Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 266,000 women in the United States are diagnosed with breast cancer each year. Many will have a lumpectomy as part of their treatment. A lumpectomy, a surgical procedure to remove cancerous tissue from the breast, requires careful preparation and understanding. It’s important for patients to be informed to feel empowered and prepared for their surgery and recovery.The critical list of questions before lumpectomy. Get the essential things you must ask your surgeon about recovery, margins, and radiation.
It’s vital to understand the procedure, risks, and recovery process. We’ll help you with the essential questions to ask during your pre-lumpectomy consultation. This way, you’ll be well-prepared for your surgery.
Key Takeaways
- Understand the importance of being informed before a lumpectomy.
- Learn the essential questions to ask during your pre-lumpectomy consultation.
- Prepare for your surgery and recovery with the right information.
- Empower yourself with knowledge to make informed decisions.
- Discover how to navigate your lumpectomy preparation effectively.
Understanding Your Breast Cancer Diagnosis
A breast cancer diagnosis significantly impacts your life, making it essential to understand it well for informed treatment decisions. We’ll help you understand the important parts of your diagnosis.
Confirming Your Diagnosis Details
It’s important to know all about your diagnosis. This means knowing the type of breast cancer, its stage, and other key details. Ask your doctor to explain your condition clearly. This will help you understand your treatment plan better.
Understanding Your Specific Type of Breast Cancer
Breast cancer is not just one disease. It’s a group of diseases with uncontrolled cell growth in the breast. There are many types, like DCIS, IDC, and ILC. Knowing your specific type of breast cancer helps choose the right treatment.
Tumor Size, Grade, and Stage Considerations
The size, grade, and stage of your tumor are very important. They help figure out your treatment and how well you might do. Tumor size is how big it is. The grade shows how much like normal cells the tumor cells are. The stage tells how far the cancer has spread. These details help decide if a lumpectomy or other treatments are right for you.
Essential Questions Before Lumpectomy About Your Surgeon’s Experience

Before you have a lumpectomy, it’s key to check your surgeon’s background. Their experience and skills can greatly affect your surgery’s success and care.
Surgeon’s Qualifications and Specialization
Find out about your surgeon’s qualifications, like their medical degree and any certifications. Being board certified in surgical oncology shows they’re an expert. Knowing their specialty can also tell you if they’re good at doing lumpectomies.
Ask about their experience with breast cancer surgeries. Also, if they’ve had special training in oncoplastic surgery. This helps you see if they can meet your needs.
Surgeon’s Monthly Lumpectomy Volume
The number of surgeries a surgeon does each month matters. Ask how many lumpectomies they do every month. Doing more surgeries means they’re more familiar with the procedure and its risks.
Monthly Lumpectomy Volume | Potential Outcome |
Low (<5) | Variable outcomes, potentially higher risk of complications |
Moderate (5-15) | Average outcomes, some risk of complications |
High (>15) | Better outcomes, lower risk of complications |
Success Rates and Outcomes
Knowing your surgeon’s success rates with lumpectomies is important. Ask about their clear margin success rates and how often they need a second surgery. Clear margins mean the tumor was removed well, avoiding more surgeries.
Also, ask how they handle complications and support patients during recovery. This shows their dedication to your care.
By asking the right questions, you can choose the best surgeon for you. A well-qualified and experienced surgeon can greatly improve your treatment’s success and your satisfaction.
Questions About Lumpectomy vs. Mastectomy Options
Choosing between lumpectomy and mastectomy is a big decision. It’s about understanding the benefits and risks of each. When you’re diagnosed with breast cancer, you have to decide which one is right for you. This choice can affect your treatment and how you feel about yourself.
Comparing Benefits and Risks of Each Approach
Lumpectomy, or breast-conserving surgery, removes the tumor and some tissue around it. It keeps most of the breast, might be less hard on your body image, and has a shorter recovery time. But, you’ll likely need radiation therapy to lower the chance of cancer coming back.
Mastectomy removes one or both breasts, either partly or fully. It might be better for getting rid of cancer, but it can affect your feelings about your body more. Losing breast tissue can be tough.
Key Considerations:
- Lumpectomy Benefits: Keeps more of the breast, less invasive, quicker recovery.
- Lumpectomy Risks: Needs radiation, might have a higher chance of cancer coming back.
- Mastectomy Benefits: Removes cancer more thoroughly, might lower the chance of cancer coming back.
- Mastectomy Risks: Loses breast tissue, longer recovery, might have surgery problems.
When Lumpectomy Is Recommended Over Mastectomy
Lumpectomy is often chosen for early-stage breast cancer. The tumor is small and can be removed without changing the breast’s look. Your doctor will consider the tumor’s size, your health, and what you prefer.
Recurrence Rates for Each Procedure
Knowing the recurrence rates for lumpectomy and mastectomy is key. Studies show lumpectomy with radiation can have similar rates to mastectomy for early-stage cancer. But, many factors can affect these rates, like the cancer’s stage and how well the tumor was removed.
Recurrence Rate Factors:
- Cancer stage at diagnosis.
- Effectiveness of surgical removal.
- Use of adjuvant therapies.
By looking at these factors and talking to your doctor, you can decide which option is best for you.
Pre-Surgery Testing and Preparation Questions
Getting ready for your lumpectomy means knowing about the tests and prep you’ll need. This info will make you feel more ready and in control.
Required Pre-Operative Tests
Your healthcare team will do several tests before your surgery. These tests check if you’re ready for the operation. You might have:
- Blood tests to see how healthy you are and find any problems.
- Imaging tests like mammograms or MRIs to look at your breast tissue closely.
- Electrocardiogram (ECG) to check your heart, if you have heart issues.
These tests help your doctors and anesthesiologists know your health. They make sure the surgery is safe for you.
Medication Adjustments Before Surgery
Tell your healthcare team about all the medicines you take. Some might need to change or stop before surgery. For example:
- Blood thinners might be stopped to avoid bleeding during surgery.
- Diabetes medications could be adjusted to keep your blood sugar right during surgery.
Always do what your healthcare team says about changing your medicines. It’s for your safety during surgery.
Fasting and Day-of-Surgery Instructions
You’ll get specific instructions for fasting and what to do on surgery day. You’ll likely be told to:
- Fast for a certain period before surgery, usually from midnight the night before.
- Avoid certain foods or drinks that could affect your surgery or anesthesia.
- Arrive at the hospital or surgical center on time, with someone to accompany you.
Following these instructions is key to your safety and the success of your surgery.
By knowing and following these guidelines, you’ll be well-prepared for your lumpectomy. You can then focus on getting better.
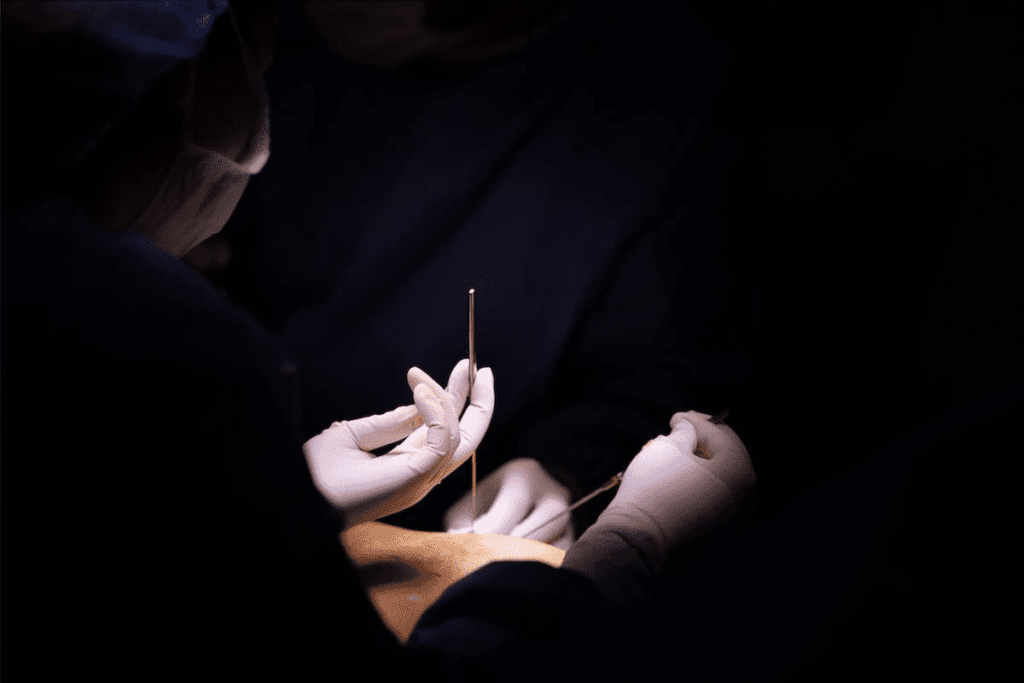
Key Questions Before Lumpectomy About the Procedure Details
Before a lumpectomy, it’s key to ask about the procedure details. This ensures you’re ready for what’s coming. Knowing the specifics can reduce anxiety and make your experience better.
Localization Procedure Questions
The localization procedure is a key part of your surgery. It finds the exact spot of the tumor or area to be removed. You should ask your surgeon about the localization method they’ll use.
Localization techniques differ, and knowing the method can make you feel more at ease. For example, wire localization uses a thin wire to guide the surgeon. Radioactive seed localization involves a small seed implanted near the tumor.
Incision Location and Size
Talking to your surgeon about the incision location and size is important. The placement and length of the incision affect the surgery’s outcome and how your breast looks afterward. Ask why they’ve chosen a specific location and size for the incision.
Knowing about the incision can help you understand the procedure better. It also helps you see how it might affect your breast’s look after surgery.
Shaving Margins Technique
The shaving margins technique is vital for removing all cancerous tissue while keeping healthy tissue. You should ask if your surgeon uses cavity shaving. This method removes more tissue around the tumor to check for cancer cells.
Procedure Detail | Description | Importance |
Localization Procedure | Method used to identify the tumor location | Ensures accurate removal of the tumor |
Incision Location and Size | Placement and length of the surgical incision | Impacts surgical outcome and cosmetic result |
Shaving Margins Technique | Method used to remove additional tissue around the tumor | Ensures removal of all cancerous tissue |
By asking these questions, you’ll understand your lumpectomy better. This can make you more confident in your treatment plan.
Anesthesia Options and Considerations
Anesthesia is key in lumpectomy procedures. Knowing your options can ease worries. It’s important to understand the types of anesthesia for pain management during surgery.
Types of Anesthesia Used for Lumpectomy
Several anesthesia types are used in lumpectomy, including:
- Local Anesthesia: Numbs the area where surgery is done, keeping you awake.
- General Anesthesia: Makes you unconscious, so you won’t feel pain.
- Conscious Sedation: Mixes drugs to relax you, but you stay awake and can talk to your team.
Potential Side Effects and Risks
Anesthesia is mostly safe, but there are risks and side effects. These include:
- Nausea and vomiting
- Sore throat or dry mouth
- Shivering or feeling cold
- Confusion or memory loss
- Allergic reactions to anesthesia medications
Talking to your anesthesiologist about these can help you understand your risks.
Pre-Existing Conditions and Anesthesia Concerns
Some health conditions can affect how you react to anesthesia. Heart disease, diabetes, or lung disease might need special care. Your healthcare team will check your health and any conditions to find the safest anesthesia for you.
Understanding your anesthesia options and talking to your healthcare provider can make you feel more ready for your lumpectomy.
Lymph Node Removal Questions to Ask
When preparing for a lumpectomy, it’s key to ask about lymph node removal. This part of breast cancer surgery can greatly impact your recovery and treatment success.
Sentinel Node Biopsy vs. Axillary Dissection
It’s important to know the difference between sentinel node biopsy and axillary dissection. Sentinel node biopsy removes the first lymph node to check if cancer has spread. Axillary dissection removes more nodes from the armpit if cancer is found in the sentinel node.
Ask your surgeon which procedure is right for you. They’ll consider your diagnosis and the risks of each.
Lymphedema Risk Assessment
Lymphedema is swelling in the arm due to lymph node removal. Your risk depends on how many nodes are removed and the surgery’s extent. Talking to your healthcare provider about your risk can help you prepare.
Risks for lymphedema include the number of nodes removed, radiation, and infection. Knowing these risks can help you prevent them.
Prevention Strategies for Lymphedema
While some risks for lymphedema can’t be changed, there are ways to lower them. Avoid heavy lifting, keep a healthy weight, and watch for injuries or infections. Early action can make a big difference if lymphedema happens.
Talk to your healthcare team about these prevention steps. They can help you create a plan to manage your risk.
Understanding Surgical Margins and Re-excision
Surgical margins can seem scary, but knowing about them helps you make better choices. When we talk about surgical margins in lumpectomy, we mean the tissue taken out with the tumor.
Clear margins mean no cancer cells are found at the edge of the removed tissue. This suggests all cancer was removed. But, if cancer cells are found at the margin, it might mean some cancer is left.
What Constitutes Clear Margins
Clear margins, or negative margins, mean the surgeon took out the tumor with healthy tissue around it. No cancer cells are found at the edge. What “clear” means can change based on the place and the cancer type.
“The margin status is a critical determinant of local recurrence risk after breast-conserving surgery.”
Margin Status | Description | Implication |
Negative (Clear) | No cancer cells at the edge | Lower risk of recurrence |
Positive | Cancer cells at the edge | Higher risk of recurrence |
Close | Cancer cells very near the edge | Variable risk, may require re-excision |
Re-excision Rates and Procedures
If margins aren’t clear, a second surgery might be needed. This is to remove more tissue to make sure all cancer is gone. How often this happens can vary, but it’s key to getting clear margins.
Re-excision Procedure: This is a second surgery to take out more tissue. The aim is to get clear margins and lower the chance of cancer coming back.
Questions About Pathology Results Timing
Knowing when to get pathology results is important. Results usually come in a week or two, but it can take longer.
Ask your doctor about when you’ll get your results. They’ll tell you what the results mean for your surgical margins.
Potential Risks and Complications to Discuss
It’s important to know the risks and complications of lumpectomy before you decide. While it’s a safe procedure, there are some risks involved.
Common Side Effects After Lumpectomy
After a lumpectomy, you might feel pain, swelling, and bruising. Some people also get temporary numbness or tingling in their breast or nipple. Most patients find some discomfort, but it usually goes away in a few weeks, a study found.
Other side effects include:
- Fatigue
- Infection
- Hematoma (collection of blood outside blood vessels)
- Seroma (collection of fluid)
Rare but Serious Complications
Though rare, serious complications can happen. These include severe infection, significant bleeding, and bad reactions to anesthesia. Lymphedema, or swelling of the arm, can also occur if lymph nodes are removed.
“Though rare, complications such as lymphedema can have a significant impact on a patient’s quality of life. Discussing these risks with your healthcare provider is essential.”
Risk Reduction Strategies
To lower the risk of complications, you can:
- Follow post-operative instructions carefully
- Go to all follow-up appointments
- Keep a healthy lifestyle, including a balanced diet and regular exercise
By understanding the risks and taking steps to prevent them, you can have a better outcome.
Hospital Stay and Immediate Post-Op Care Questions
The time after a lumpectomy is key for your recovery. Knowing what to expect can make your return to normal life easier.
Outpatient vs. Inpatient Procedures
Most lumpectomies are done on an outpatient basis. This means you can go home the same day. But, if your health or the surgery’s complexity is a concern, your doctor might suggest an inpatient procedure.
- Outpatient benefits include recovering at home and possibly saving money.
- Inpatient advantages include more monitoring by doctors, which is good for those with other health issues.
Surgical Drain Management
A surgical drain might be used during your lumpectomy to remove extra fluid. Knowing how to care for this drain is important for a smooth recovery.
Key aspects to discuss with your healthcare provider include:
- How to empty and record the drain’s output
- Signs of infection or complications related to the drain
- When the drain is expected to be removed
Pain Management Options
Managing pain well is a big part of your care after surgery. Your healthcare team will talk to you about different options, like:
- Oral medications: Pills or liquids for pain at home
- Regional anesthesia: Ways to numb the surgical area
- Alternative methods: Such as relaxation techniques or acupuncture
It’s important to follow your healthcare provider’s advice on pain management for a comfortable recovery.
Recovery Timeline and Return to Normal Activities
Knowing what to expect during your recovery can make it easier after a lumpectomy. Understanding the recovery timeline and when you can return to normal activities helps you plan. It also helps you manage your expectations.
Short-term Recovery Expectations
In the first few days after your lumpectomy, you might feel some discomfort, swelling, and bruising. These symptoms are temporary and can be managed with pain medication and rest. It’s a good idea to have someone help you during this time.
Immediate Post-Surgery Recovery Tips:
- Rest as much as possible
- Avoid heavy lifting
- Follow your surgeon’s instructions for wound care
Physical Restrictions After Surgery
After your surgery, you’ll need to avoid certain physical activities. Don’t lift heavy things, bend, or do strenuous activities for at least 2-3 weeks. Your surgeon will give you specific instructions based on your situation.
Return to Work and Exercise Guidelines
The time it takes to go back to work and start exercising again depends on your job and health. Most people can go back to work in 1-2 weeks. But, this can vary. Start with light activities like walking when you start exercising again.
Activity | Recommended Timeline |
Return to desk work | 1-2 weeks |
Return to physical labor | 2-4 weeks |
Light exercise (e.g., walking) | 1-2 weeks |
Strenuous exercise | 4-6 weeks |
It’s very important to follow your healthcare provider’s advice on your recovery and when to return to normal activities. This helps avoid complications and makes your recovery smoother.
Cosmetic Outcome Questions to Consider
When thinking about lumpectomy, talking about how it might change your breast’s look is key. Knowing what to expect can help you decide what’s best for you.
Expected Appearance Changes
After a lumpectomy, your breast might look different. These changes can vary a lot from person to person. Things like the tumor’s size and where it is, how much tissue is removed, and how you heal can affect how your breast looks.
Breast Symmetry Considerations
How even your breasts look is important. Lumpectomy might make them look uneven. Talking to your surgeon about making them look more even is important.
- Understanding the chance for unevenness
- Looking into surgery to fix it
- Using prosthetics to help evenness
Scar Management Techniques
Scars are part of healing after a lumpectomy. Good scar care can make scars look better. Techniques include massage, creams, and sometimes laser therapy. Your doctor can suggest the best way to care for your scar.
Knowing what to expect and talking to your healthcare team can help you get the best results.
Oncoplastic and Reconstruction Options
When you think about a lumpectomy, knowing about oncoplastic surgery and reconstruction is key. Oncoplastic surgery mixes cancer removal with plastic surgery to keep your breast looking good.
Immediate vs. Delayed Reconstruction
Choosing between immediate or delayed reconstruction is a big decision. Immediate reconstruction happens during your lumpectomy. Delayed reconstruction comes after your cancer treatment is done.
Immediate Reconstruction Benefits: It means fewer surgeries, might look better, and can help with feeling less stressed about losing a breast.
Delayed Reconstruction Considerations: It lets your doctors focus on treating your cancer first. You also have time to think about how to rebuild your breast.
Reconstruction Timing | Benefits | Considerations |
Immediate | Reduced number of surgeries, potentially better cosmetic outcomes | Added complexity to cancer surgery, impact on treatment timeline |
Delayed | Simplified treatment, time to think about options | More surgeries, possible emotional impact of waiting |
Oncoplastic Techniques During Lumpectomy
Oncoplastic methods can make your breast look better after a lumpectomy. These methods move your breast tissue to keep its shape after removing cancer.
Some common oncoplastic techniques include:
- Volume displacement techniques, where the remaining tissue is moved to fill the gap.
- Volume replacement techniques, where the gap is filled with tissue from elsewhere or an implant.
Insurance Coverage for Reconstruction
Knowing what your insurance covers is important when thinking about reconstruction. The Women’s Health and Cancer Rights Act (WHCRA) of 1998 says insurance must cover reconstruction after mastectomy.
But, coverage for reconstruction after lumpectomy might not be the same. Always check with your insurance to see what they cover.
Questions About Radiation After Lumpectomy
After a lumpectomy, knowing about radiation therapy is key for recovery and peace of mind. Radiation therapy is a big part of breast-conserving therapy. It aims to kill any cancer cells left in the breast, lowering the chance of cancer coming back.
When Radiation Is Recommended
Radiation therapy is often needed after a lumpectomy for early-stage breast cancer patients. The choice to have radiation depends on several things. These include the tumor’s size and grade, if cancer is in the lymph nodes, and the patient’s health. Talking to your healthcare provider is vital to know if radiation is right for you.
- Tumor size and characteristics
- Lymph node involvement
- Patient’s overall health and preferences
Radiation Timeline and Frequency
The time and frequency of radiation therapy vary. It usually starts a few weeks after the lumpectomy, when the area is healed enough. Treatment is given daily, from Monday to Friday, for weeks. Your radiation oncologist will decide the exact time and schedule based on your needs.
- Initial consultation with a radiation oncologist
- Simulation and planning
- Daily radiation treatments over several weeks
Potential Side Effects of Radiation
Radiation therapy is usually well-tolerated, but there can be side effects. Common ones include feeling tired, skin changes in the treated area, and breast swelling. Most side effects go away after treatment ends. Your healthcare team will help you manage these effects and aim for the best outcome.
Knowing about radiation therapy after a lumpectomy can make you feel more ready and in charge of your treatment. It’s important to keep in touch with your healthcare provider to answer any questions or worries you have about radiation therapy.
Conclusion: Making an Informed Decision About Your Lumpectomy
Being well-prepared is key when thinking about a lumpectomy. Knowing your diagnosis and understanding your options helps you make a choice that fits you. This choice should meet your personal and medical needs.
People who know a lot about their lumpectomy do better and are happier. We suggest using this guide to talk to your doctor. This way, you get care that’s just right for you.
Being involved in your care helps you feel sure and clear about your treatment. Your healthcare team is always there to help. They guide you and care for you to get the best results.
FAQ
What is a lumpectomy and how does it differ from a mastectomy?
A lumpectomy removes a tumor and some tissue from the breast. It aims to keep as much of the breast as possible. Unlike a mastectomy, which removes the whole breast, a lumpectomy may require radiation to kill any remaining cancer cells.
How can I assess my surgeon’s experience with lumpectomies?
Ask about your surgeon’s qualifications and how many lumpectomies they perform. Also ask about their success rates. This information can help you feel more confident in their expertise.
What are the benefits and risks of choosing lumpectomy over mastectomy?
A lumpectomy preserves more of the breast, which may offer better cosmetic results. However, it often requires radiation. A mastectomy removes more tissue, which may lower the chance of cancer returning but can significantly affect body image. Discuss both options with your doctor to determine what’s best for you.
What pre-surgery tests and preparations are necessary for a lumpectomy?
You may need imaging tests, blood work, and a review of your medical history. You might also need to stop certain medications and fast before surgery. Your doctor will provide specific instructions.
What happens during a lumpectomy procedure?
The surgeon locates the tumor using specialized techniques, removes it, and excises some surrounding tissue. They may also use margin shaving to ensure all cancer cells are removed, depending on the tumor’s size and location.
What types of anesthesia are used for lumpectomy, and what are the possible side effects?
You may receive local anesthesia with sedation or general anesthesia. Possible side effects include nausea, fatigue, and reactions to medications. Discuss anesthesia options with your anesthesiologist.
What are the differences between sentinel node biopsy and axillary dissection?
A sentinel node biopsy removes the first lymph node(s) where cancer may spread. An axillary dissection removes more lymph nodes. Sentinel node biopsy is less invasive and may reduce the risk of swelling.
How are surgical margins determined, and what happens if they are not clear?
A pathologist examines the removed tissue to check the margins. If margins are not clear, you may need additional surgery to ensure all cancer has been removed.
What are the possible risks and complications of lumpectomy?
Risks include infection, bleeding, scarring, and changes in breast sensation or appearance. Rare but serious complications may occur. Discuss these risks with your surgeon.
What can I expect during my hospital stay and immediate post-operative care?
The length of your stay depends on the surgery. You may need to manage drains, dressings, and pain. Your healthcare team will give you instructions for care at home.
How long is the recovery timeline, and when can I return to normal activities?
Recovery varies, but most patients can resume light activities within a few weeks. Heavy lifting and strenuous exercise should be avoided longer. Your surgeon will guide you on timing.
What are the possible cosmetic outcomes of lumpectomy, and how can I manage scarring?
A lumpectomy aims to preserve breast appearance, but changes in shape or scarring may occur. Oncoplastic techniques can improve cosmetic results. Discuss scar management options with your surgeon.
What are my options for oncoplastic and reconstruction surgery after lumpectomy?
Oncoplastic techniques reshape the breast during cancer surgery. Reconstruction options vary based on your anatomy, treatment needs, and personal preferences. Insurance may cover some or all options—ask your provider.
When is radiation therapy recommended after lumpectomy, and what are the possible side effects?
Radiation is commonly recommended after lumpectomy to eliminate remaining cancer cells. Side effects may include fatigue, skin irritation, and swelling. Your doctor will explain the radiation plan.
How do I navigate insurance coverage, out-of-pocket expenses, and seeking a second opinion?
Review your insurance policy and speak with your insurer to understand coverage. Out-of-pocket costs vary. Seeking a second opinion is encouraged and can help ensure you receive the best care. Financial assistance programs may be available.
What questions should I ask about my breast cancer diagnosis before undergoing a lumpectomy?
Ask about your cancer’s type, size, grade, and stage, as well as available treatment options. This information helps you understand your diagnosis and make informed decisions.
How can I prepare for the day of my lumpectomy surgery?
Follow your doctor’s instructions regarding fasting, medication adjustments, and arrival time. Understanding the process can help reduce anxiety.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK558981/