Last Updated on October 21, 2025 by mcelik

About 100,000 people in the United States have sickle cell disease. It’s a chronic blood condition with deep genetic roots. We’re going to look into its genetic aspects to fully grasp its impact.
It’s important to know if sickle cell anemia genetic factors play a role in the disease. This knowledge is key for those affected and their families. The genetic basis of sickle cell disease shows how it’s passed down and the risks for carriers.
We’ll explore the genetic side to shed light on inheritance patterns and family implications. Knowing this is crucial for managing the condition well.
Key Takeaways
- Sickle cell disease is a genetic disorder affecting hemoglobin production.
- The condition is inherited in an autosomal recessive pattern.
- Carriers of the sickle cell trait are generally healthy but can pass the mutated gene to their offspring.
- Understanding the genetic basis helps in family planning and risk assessment.
- Genetic counseling is recommended for families with a history of sickle cell disease.
What Is Sickle Cell Disease?
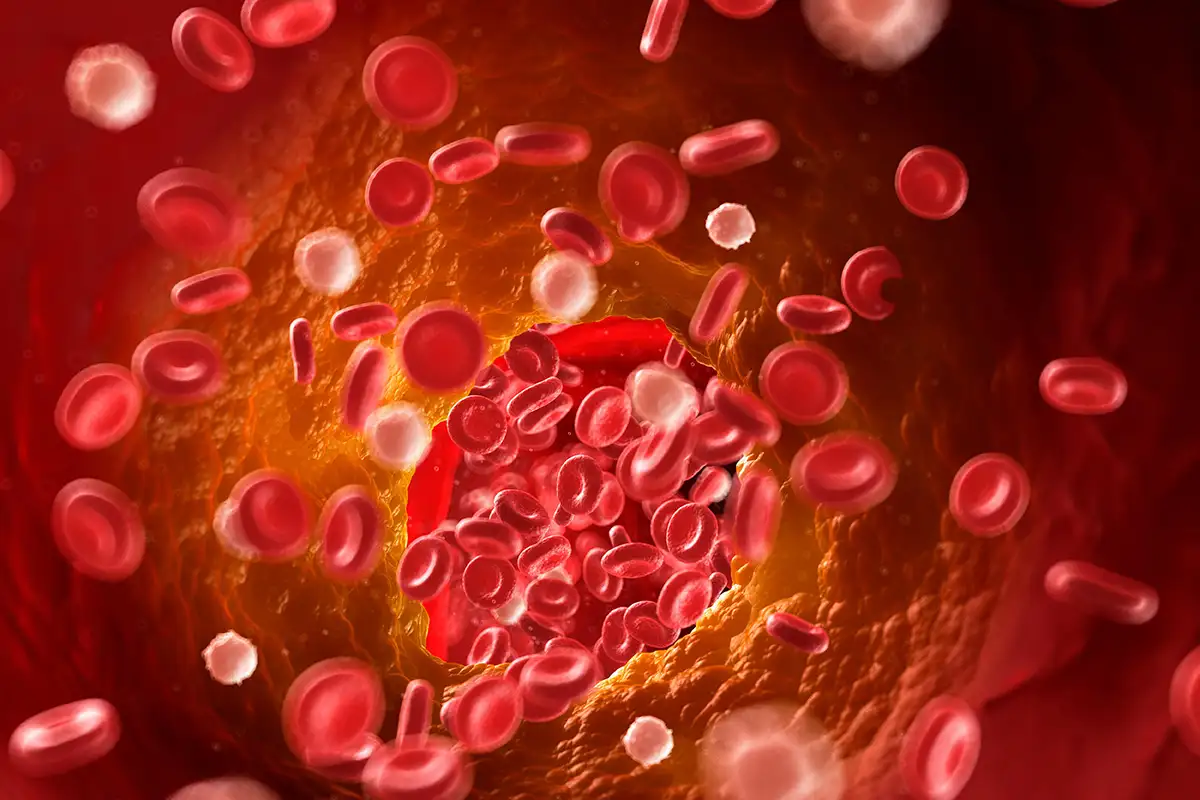
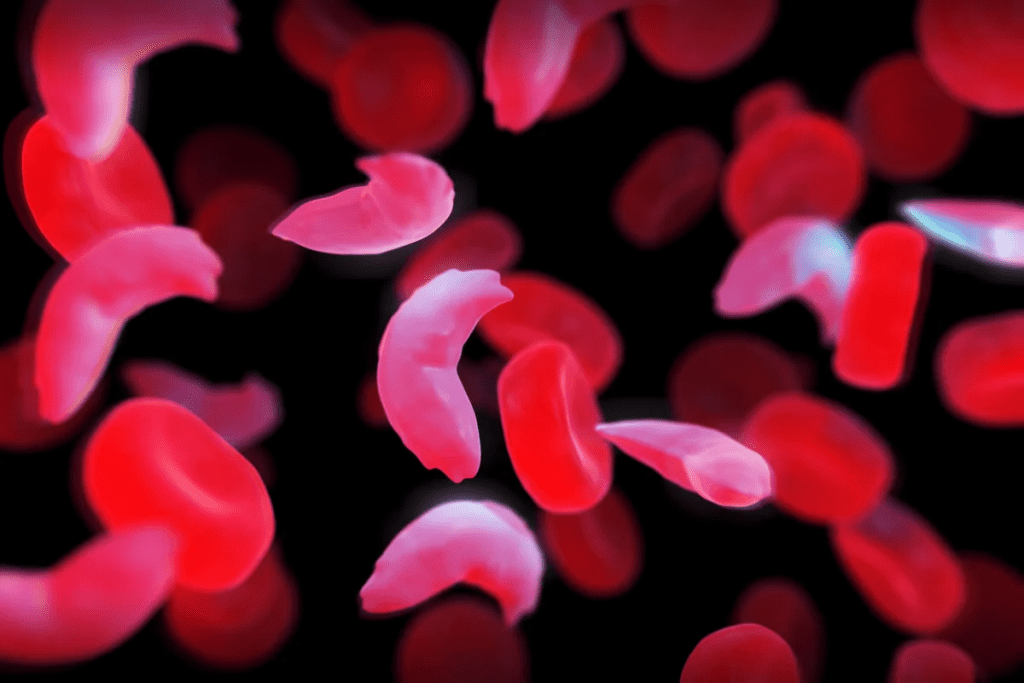
Sickle cell disease is a genetic condition that changes how hemoglobin works in red blood cells. This change makes red blood cells sickle-shaped, a key sign of the disease.
Definition and Basic Characteristics
Sickle cell disease affects hemoglobin, a protein in red blood cells. It’s a group of disorders that alter hemoglobin’s function. This leads to the creation of sickle hemoglobin or hemoglobin S.
This abnormal hemoglobin causes red blood cells to become sickle-shaped. This shape makes them more likely to break down and get stuck in blood vessels.
How Sickle-Shaped Cells Affect the Body
Sickle-shaped red blood cells can harm the body in many ways. They are more fragile and break down easily, causing anemia. These cells can also block small blood vessels, leading to pain and tissue damage.
“Sickle cell disease is a significant public health issue worldwide, affecting millions of people. Understanding its genetic basis is crucial for developing effective management strategies.”
Primary Symptoms and Complications
Symptoms of sickle cell disease vary from person to person. Common signs include pain episodes, anemia, swelling, frequent infections, and delayed growth in children. Serious complications include stroke, acute chest syndrome, and splenic sequestration.
| Symptom/Complication | Description |
| Pain Crises | Episodes of pain due to vaso-occlusion by sickled red blood cells. |
| Anemia | Reduced number of red blood cells due to hemolysis. |
| Acute Chest Syndrome | A life-threatening condition characterized by a new pulmonary infiltrate on chest radiograph. |
Is Sickle Cell Disease Genetic? The Definitive Answer
Sickle cell disease is a genetic condition. Knowing it’s hereditary is key for families dealing with it. This knowledge helps in managing the disease and making family planning decisions.
The Hereditary Nature of Sickle Cell Disease
Sickle cell disease comes from a mutation in the HBB gene. This gene codes for a part of hemoglobin. The mutation causes abnormal hemoglobin, known as sickle hemoglobin or HbS.
The disease follows an autosomal recessive pattern. This means a person needs two copies of the mutated HBB gene to have the disease. One copy comes from each parent.
Because of its hereditary nature, sickle cell disease often appears in families. If both parents carry the mutated gene, there’s a 25% chance their child will have the disease. There’s also a 50% chance the child will be a carrier like the parents. And a 25% chance the child won’t have the disease or be a carrier.
Key Points About Inheritance:
- Autosomal recessive inheritance pattern
- Both parents must be carriers for a child to be at risk
- 25% chance of having a child with sickle cell disease if both parents are carriers
Why Sickle Cell Is Not Contagious
Sickle cell disease is not contagious. It’s not spread through contact or exposure. It’s caused by genetic inheritance, not by bacteria or viruses.
Born With the Condition: Genetic Presence at Birth
People are born with sickle cell disease because of a genetic mutation. This mutation is present at birth. Newborn screening programs can detect it through a blood test.
Early diagnosis is vital for managing sickle cell disease. It allows for early treatment. This can prevent complications and improve life quality for those with the disease.
Key Facts About Sickle Cell Disease at Birth:
- Genetic mutation is present at birth
- Newborn screening programs can diagnose the condition early
- Early diagnosis enables timely medical interventions
Sickle Cell Anemia Genetics: Understanding the Mutation
Sickle cell anemia comes from a genetic change in the HBB gene. This change affects how hemoglobin is made. It leads to abnormal hemoglobin, called sickle hemoglobin or hemoglobin S.
The HBB Gene and Its Normal Function
The HBB gene tells our bodies how to make beta-globin. Beta-globin is key for hemoglobin, which carries oxygen. Without it, our bodies can’t get oxygen where it’s needed.
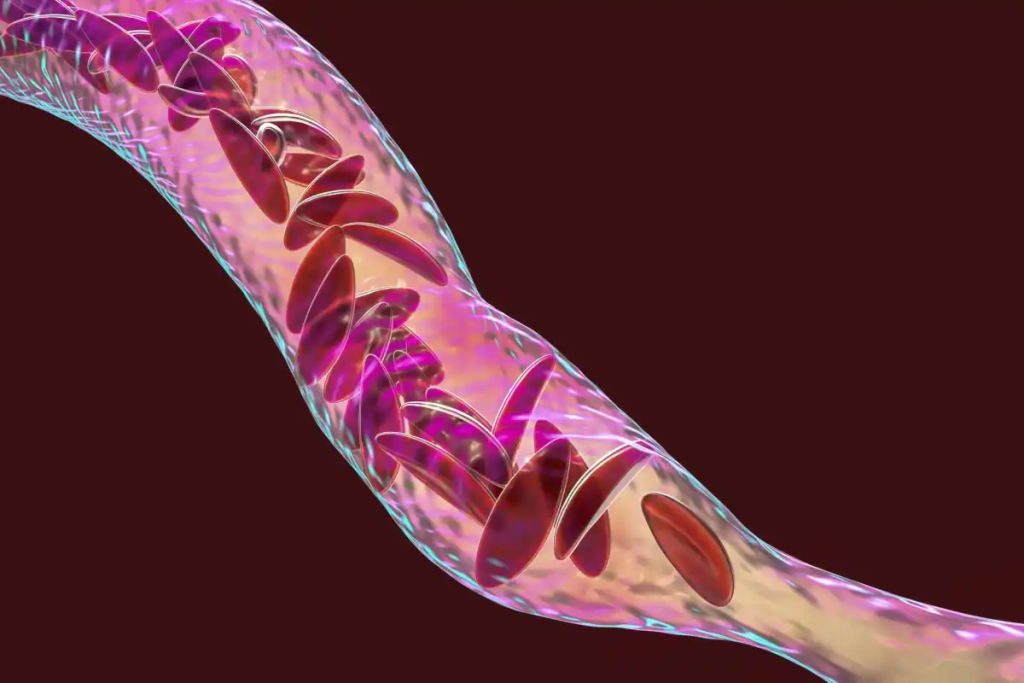
How the Genetic Mutation Affects Hemoglobin
The HBB gene mutation makes abnormal beta-globin, or hemoglobin S. When it gets cold or dehydrated, hemoglobin S can change shape. This makes red blood cells stiff and sickle-shaped, a key sign of sickle cell anemia.
The Molecular Basis of Sickling
Sickling happens when deoxygenated hemoglobin S sticks together. This makes red blood cells sickle-shaped. This shape change is bad for the cells and can cause damage.
Knowing how sickle cell anemia works helps us find better treatments. It’s important for managing the disease.
Inheritance Pattern for Sickle Cell Disease
Sickle cell disease follows an autosomal recessive model. This means it’s not linked to sex chromosomes. A person needs two defective copies of the HBB gene, one from each parent, to have the disease.
Autosomal Recessive Inheritance Explained
For autosomal recessive inheritance, both parents must carry the mutated gene. With each pregnancy, there’s a 25% chance the child will have sickle cell disease. There’s also a 50% chance the child will be a carrier like their parents. And a 25% chance the child won’t inherit the mutated gene.
Carrier Status and Sickle Cell Trait
Being a carrier means having one normal and one mutated HBB gene. Carriers usually don’t show full symptoms but can pass the mutated gene to their kids. They might face health issues under extreme conditions.
Probability Charts for Parents and Children
Knowing the chances of passing on sickle cell disease or the trait is key for family planning. The risk depends on the parents’ genotypes. Here’s a table showing possible genotypes and phenotypes of offspring when both parents are carriers:
| Genotype of Offspring | Probability | Phenotype of Offspring |
| Normal HBB gene from both parents | 25% | Not affected, not a carrier |
| One mutated HBB gene from one parent and one normal HBB gene from the other | 50% | Carrier, not affected |
| Mutated HBB gene from both parents | 25% | Affected by sickle cell disease |
Genetic counseling offers detailed info and support to families with sickle cell disease. It helps them understand their risks and make informed choices.
What Causes Sickle Cell Anemia at the Genetic Level
Sickle cell anemia starts with a single change in a gene. This change affects the HBB gene. It’s responsible for making a part of hemoglobin.
The Single Nucleotide Substitution
A single change in the HBB gene leads to sickle hemoglobin, or HbS. This happens when glutamic acid is swapped with valine at the sixth spot of the beta-globin chain.
This change comes from a DNA sequence shift from GAG to GTG. It makes hemoglobin stick together when there’s not enough oxygen. This causes red blood cells to curve, a sign of sickle cell anemia.
Different Types of Hemoglobin Mutations
While HbS is the main cause, other mutations can also lead to sickle cell anemia. These include:
| Hemoglobin Mutation | Description | Effect |
| HbS | Sickle hemoglobin | Causes sickling of red blood cells |
| HbC | Abnormal hemoglobin with glutamic acid to lysine substitution | Mild hemolytic anemia |
| HbE | Abnormal hemoglobin with glutamic acid to lysine substitution | Mild hemolytic anemia |
Genetic Triggers and Environmental Factors
Genetic changes are the main cause, but the environment can also play a role. Factors include:
- Low oxygen levels
- Dehydration
- Infections
- High altitude
Knowing about these factors helps in managing the disease. It also aids in finding new treatments.
Common Misconceptions About How Sickle Cell Disease Is Inherited
Sickle cell disease inheritance is often misunderstood, leading to unnecessary fear and stigma. We aim to clarify the facts and dispel common myths surrounding the inheritance of this genetic condition.
Myths About Sickle Cell Transmission
One of the most pervasive myths is that sickle cell disease is contagious, that it can be “caught” from someone who has it. This is entirely false; sickle cell disease is a genetic disorder that is inherited from one’s parents.
Clarifying Dominant vs. Recessive Inheritance
Sickle cell disease is inherited in an autosomal recessive pattern. This means that for a child to have the disease, they must inherit two defective hemoglobin genes”one from each parent. We often get asked if having one sickle cell gene (being a carrier) means you’ll develop the disease. The answer is no; carriers typically do not display the full symptoms of the disease but can pass the gene to their offspring.
Who Can and Cannot Develop Sickle Cell Disease
Anyone can be a carrier of the sickle cell gene, but the disease primarily affects individuals of African, Caribbean, and Middle Eastern descent. To develop sickle cell disease, an individual must inherit two copies of the mutated gene. Carriers, who have one normal and one mutated gene, are generally healthy but can pass the mutated gene to their children.
| Parent 1 Status | Parent 2 Status | Child’s Risk of Sickle Cell Disease | Child’s Risk of Being a Carrier |
| Carrier | Carrier | 25% | 50% |
| Carrier | Not a Carrier | 0% | 50% |
| Affected | Carrier | 50% | 50% |
| Affected | Affected | 100% | 0% |
By understanding the genetic basis of sickle cell disease and how it’s inherited, we can work to reduce misconceptions and support those affected by the condition.
Who Gets Sickle Cell Disease? Population Genetics
To understand who gets sickle cell disease, we need to look at its genetics and where it’s found. It’s not spread out evenly around the world. It’s more common in certain places and among certain groups.
Geographic Distribution and Affected Populations
Sickle cell disease is common in warm and tropical areas, especially where malaria is or was common. This includes parts of Africa, the Middle East, India, and the Mediterranean. In the U.S., it’s more common among African Americans and some Hispanic Americans.
The disease’s spread is tied to how people moved and malaria’s history. For example, in West Africa, the sickle cell trait is common because it helps fight malaria.
The Evolutionary Advantage Against Malaria
The sickle cell trait helps protect against severe malaria. People with one copy of the mutated gene are more likely to survive malaria. This means they can pass on their genes, making the trait more common in malaria areas.
Studies show the sickle cell trait can cut malaria risk by up to 90% in kids. This is why it’s so common in places where malaria is a big problem.
Prevalence Statistics in the United States
In the U.S., sickle cell disease is a big issue, especially in the African American community. The CDC says it affects about 1 in 365 African American births. It affects about 1 in 16,300 Hispanic American births.
| Ethnic Group | Incidence of Sickle Cell Disease |
| African American | 1 in 365 births |
| Hispanic American | 1 in 16,300 births |
These numbers show why we need to be aware and screen for sickle cell disease, especially in high-risk communities.
Diagnosing the Genetic Basis of Sickle Cell Disease
Understanding sickle cell disease’s genetic roots is key to diagnosing it. Diagnosing this disease requires genetic tests and clinical checks. These steps help identify the disease and its severity.
Prenatal Testing Options
Prenatal tests for sickle cell disease are available. They give expectant parents vital information. These tests show if the fetus has the sickle cell gene.
The main prenatal tests are:
- Chorionic villus sampling (CVS)
- Amniocentesis
Both tests have a small risk but offer important genetic insights.
| Prenatal Test | Description | Gestational Age |
| Chorionic Villus Sampling (CVS) | Involves removing a sample of cells from the placenta | 10-12 weeks |
| Amniocentesis | Involves withdrawing a sample of amniotic fluid | 15-20 weeks |
Newborn Screening Programs
Newborn screening for sickle cell disease is vital. Most countries screen for it soon after birth. This early check helps manage the disease.
Early screening benefits include:
- Early intervention to prevent complications
- Education for families on managing the condition
- Monitoring for potential complications
Genetic Testing for Adults and Family Members
Genetic testing is not just for newborns and fetuses. It’s also for adults and family members. This testing helps find carriers or those with the disease.
Genetic testing for adults offers:
- Determining carrier status
- Assessing the risk of passing the condition to offspring
- Informing family planning decisions
Knowing the genetic basis of sickle cell disease helps individuals and families. It aids in making health and reproductive choices.
Genetic Counseling for Families Affected by Sickle Cell
Genetic counseling is key for families dealing with sickle cell disease. It helps them understand the genetic side of things. This knowledge is vital for making health and family planning decisions.
When to Seek Genetic Counseling
If you have sickle cell disease or trait in your family, get genetic counseling. It’s especially important if you’re planning a family or are already pregnant. Counseling can show you the risks of passing on the condition to your kids.
It’s best to get counseling early, before pregnancy. This way, you can make informed choices. It can also lower the chance of having a child with sickle cell disease.
What to Expect During Counseling Sessions
Genetic counseling talks about your medical history and sickle cell disease. You’ll learn about the risks of passing it to your kids. Counselors explain this complex info in simple terms.
A trained genetic counselor will lead the session. They’ll answer your questions and guide you on managing the condition.
| Aspect | Description |
| Medical History Review | A detailed review of the family’s medical history to identify any instances of sickle cell disease or trait. |
| Genetic Basis Explanation | An explanation of how sickle cell disease is inherited and the genetic factors involved. |
| Risk Assessment | An assessment of the risks associated with passing on the condition to children. |
Family Planning with Sickle Cell Genetics
Genetic counseling is crucial for family planning. It helps families understand genetic risks. This knowledge is key for making choices about pregnancy, like prenatal testing.
We support families with the info they need. Our goal is to help them understand sickle cell genetics. This way, they can make the best decisions for their family.
The Relationship Between Genetics and Symptom Severity
Understanding sickle cell disease’s genetic basis helps explain why symptoms vary. The condition’s impact on people can differ a lot. Genetics play a big role in this difference.
Genetic Modifiers of Sickle Cell Disease
Genetic modifiers are genes that can change how sickle cell disease affects people. They can make symptoms better or worse. This depends on their type and how they work with the HBB gene mutation.
Key genetic modifiers include genes that affect hemoglobin production and fetal hemoglobin levels. For example, more fetal hemoglobin can make the disease less severe.
Why Symptoms Vary Between Individuals
Several genetic factors cause the difference in symptom severity among sickle cell disease patients. These include genetic modifiers, other inherited conditions, and genetic variations. These factors affect how the disease is expressed.
For instance, having other genetic conditions can change how sickle cell disease is experienced. Alpha-thalassemia, for example, can make the disease less severe by lowering hemoglobin S levels.
Co-inheritance of Other Genetic Conditions
Having other genetic conditions can greatly affect the severity and how sickle cell disease is seen. It’s important to understand these interactions to manage the disease well.
| Co-inherited Condition | Effect on Sickle Cell Disease |
| Alpha-thalassemia | Can reduce disease severity by decreasing hemoglobin S concentration. |
| High Fetal Hemoglobin | Generally associated with milder disease symptoms. |
| G6PD Deficiency | Can increase the risk of certain complications, such as hemolysis. |
Current Research in Sickle Cell Genetics
The study of sickle cell genetics is moving fast. New research is uncovering how sickle cell disease works. This knowledge is leading to new ways to treat it.
Gene Therapy Approaches
Gene therapy is a big deal in sickle cell disease research. It aims to fix the genetic problem causing the disease. Scientists are using gene editing technologies to change the HBB gene in sickle cell patients.
“Gene therapy could be a cure for sickle cell disease,” studies say. Clinical trials are checking if it’s safe and works well.
CRISPR and Genetic Editing Potential
The CRISPR/Cas9 system is changing genetic editing. It lets scientists edit genes with great precision. CRISPR/Cas9 is being tested in studies, showing it might help treat sickle cell disease.
“The advent of CRISPR/Cas9 has opened new avenues for treating genetic diseases like sickle cell anemia,” – A leading researcher in the field.
Breakthrough Studies and Clinical Trials
Many studies and trials are happening now. They’re looking into gene therapy, genetic editing, and new treatments. These include tests on gene therapy, CRISPR/Cas9, and genetic changes.
- Clinical trials assessing gene therapy safety and efficacy
- Studies on CRISPR/Cas9 editing in human cells
- Research into genetic modifiers of sickle cell disease
As research goes on, we’ll see better treatments. This could change how we manage sickle cell disease.
The Future of Genetic Treatments for Sickle Cell Disease
New genetic treatments bring hope for sickle cell disease patients. Research is moving towards more precise and powerful therapies.
Emerging Therapies Targeting Genetic Causes
New treatments aim to fix sickle cell disease’s genetic cause. Gene editing, like CRISPR/Cas9, shows great promise in fixing the faulty gene.
Gene Therapy Approaches: Gene therapy tries to fix sickle cell by changing or replacing the HBB gene. It uses viruses to carry a healthy gene to cells.
Personalized Medicine Approaches
Personalized medicine is key in treating sickle cell disease. It tailors treatments to each person’s genes, making care more effective.
Tailoring Treatment: This method looks at each patient’s unique genetic makeup. It helps predict how severe the disease will be and how well treatments will work.
Timeline for New Genetic Treatments
It’s hard to say when new treatments will arrive. But, many are in late-stage trials. We expect some to be approved in the next few years.
| Therapy Type | Current Stage | Expected Timeline |
| Gene Editing | Clinical Trials | 2025-2030 |
| Gene Therapy | Advanced Clinical Trials | 2026-2032 |
| Personalized Medicine | Early Adoption | 2024-2028 |
The future for sickle cell disease treatments looks bright. With new therapies coming, we’re optimistic about better lives for those affected.
Conclusion: Living with a Genetic Condition
We’ve looked into the genetic roots of sickle cell disease. It’s a condition passed down through genes, affecting both individuals and their families. To manage it, a full care plan is needed, from genetic advice to new treatments.
Dealing with sickle cell disease means more than just medical care. It also involves changing your lifestyle and getting emotional support. Knowing the genetic side of the disease helps people make better choices for their health.
In the end, sickle cell disease is a tough genetic issue, but research and new treatments bring hope. We urge those dealing with the disease to keep up with the latest news. Seek help from doctors and support groups too.
FAQ
Is sickle cell disease genetic?
Yes, sickle cell disease is caused by a gene mutation. This mutation is in the HBB gene, which codes for hemoglobin.
How is sickle cell disease inherited?
Sickle cell disease is inherited in a specific way. A person needs two copies of the mutated HBB gene, one from each parent, to have the disease.
What is the difference between sickle cell trait and sickle cell disease?
Sickle cell trait happens when a person has one normal and one mutated HBB gene. Sickle cell disease occurs when a person has two mutated genes.
Can sickle cell disease be contagious?
No, sickle cell disease is not contagious. It cannot spread from one person to another.
Are people born with sickle cell disease?
Yes, sickle cell disease is present at birth. It is a genetic condition that people are born with.
How does genetic mutation affect hemoglobin?
The mutation in the HBB gene leads to abnormal hemoglobin. This abnormal hemoglobin, known as sickle hemoglobin or HbS, causes red blood cells to become sickle-shaped.
What is the molecular basis of sickling?
Sickling happens when sickle hemoglobin polymerizes under low oxygen conditions. This causes red blood cells to deform into a sickle shape.
Can genetic testing diagnose sickle cell disease?
Yes, genetic testing can identify the HBB gene mutation. This is how sickle cell disease is diagnosed.
What is the role of genetic counseling in sickle cell disease?
Genetic counseling helps families understand sickle cell disease risks. It aids in making informed reproductive decisions and managing the condition.
Are there any new treatments for sickle cell disease based on genetic research?
Yes, genetic research has led to new treatments. These include gene therapy and CRISPR/Cas9 gene editing, which are being tested in clinical trials.
How do genetic modifiers affect the severity of sickle cell disease?
Genetic modifiers can change how severe sickle cell disease is. They affect the HBB gene or other genes involved in the disease.
Can co-inheritance of other genetic conditions affect sickle cell disease?
Yes, having other genetic conditions can change how sickle cell disease presents. It can also affect its severity.
References
- National Human Genome Research Institute. (2024). Sickle cell disease: Genetic basis and inheritance. National Institutes of Health. Retrieved from https://www.genome.gov/Genetic-Disorders/Sickle-Cell-Disease