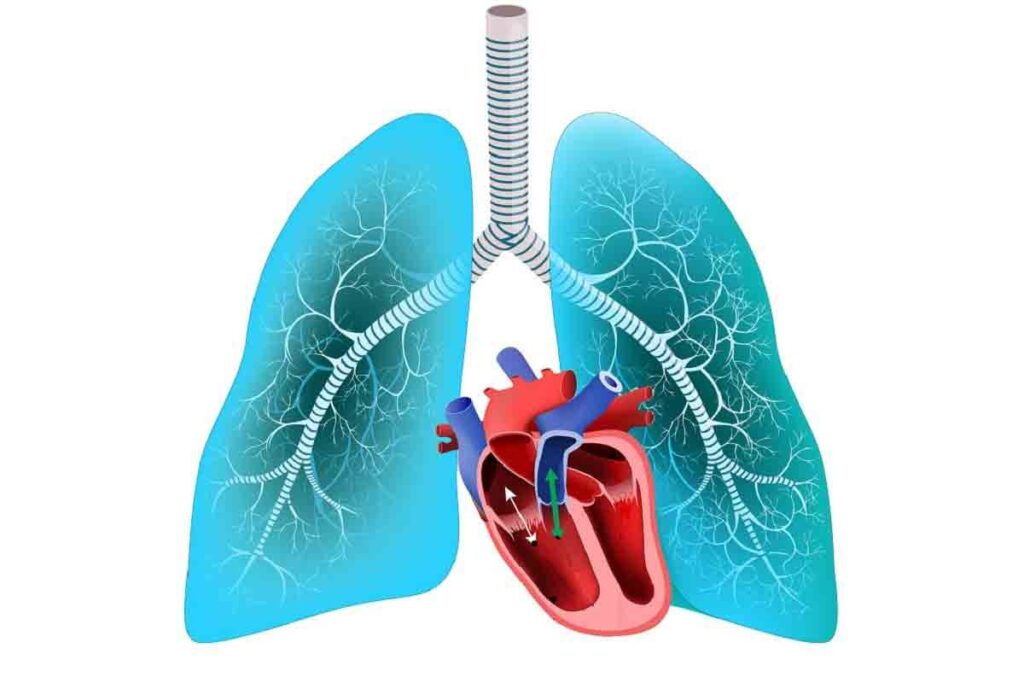
A pulmonary embolism occurs when a blood clot from the legs travels to the lungs. It blocks blood flow, harming the lungs and overall health. This can be very dangerous if not treated quickly.
Blood clots that cause pulmonary embolism usually start in the legs. Prolonged sitting, genetic factors, and some medical conditions can raise the risk.
When a clot breaks free, it moves through the blood to the lungs. It can block a pulmonary artery. This puts strain on the heart and lowers blood oxygen levels.
The respiratory system is greatly affected by a pulmonary embolism. The clot can reduce blood oxygen, causing shortness of breath and rapid breathing. In severe cases, it can lead to respiratory failure.
Symptoms of pulmonary embolism include sudden shortness of breath and chest pain. Coughing up blood is also a sign. Doctors use CT scans and blood tests to diagnose it.
| Symptoms | Diagnostic Tests | Immediate Effects |
| Shortness of breath | CT Scan | Reduced oxygen levels |
| Chest pain | Blood tests | Strain on the heart |
| Coughing up blood | Imaging tests | Respiratory distress |
Knowing the typical recovery time for pulmonary embolism is key for patients and their families. The road to recovery is different for everyone. Yet, most people follow a similar path, divided into several stages.
The recovery starts in the hospital, where patients get immediate care. The hospital stay length depends on the condition’s severity and the patient’s health. Patients are watched closely and start anticoagulant treatment to stop more clots.
After leaving the hospital, the first week at home is all about rest. It’s important to avoid hard activities during this time.
In the early recovery phase, symptoms start to get better. Patients slowly increase their physical activity, as advised by doctors. It’s important to stick to medication and keep up with doctor’s appointments.
Being aware of any worsening symptoms or complications is key during this time.
In the second and third months, health keeps improving, and symptoms lessen. This is a time to build strength and endurance through exercise and physical therapy. It’s also important to keep taking anticoagulant medication and make lifestyle changes to prevent future problems.
Full recovery from pulmonary embolism can take 3 to 6 months. The recovery time depends on the clot size, location, underlying health issues, and treatment success. Working closely with healthcare providers is vital to track progress and address any issues that come up.
The question of whether pulmonary embolism will completely go away is complex. It depends on several factors. The effectiveness of treatment, like anticoagulant therapy, plays a key role in determining the outcome.
Anticoagulants are a key part of treating pulmonary embolism. They prevent new blood clots and help dissolve existing ones naturally. Anticoagulation therapy starts quickly after diagnosis to stop new clots and dissolve old ones.
Anticoagulants don’t directly dissolve clots. Instead, they help the body’s natural processes break down clots. How long someone needs to take anticoagulants depends on their risk factors and the severity of the pulmonary embolism.
Many patients see big improvements after treatment. But, how much they improve can vary. Some people may have residual symptoms, like shortness of breath or fatigue, for weeks or months after diagnosis.
Having residual symptoms doesn’t mean the pulmonary embolism didn’t resolve. It might show the body is slowly recovering or has underlying conditions that caused the initial event.
Most people who have had a pulmonary embolism can get their lung function back to normal or close to it. But, how much they recover can depend on several things. These include the size and location of the clot, any lung disease they might have, and how well the anticoagulant therapy works.
Long-term lung function after a pulmonary embolism is usually good. But, some people might have lasting exercise limits or chronic thromboembolic pulmonary hypertension (CTEPH), a rare but serious condition.
Many factors affect how long it takes to recover from blood clots in the lungs. Knowing these factors helps manage expectations and guide the recovery process.
The size, location, and severity of the clot matter a lot. Larger clots or those in critical areas can cause more severe symptoms. This can lead to a longer recovery time.
The severity of the clot also plays a role. It affects blood pressure and oxygen levels. Patients with severe clots may need closer monitoring and more aggressive treatment.
Pre-existing health conditions can make recovery harder. Conditions like heart disease or cancer can affect how well the body recovers. These conditions may also change the treatment plan.
For example, kidney disease may require special medication adjustments. Liver disease needs careful monitoring because of its role in clotting.
Age and fitness level are important too. Older adults may take longer to recover due to health issues. Younger, fitter people might recover faster.
Being physically fit can help recovery by improving heart function. Doctors may recommend gentle exercise to aid in recovery.
Sometimes, surgery is needed to treat blood clots in the lungs. Procedures like removing the clot or placing a filter can affect recovery time. These are usually for severe cases or when anticoagulants can’t be used.
Deciding on surgery depends on the patient’s health and the clot’s severity. Recovery from surgery adds to the overall time needed to get better.
Medical treatments are key in recovering from pulmonary embolism. We use different therapies to help the body heal, stop new clots, and manage symptoms.
Anticoagulation therapy is the main treatment for pulmonary embolism. Anticoagulants prevent new clots and stop existing ones from growing. There are two main types:
Newer oral anticoagulants (NOACs) like rivaroxaban and apixaban don’t need blood monitoring.
In severe cases, or when therapy doesn’t work, surgery might be needed. This includes:
These surgeries are for life-threatening cases or high-risk situations.
Regular tests and monitoring are vital for managing pulmonary embolism recovery. This includes:
By keeping a close eye on the patient, we can adjust treatments for the best results.
Following your medication regimen is key to recovering safely after a pulmonary embolism. Adherence to anticoagulant therapy is vital to prevent more clots and help dissolve existing ones.
Anticoagulants are essential in treating pulmonary embolism. Understanding their role helps patients see why their medication is so important. These drugs stop the body from forming new clots and prevent existing ones from growing.
Anticoagulants come in different forms, like tablets and injectables. Common ones for pulmonary embolism include warfarin, rivaroxaban, apixaban, and dabigatran. Each has a specific dosage schedule that must be followed.
It’s important to know that anticoagulant therapy needs regular checks. For some, like warfarin, blood tests are needed to monitor the INR, which shows how well the blood clots.
Anticoagulants are lifesaving but can cause side effects. The main risk is bleeding. Patients might bruise more easily, have nosebleeds, or bleed from cuts more than usual.
To handle these risks, knowing the signs of serious bleeding is key. These include heavy bleeding, severe headache, or abdominal pain. If you experience these, get medical help right away.
Sticking to your anticoagulant regimen is vital for managing pulmonary embolism. Skipping doses or taking them irregularly can lead to inadequate protection against clots.
“Adherence to anticoagulation therapy is a key factor in preventing recurrent venous thromboembolism.”
To stay on track, reminders, pill boxes, or apps can help. Regular check-ups with your healthcare provider are also important. They help ensure your treatment is working and make any needed changes.
By sticking to your medication plan, you can greatly improve your chances of a full recovery from pulmonary embolism.
Recovering from pulmonary embolism means finding the right balance between rest and activity. It’s important to know how to safely start and increase physical activity. This helps improve our health and well-being.
In the early stages, start with low-intensity exercises that are easy on the body. Safe options include gentle stretching, short walks, and deep breathing exercises. These activities help improve circulation, reduce stiffness, and promote overall cardiovascular health.
As you get better, it’s time to slowly increase your physical activity. Listen to your body and only make adjustments based on your healthcare provider’s guidance. Usually, patients can start increasing their activity levels around 2-4 weeks after diagnosis, depending on their individual condition and response to treatment.
Physical therapists are key in guiding patients through recovery. They provide personalized exercise plans tailored to each patient’s needs and limitations. Working with a physical therapist can help ensure a safe and effective return to physical activity.
By gradually increasing physical activity with the help of healthcare professionals, patients can greatly improve their recovery from pulmonary embolism. This improves their overall health and reduces the risk of future complications.
Recovering from a pulmonary embolism needs more than just medicine. It also requires a careful diet. A balanced diet helps your body heal and prevents future problems.
Eating foods rich in nutrients can help you get better. Foods like lean meats, fish, and legumes are great for fixing tissues. Also, fruits and veggies with antioxidants fight inflammation and boost health.
If you’re taking anticoagulants, watch what you eat. Foods with a lot of vitamin K, like leafy greens, can affect the medicine. Eating these foods regularly helps your medicine work right.
| Food | Vitamin K Content | Recommendation |
| Spinach | High | Maintain consistent intake |
| Broccoli | Moderate | Monitor intake |
| Green beans | Low | No significant impact |
Drinking enough water is key for blood health. It keeps blood from getting too thick and lowers clot risk. Drink lots of water all day.
By eating well, watching what you eat with anticoagulants, and drinking water, you can help your body heal from a pulmonary embolism.
Recovering from pulmonary embolism means keeping an eye on how we’re doing. We need to watch how our body reacts to treatment. This helps us make sure we’re getting better smoothly.
Getting better means our breathing should get easier. We should notice if we’re not getting as short of breath. Tracking these changes helps us see if our lungs are healing. Keeping a symptom journal is a good idea for doctor’s visits.
Chest discomfort is common when getting over pulmonary embolism. But, we need to tell the difference between normal symptoms and serious ones. If the pain doesn’t go away or gets worse, we need to see a doctor. Talking to our doctor about the pain helps us manage it better.
Knowing when to call the doctor is key during recovery. We should watch for signs like sudden breathing trouble, severe chest pain, or bleeding. Knowing these signs helps us act fast if something goes wrong.
Being proactive and informed helps us manage our recovery well. This way, we can avoid complications and get better faster.
Making lifestyle changes can greatly lower the chance of getting a pulmonary embolism again. We know it’s hard, but it’s key for your health and happiness.
Sitting for too long can lead to blood clots, a big worry for those who’ve had pulmonary embolism. To fight this, moving regularly is important. Try standing, stretching, and walking every hour. If you sit a lot at work, set reminders to get up and stretch.
Effective movement strategies include:
Wearing compression stockings can help stop blood clots in your legs. Follow your doctor’s advice on when to wear them, like on long trips or when sitting a lot. Also, drink lots of water and wear loose clothes to help blood flow better.
Other preventive measures to consider:
Changing risk factors is key to avoiding pulmonary embolism again. Work with your doctor to find out what risks you have and how to lower them. This might mean managing health issues, like high blood pressure or diabetes, or making lifestyle changes like quitting smoking or exercising more.
Key risk factors to modify:
By making these lifestyle changes and working with your doctor, you can lower your risk of getting a pulmonary embolism again. This will also improve your overall health.
Recovering from a pulmonary embolism is not just about physical healing. It also involves dealing with mental health challenges. Managing your mental health is key during this time. The experience can be very traumatic, causing anxiety and fear.
Many patients worry about having another pulmonary embolism. Addressing this anxiety means understanding your condition and following your treatment plan. Talking openly with your healthcare provider is also important.
Practicing mindfulness, meditation, and deep breathing can help manage anxiety.
A strong support system is essential for mental health during PE recovery. This includes family, friends, support groups, and mental health professionals. Connecting with others who have gone through similar experiences can offer comfort and reduce feelings of isolation.
We encourage patients to reach out to their loved ones and healthcare providers. This helps build a strong support network.
It’s normal to feel overwhelmed during recovery. But, if you’re feeling anxious, depressed, or have other mental health concerns, you need professional help. Recognizing the signs that you need support is important.
If your mental health is affecting your daily life, it’s time to seek help. A mental health professional can provide the support you need.
By focusing on mental health and seeking help when needed, patients can better handle the challenges of PE recovery. We aim to provide care that covers both physical and mental aspects of recovery.
Deciding when to go back to work after a pulmonary embolism is important. It’s about being ready physically and mentally. You also need to think about what your job requires.
Going back too soon can be risky. Waiting too long can cause delays. So, it’s key to plan carefully.
Talk to your healthcare provider about your limits before going back to work. They can tell you how far you’ve come and what you can do safely.
Some things to talk about include:
Depending on your job and recovery, you might need workplace changes. These can make going back to work easier.
Some changes to consider include:
Talking to your employer about these can make your work environment supportive of your recovery.
Going back to normal activities slowly is often advised. It helps avoid overdoing it and prevents complications. This lets your body get used to more demands.
Strategies for a slow return include:
Recovering from pulmonary embolism is a long journey. It needs patience, sticking to treatment plans, and making lifestyle changes. As we wrap up our talk on recovery time, let’s think about the important steps to get back to health.
We’ve seen how following medication, starting with small physical activities, eating right for healing, and managing recovery are key. These steps help people understand their recovery better.
Life after pulmonary embolism means starting a new chapter. It’s about preventing another episode and keeping overall health in check. Making smart lifestyle choices and working with doctors can lower the risk of future problems.
It’s important to keep up with our recovery plans. Getting support from doctors, family, and friends is vital. This way, we can have a successful recovery and look forward to a healthier life ahead.
Recovery from a pulmonary embolism takes time. Patients usually stay in the hospital first. Then, they recover at home for weeks. The whole process can last months.
Several things affect recovery time. These include the clot’s size and location, the patient’s health, age, and if surgery is needed.
Yes, with the right treatment, the clot usually dissolves. Symptoms get better. But, some people might have lasting lung issues.
Anticoagulants stop new clots from forming. They help the body break down the existing clot. This lowers the risk of another embolism.
Symptoms include shortness of breath, chest pain, and tiredness. These symptoms get better over weeks to months.
Yes, but it depends on the severity and your job. Talk to your doctor about when you can go back to work and what you can do.
To prevent another embolism, make lifestyle changes. Move often, wear compression stockings, and manage risk factors.
Good nutrition is key for healing. Certain foods help, and it’s important to eat right if you’re on blood thinners.
Take care of your mental health by managing anxiety and building a support network. Know when to seek help.
Follow-up tests and monitoring are vital. They help adjust treatment and catch any problems early.
Symptoms usually get better in weeks to months.
Recovery from blood clots in the lungs takes several weeks to months.
Small clots might dissolve on their own. But, a pulmonary embolism usually needs medical treatment to prevent more clots and complications.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us