Last Updated on October 21, 2025 by mcelik
About 1 in 5,000 males worldwide are born with hemophilia. It’s a genetic disorder that makes it hard for the body to make blood clots. Clots are needed to stop bleeding. For families with a history of hemophilia, knowing how it affects pregnancy is key.
Women who carry the hemophilia gene have a good chance of passing it to their kids. Prenatal tests can tell if the baby has the condition. This helps families make informed choices and get ready for the baby’s arrival.
It’s important to understand hemophilia and pregnancy to manage risks and ensure a safe birth. Thanks to medical progress, outcomes for people with hemophilia have gotten much better. So, it’s vital for expecting parents to know about the latest prenatal tests and care.

Key Takeaways
- Prenatal testing is crucial for determining if the fetus has hemophilia.
- Understanding hemophilia’s genetic implications helps in family planning.
- Advances in medical care have improved outcomes for hemophiliacs.
- Expectant mothers who are carriers should be aware of the risks and management strategies.
- Proper prenatal care can significantly reduce complications during birth.
Understanding Hemophilia: The Basics
Hemophilia is a condition where blood can’t form clots properly. It’s usually passed down through genes. It affects the production of proteins needed for blood clotting.

What Is Hemophilia?
Hemophilia is a rare bleeding disorder. It happens when the blood can’t clot right because of missing or low levels of clotting factors. It’s often called a “bleeder’s disease.”
It can cause bleeding that lasts a long time after injuries, surgeries, or dental work. It can also lead to bleeding in joints or muscles without any injury.
Types of Hemophilia (A, B, and C)
There are three main types of hemophilia: Hemophilia A, B, and C. Hemophilia A, also known as classic hemophilia, is caused by a lack of factor VIII. Hemophilia B, also known as Christmas disease, is due to a lack of factor IX. Hemophilia C is a milder form caused by a lack of factor XI.
- Hemophilia A is the most common form, accounting for about 80% of cases.
- Hemophilia B is less common but shares similar symptoms with Hemophilia A.
- Hemophilia C is generally milder and often doesn’t cause spontaneous bleeding.
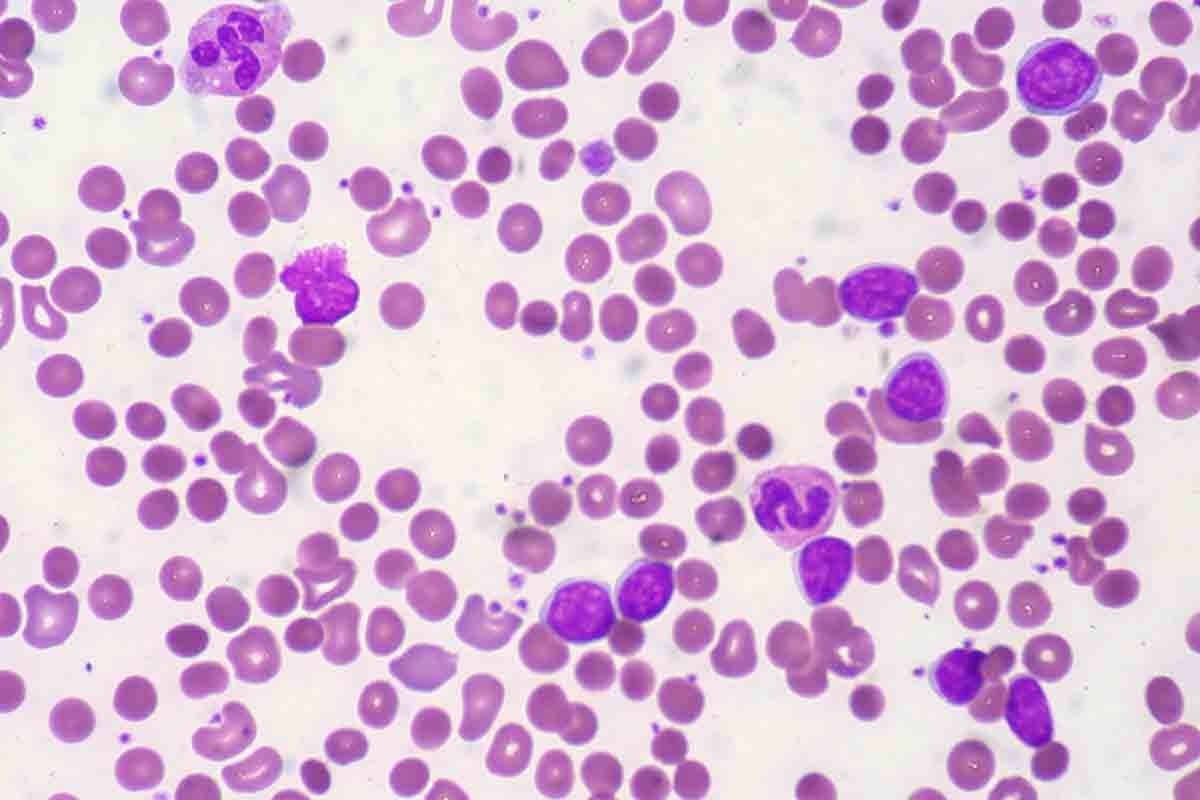
How Hemophilia Affects Blood Clotting
Hemophilia mainly affects the blood’s clotting process. Normally, when a blood vessel is injured, the body forms a clot to stop the bleeding. In individuals with hemophilia, this clotting process is impaired due to the lack or low levels of certain clotting factors.
As a result, bleeding can continue for a longer period. This can lead to complications.
The severity of hemophilia is determined by the level of clotting factor activity in the blood. Individuals with factor VIII activity levels below 1% are considered to have severe hemophilia. Those with levels between 1-5% have moderate hemophilia. And those with levels above 5% but below 40% have mild hemophilia.
Hemophilia and Gender: Can Women Have Hemophilia?
hemophilia in females
Hemophilia is often linked to males, but females can also be affected. This genetic disorder follows an X-linked inheritance pattern. This pattern is key in how it’s passed down and how it shows up in people.
X-Linked Inheritance Pattern
Hemophilia is caused by mutations in genes on the X chromosome. These genes are important for blood clotting. Since males have only one X chromosome, they’re more likely to have hemophilia because of a single mutation.
Females, with two X chromosomes, are less likely to have hemophilia. But they can be carriers. This means they can pass the mutated gene to their children.
Female Carriers vs. Affected Females
Female carriers have one normal and one mutated X chromosome. Most don’t show symptoms, but some might have mild bleeding issues. This is because of how X-chromosomes are turned on and off.
In rare cases, females can be affected. This happens if they get two mutated X chromosomes or have other genetic conditions like Turner syndrome.
Symptoms in Female Carriers
Many female carriers don’t show symptoms, but some might. They might bruise easily, have heavy periods, or bleed a lot after childbirth or surgery. How bad these symptoms are can vary a lot.
It’s important to understand hemophilia in females. Knowing they can be carriers or affected helps in early diagnosis and care. This improves their quality of life.
Hemophilia Pregnancy: Risks and Considerations
Hemophilia pregnancy comes with risks for both mom and baby. Women with hemophilia or who carry the gene face special challenges. They need special care during pregnancy.
Maternal Risks During Pregnancy
Women with hemophilia or carriers face several risks during pregnancy. Some of these risks include:
- Postpartum Hemorrhage: Women with hemophilia or carriers are at a higher risk of experiencing postpartum hemorrhage due to their bleeding disorder.
- Factor Level Changes: Pregnancy can cause changes in clotting factor levels, potentially affecting the severity of hemophilia symptoms.
- Need for Factor Replacement Therapy: Some women may require factor replacement therapy during pregnancy to manage their bleeding risks.
Fetal Risks During Pregnancy
The fetus also faces risks due to the chance of inheriting hemophilia. Key considerations include:
- Inheritance of Hemophilia: There is a risk that the fetus may inherit hemophilia if the mother is a carrier or affected.
- Prenatal Testing: Prenatal testing, such as chorionic villus sampling (CVS) or amniocentesis, can help determine if the fetus has hemophilia.
Importance of Specialized Care
Women with hemophilia or carriers need specialized care during pregnancy. This includes:
- Multidisciplinary Care Team: A team of healthcare providers, including obstetricians, hematologists, and genetic counselors, should be involved in the care.
- Genetic Counseling: Genetic counseling can help women understand their risks and make informed decisions about their pregnancy.
- Monitoring and Management: Close monitoring of clotting factor levels and management of bleeding risks are essential.
By understanding the risks and getting the right care, women with hemophilia or carriers can have a safer pregnancy and childbirth experience.
Genetic Transmission of Hemophilia
Hemophilia’s inheritance is complex, involving genetic factors that affect carrier status and the chance of having affected children. It’s caused by mutations in genes for clotting factors VIII (Hemophilia A) and IX (Hemophilia B). Knowing these genetic mechanisms is key for families dealing with hemophilia.
Inheritance Patterns
Hemophilia follows an X-linked recessive pattern. This means the genes causing it are on the X chromosome. Females have two X chromosomes, while males have one X and one Y. Males are more likely to have hemophilia because they only have one X chromosome.
Female carriers have one normal and one mutated X chromosome. They often don’t show symptoms or have mild ones due to X-chromosome inactivation. But, they can pass the mutated gene to their children.
Carrier Probability Calculations
Figuring out the chance of being a carrier is crucial for genetic counseling. For Hemophilia A and B, carrier risk is based on family history and genetic tests. A female is definitely a carrier if she has a father with hemophilia or more than one son with it.
- If a woman has one son with hemophilia and no other affected relatives, her carrier risk can be estimated using Bayesian analysis.
- Genetic testing can spot carriers by finding the specific mutation causing hemophilia in the family.
Risk of Having an Affected Child
The chance of having a child with hemophilia depends on the mother’s carrier status and the child’s gender. Sons of carrier females have a 50% chance of getting hemophilia, while daughters have a 50% chance of being carriers.
- Sons who get the mutated gene will have hemophilia.
- Daughters who get the mutated gene will usually be carriers.
Genetic counseling is essential for families with hemophilia history. It offers insights on risks and family planning options, aiding in informed decisions.
Genetic Counseling for Hemophilia Carriers
hemophilia genetic counseling
Genetic counseling for hemophilia carriers is key in helping them make smart choices about having kids. It helps them understand their genetic status and the chances of passing hemophilia to their children.
When to Seek Genetic Counseling
Carriers should get genetic counseling before they get pregnant. This way, they can grasp their risks and plan their family wisely. If there’s a family history of hemophilia, talking to a genetic counselor is crucial. They can shed light on the chances of passing the condition to future kids.
What to Expect During Counseling
In a genetic counseling session, a counselor will look at your family’s medical history. They’ll explain how hemophilia is passed down and the risks to your kids. They might also talk about different ways to have a child and prenatal tests.
The counseling is personalized to meet your needs. It’s a safe space to ask questions and get answers. This way, carriers can make choices about having kids that feel right for them.
Making Informed Family Planning Decisions
With a genetic counselor’s help, carriers can look into different family planning options. This might include prenatal tests to see if the baby has hemophilia. They might also consider things like egg donation or adoption.
Reports like the ACHA-NCHA III can help in these discussions. They offer insights into health and well-being, which are important for planning a family. By thinking about these things, carriers can make choices that fit their values and health goals.
Carrier Testing and Diagnosis
hemophilia carrier testing
Understanding if you carry the gene for hemophilia starts with testing. This is especially true if your family has a history of it. Carrier testing gives you the power to know your genetic status. This knowledge helps you plan your family and manage pregnancy better.
Methods for Identifying Carriers
There are several ways to find out if you carry the hemophilia gene. Genetic counseling often goes hand in hand with these tests. It helps you understand what your results mean for your health and family planning.
DNA sequencing is a common method. It looks at your DNA for mutations in the genes that cause hemophilia A and B. Another method is linkage analysis. It follows how the mutated gene is passed down in your family.
Interpreting Test Results
Understanding your carrier test results needs a good grasp of genetics. A positive result means you carry the mutated gene. But, a negative result doesn’t always mean you’re not a carrier, especially with complex family histories or unclear mutations.
Genetic counselors are key in explaining your test results. They talk about the risks and what it means for planning your family. They also help with managing the condition during pregnancy.
Psychological Impact of Carrier Status
Being told you carry the hemophilia gene can be tough on your mind. You might feel anxious, guilty, or unsure about your future and the risks to your kids. Support systems, like genetic counseling and psychological help, are crucial for coping.
Don’t forget the importance of support groups and educational resources. They provide carriers with the info and community they need to deal with their carrier status.
Prenatal Testing for Hemophilia
Expectant parents who carry hemophilia need to know about prenatal testing. These tests can tell if the fetus has the condition. This helps parents decide what to do next.
Non-Invasive Prenatal Testing Options
Non-invasive prenatal testing (NIPT) looks at the mother’s blood for DNA signs of hemophilia in the fetus. It’s less risky than other tests but might not always be right.
NIPT can start as early as 10 weeks. It’s mainly for checking for chromosomal issues. But, some tests can spot genetic changes linked to hemophilia.
Invasive Testing Procedures
Invasive tests like chorionic villus sampling (CVS) and amniocentesis take a sample from the fetus. CVS is done between 10 and 13 weeks. Amniocentesis is after 15 weeks.
These tests have a small risk of complications, like miscarriage. But, they can definitely say if the fetus has hemophilia.
Timing of Prenatal Diagnosis
The timing of prenatal tests varies. Non-invasive tests can start earlier. Invasive tests are later. Knowing this is key for parents.
Ethical Considerations
Prenatal testing for hemophilia brings up big ethical questions. Parents must think about the benefits and risks of testing. They also face a tough choice about continuing or ending the pregnancy.
It’s vital for families to get full counseling. This helps them make these hard decisions.
Treatment Options During Hemophilia Pregnancy
Hemophilia treatment during pregnancy is a complex process. It aims to keep both mother and baby healthy. It’s vital to manage hemophilia well to avoid problems during pregnancy and childbirth.
Factor Replacement Therapy
Factor replacement therapy is key in managing hemophilia during pregnancy. It replaces the missing clotting factor to help blood clot normally. The goal is to keep enough factor levels to prevent bleeding.
- Benefits: Reduces the risk of bleeding during pregnancy and childbirth.
- Considerations: Requires regular monitoring of clotting factor levels and adjustment of doses as needed.
Desmopressin (DDAVP) Use
Desmopressin, or DDAVP, is used for mild hemophilia A. It boosts the levels of factor VIII and von Willebrand factor in the blood.
Key considerations for DDAVP use during pregnancy include:
- Monitoring for potential side effects such as hyponatremia.
- Assessing the patient’s response to DDAVP to ensure efficacy.
Monitoring Clotting Factor Levels
It’s crucial to regularly check clotting factor levels during pregnancy. This ensures treatment is working and makes any needed changes. It helps prevent bleeding and clotting problems.
Managing Other Bleeding Disorders in Pregnancy
Women with bleeding disorders like von Willebrand disease or factor XI deficiency need special care in pregnancy. Treatment plans may include factor replacement therapy, DDAVP, or other specific treatments.
Key aspects of managing other bleeding disorders include:
- Accurate diagnosis of the bleeding disorder.
- Development of a personalized treatment plan.
- Close collaboration between hematologists and obstetricians.
Creating a Comprehensive Birth Plan
Women with hemophilia need a detailed birth plan for a safe delivery. A good plan manages bleeding disorder challenges during pregnancy and birth.
Assembling a Specialized Medical Team
It’s key to have a team of experts in hemophilia and pregnancy. This team should include doctors and specialists for full care.
This team will make a care plan for you, watch your pregnancy, and handle any issues. Choose doctors with bleeding disorder experience for the best care.
Hospital Selection Considerations
Choosing a hospital for high-risk pregnancies and hemophilia care is important. The hospital should have a hematology department and the right treatments.
Look for a hospital with 24/7 hematology services, a specialized treatment center, and experience with bleeding disorders during birth.
| Hospital Feature | Importance | Considerations |
| 24/7 Hematology Services | High | Ensures immediate care for bleeding complications |
| Hemophilia Treatment Center | High | Provides specialized care and treatment options |
| Experience with Bleeding Disorders | High | Indicates familiarity with managing hemophilia during delivery |
Emergency Protocols
Having emergency plans is crucial for a birth plan. This includes steps for bleeding emergencies during delivery.
The emergency plan should cover how to handle bleeding emergencies. This includes using clotting factor concentrates and other treatments.
Communication with Healthcare Providers
Talking well with healthcare providers is key. This ensures your birth plan is followed. Discuss your plan with the team and make sure all info is documented.
Delivery Options for Women with Hemophilia
Women with hemophilia need to know their delivery options. This helps them make the best choice for their health and their baby’s. The decision between vaginal birth and cesarean section depends on many factors.
Vaginal Birth Considerations
Vaginal birth is possible for women with hemophilia. But, it needs careful planning. Factor replacement therapy might be needed to control bleeding risks. Always talk to a healthcare provider who knows about hemophilia before making a decision.
Cesarean Section Considerations
Women with hemophilia might choose a cesarean section. This is especially true if the baby’s health is at risk or if pregnancy complications arise. It’s important to have coordinated care from both obstetricians and hematologists to reduce surgery risks.
Anesthesia Options and Risks
Choosing the right anesthesia is crucial. Healthcare providers should discuss the options with you. Regional anesthesia, like epidural or spinal, might be used with caution due to bleeding risks. Close monitoring is key to handle any issues.
Preventing Maternal Hemorrhage
Stopping maternal hemorrhage is key during delivery for women with hemophilia. This can be done with factor replacement therapy and uterotonic agents to help the uterus contract. Having a detailed birth plan is important to prepare for any bleeding issues.
| Delivery Option | Key Considerations | Risk Management Strategies |
| Vaginal Birth | Factor replacement therapy, careful monitoring | Factor VIII or IX replacement, close monitoring of bleeding |
| Cesarean Section | Coordinated care between specialists, surgical risks | Preoperative factor replacement, postoperative monitoring |
| Anesthesia | Regional anesthesia risks, alternative options | Careful selection of anesthesia type, monitoring for bleeding complications |
Special Considerations for Newborns with Hemophilia
Hemophilia in newborns brings unique challenges. Healthcare providers and parents must be ready to face these challenges. It’s important to know the special needs and possible complications.
Immediate Post-Birth Testing
For families with a known history of hemophilia, prenatal testing can offer insights. But, even without prior knowledge, immediate post-birth testing is crucial. This usually involves a blood test to check clotting factor levels in the newborn.
Clotting factor assays are key tests for diagnosing hemophilia in newborns. They measure factor VIII (8) for Hemophilia A or factor IX (9) for Hemophilia B in the blood.
Preventing Birth-Related Bleeding
Newborns with hemophilia face bleeding risks, especially after birth. It’s vital to prevent birth-related bleeding. This might include giving clotting factor concentrates soon after birth, especially if there’s a risk of bleeding.
| Procedure | Purpose | Timing |
| Clotting factor assay | Diagnose hemophilia | Immediately after birth |
| Administration of clotting factor concentrates | Prevent or treat bleeding | As needed, based on clinical assessment |
Initial Treatment Approaches
The first treatment for newborns with hemophilia aims to prevent and manage bleeding. This usually involves factor replacement therapy. It replaces the missing clotting factor to help normal clotting.
Parents should team up with their healthcare team to create a detailed treatment plan. This plan will include checking clotting factor levels, preventing injuries, and managing bleeding episodes.
Postpartum Care for Mothers with Bleeding Disorders
The postpartum period is tough for women with bleeding disorders. They need special care to avoid problems and recover well.
Managing Postpartum Bleeding Risks
Women with bleeding disorders face a higher risk of postpartum hemorrhage (PPH). Effective management involves watching bleeding closely, using clotting factor concentrates when needed, and uterotonic agents to help the uterus contract.
A team of doctors, including obstetricians and hematologists, should work together. They help figure out the risk of PPH and plan how to reduce it.
| Risk Factor | Management Strategy |
| History of PPH | Prophylactic administration of clotting factor concentrates |
| Low fibrinogen levels | Fibrinogen replacement therapy |
| Multiple pregnancy | Close monitoring and preparation for potential hemorrhage |
Recovery Timeline and Expectations
Recovery for women with bleeding disorders takes longer and is more complex. It’s essential for patients to understand the recovery timeline and what to expect.
- Immediate postpartum period: Close monitoring in a hospital setting.
- First few weeks: Gradual recovery, with ongoing assessment of bleeding risks.
- Follow-up appointments: Regular check-ups with healthcare providers to monitor recovery and adjust treatment plans as necessary.
Follow-Up Care Requirements
Follow-up care is key for managing the long-term health of women with bleeding disorders post-pregnancy. This includes:
- Regular hematologic assessments to monitor clotting factor levels.
- Adjustments to treatment plans based on the patient’s condition and recovery progress.
- Emotional support and counseling to address any psychological impacts of the pregnancy and postpartum experience.
Breastfeeding Considerations
Breastfeeding is often encouraged for women with bleeding disorders. Benefits include improved uterine contraction and potential reduction in bleeding risk. However, the decision to breastfeed should be made in consultation with healthcare providers, taking into account the individual’s overall health and specific condition.
By understanding the unique challenges and implementing appropriate care strategies, women with bleeding disorders can navigate the postpartum period more safely and effectively.
Other Bleeding Disorders and Pregnancy
It’s important to know about bleeding disorders other than hemophilia when managing pregnancy. These conditions can also affect pregnancy and need special care.
Von Willebrand Disease
Von Willebrand disease (VWD) is the most common inherited bleeding disorder. It affects both men and women. It’s caused by a lack or problem with von Willebrand factor (VWF), a key clotting protein.
During pregnancy, VWF levels usually go up. This can sometimes hide the symptoms of VWD. But, the risk of bleeding is still there, especially during delivery and after.
Managing VWD during pregnancy means keeping an eye on VWF and factor VIII levels. Sometimes, desmopressin is used to help release VWF. But, how well it works can vary based on the type of VWD.
- Regular monitoring of VWF and factor VIII levels
- Use of desmopressin or VWF concentrates as needed
- Planning for delivery with a multidisciplinary team
Factor XI Deficiency
Factor XI deficiency is another bleeding disorder that can make pregnancy tricky. It’s caused by a lack of factor XI, a protein needed for blood clotting. It’s more common in people of Ashkenazi Jewish descent.
Management strategies for factor XI deficiency during pregnancy include:
- Assessing the risk of bleeding based on factor XI levels
- Using fresh frozen plasma or factor XI concentrate to manage bleeding risks
- Coordinating with a hematologist and obstetrician for delivery planning
Rare Clotting Factor Deficiencies
Rare clotting factor deficiencies, like deficiencies in factors II, V, VII, X, or XIII, can also affect pregnancy. These conditions are often inherited and can lead to serious bleeding problems.
The management of rare clotting factor deficiencies involves:
- Specific factor replacement therapy
- Close monitoring for signs of bleeding
- Multidisciplinary care for delivery and postpartum management
Platelet Function Disorders
Platelet function disorders are conditions where platelets don’t work right, leading to poor blood clotting. These can be inherited or acquired and can complicate pregnancy.
Management approaches include:
- Assessing platelet function through laboratory tests
- Using platelet transfusions or other therapies as needed
- Planning for potential bleeding complications during delivery
In conclusion, managing pregnancy with bleeding disorders other than hemophilia needs a detailed and team-based approach. Understanding the specific risks and how to manage them helps ensure a safe and healthy pregnancy for both mom and baby.
Living with Hemophilia: Resources for New Parents
As a new parent to a child with hemophilia, finding the right support is key. Hemophilia makes it hard for blood to clot. Luckily, many resources are out there to help families.
Support Groups and Organizations
Support groups and organizations offer emotional support and guidance. The National Hemophilia Foundation is a big help. They have local groups and educational materials. Joining these groups can connect families with others who face similar challenges.
Educational Materials
Understanding hemophilia is crucial. Sources like the World Federation of Hemophilia and PubMed offer insights into treatments. These resources help parents make informed decisions for their child’s care.
Financial Assistance Programs
Dealing with hemophilia can be expensive. But, there are financial help programs out there. Organizations like the National Hemophilia Foundation’s HELP program offer financial support for families.
Connecting with Other Hemophilia Families
Meeting other families with children with hemophilia can be very helpful. Organizations help connect families through events and online forums. Sharing experiences and advice can be very beneficial.
In conclusion, while hemophilia is challenging, there are many resources to help. Support groups, educational materials, financial help, and connections with other families can make a big difference. With these resources, parents can give their children the best care possible.
Conclusion: Navigating Hemophilia and Motherhood
Managing hemophilia and motherhood needs careful planning and support. Women with hemophilia or carriers must know the risks of pregnancy. This knowledge is key to a safe pregnancy.
It’s vital to work with a specialized medical team. They help ensure the best health for both mom and baby. Close monitoring is crucial during pregnancy.
Understanding hemophilia and motherhood helps women make smart health choices. This approach lets them handle pregnancy with confidence. It’s all about getting the right care.
With the right support, women with hemophilia can have a healthy pregnancy. They can also enjoy a positive motherhood experience.
FAQ
What is hemophilia?
Hemophilia is a genetic disorder. It makes it hard for the body to make blood clots. Blood clots are needed to stop bleeding.
Can women have hemophilia?
Yes, women can have hemophilia. It’s more common in males. But, females can carry the gene and sometimes be affected by it.
How is hemophilia inherited?
Hemophilia is inherited in an X-linked recessive pattern. This means the genes are on the X chromosome.
What are the risks associated with hemophilia during pregnancy?
Pregnant women with hemophilia or who carry the gene face bleeding risks. There’s also a chance their child could inherit it.
What prenatal testing options are available for hemophilia?
Tests include ultrasound and invasive methods like amniocentesis or CVS. These tests check if the fetus has hemophilia.
How is hemophilia managed during pregnancy?
Management includes factor replacement therapy and monitoring clotting factor levels. Desmopressin may also be used to increase factor VIII levels.
What considerations are there for delivery in women with hemophilia?
Delivery planning is crucial. It should consider bleeding risks and the baby’s chance of having hemophilia. Options include vaginal delivery or cesarean section.
Can hemophilia affect the newborn?
Yes, newborns with hemophilia need immediate testing and treatment. This is to prevent bleeding, especially after birth-related injuries.
What postpartum care is necessary for mothers with bleeding disorders?
Postpartum care includes managing bleeding risks and monitoring for postpartum hemorrhage. A recovery plan with follow-up care is also important.
Are there resources available for families dealing with hemophilia?
Yes, there are support groups, educational materials, and financial assistance programs. They help families manage hemophilia.
How does being a carrier of hemophilia affect a woman?
Being a carrier can have psychological implications. There’s also a risk of passing the condition to offspring. Genetic counseling is important.
What is genetic counseling for hemophilia?
Genetic counseling provides information on passing hemophilia to children. It discusses testing options and helps with family planning decisions.
What other bleeding disorders can impact pregnancy?
Bleeding disorders like von Willebrand disease, factor XI deficiency, and platelet function disorders can also affect pregnancy. They require specialized care.