About 100,000 people in the United States live with sickle cell disease. This condition causes severe pain because of red blood cells that don’t shape right.Learn about sickle cell anemia symptoms and why the disease is painful, including common pain episodes and ways to manage discomfort effectively.
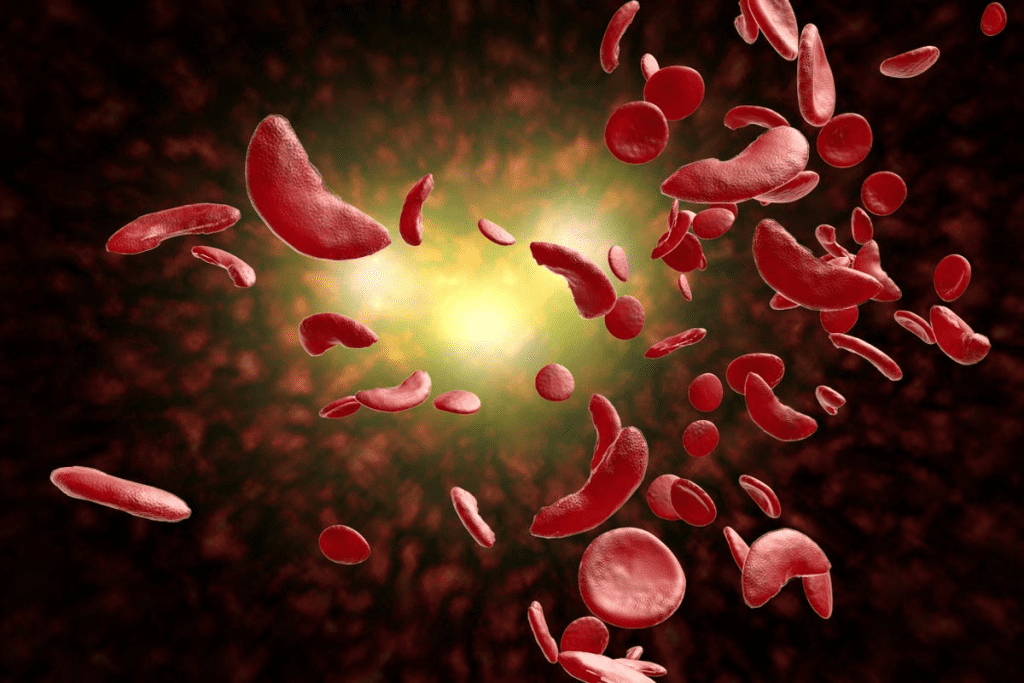
Sickle cell anemia is a big health problem. It happens when red blood cells have abnormal hemoglobin. This leads to many health issues. The pain from this condition can be very bad and last a long time, making life hard.
The signs of sickle cell anemia can differ from person to person. But, many people have pain episodes, or crises. These can start from things like not drinking enough water, feeling stressed, or being in very hot or cold places.
Key Takeaways
- Sickle cell disease affects approximately 100,000 people in the U.S.
- The condition is characterized by abnormally shaped red blood cells.
- Pain crises are a hallmark symptom of sickle cell anemia.
- Factors like dehydration and stress can trigger pain episodes.
- Understanding the symptoms is key to managing the condition.
Understanding Sickle Cell Disease
Sickle cell disease is a genetic disorder that affects red blood cells. It changes their shape and function, leading to health issues. This condition impacts hemoglobin, a protein in red blood cells that carries oxygen.
What Is Sickle Cell Disease?
Sickle cell disease is caused by abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S. This abnormality makes red blood cells take on a sickle shape, mainly when oxygen levels are low. The sickling of red blood cells can cause them to break down early and get stuck in small blood vessels, blocking blood flow.
The Genetic Basis of Sickle Cell Disease
The disease is caused by a mutation in the HBB gene, which codes for the beta-globin subunit of hemoglobin. This mutation leads to the production of sickle hemoglobin. It is inherited in an autosomal recessive pattern, meaning a person needs two defective HBB genes to have the disease.
Carriers, who have only one defective gene, usually don’t show symptoms but can pass the gene to their children.
Types of Sickle Cell Disease
There are several types of sickle cell disease, based on genetic mutations. The most common is sickle cell anemia (HbSS), where a person has two sickle hemoglobin genes. Other types include HbSC disease and HbS beta-thalassemia, caused by different abnormal hemoglobin genes.
Knowing the specific type of sickle cell disease is key to managing it well.
The Science Behind Sickle Cell Anemia

Sickle cell anemia is a genetic disorder that affects hemoglobin in red blood cells. Hemoglobin is a protein that carries oxygen to the body’s parts. This disorder changes how hemoglobin works, leading to sickle-shaped red blood cells.
How Hemoglobin Abnormalities Cause Sickling
Hemoglobin abnormalities are the main cause of sickle cell anemia. A point mutation in the HBB gene leads to hemoglobin S. This hemoglobin can polymerize under low oxygen, making red blood cells rigid and sickle-shaped.
The sickling process is complex. It involves the concentration of hemoglobin S, oxygen levels, and other hemoglobin variants. Knowing these factors is key to finding effective treatments.
The Process of Cell Sickling and Blood Flow Obstruction
The sickling of red blood cells causes blood flow obstruction. These cells are rigid and sticky. They stick to the blood vessel walls, causing blockages.
This blockage leads to tissue ischemia and pain. It can also damage organs like the spleen, kidneys, and lungs. Managing the condition requires a broad approach, including pain management and preventing infections.
Pain: The Hallmark of Sickle Cell Disease
Sickle cell disease pain is more than just a symptom. It needs a detailed plan to manage. We’ll look at why the pain happens, where it hurts, how bad it is, and the difference between sudden and ongoing pain.
Why Sickle Cell Causes Pain
The pain comes from sickled red blood cells blocking small blood vessels. This causes tissue ischemia. The buildup of metabolic byproducts then triggers pain receptors.
Many things can make sickling worse, like dehydration, infections, and extreme temperatures. It’s key to manage these to avoid pain.
Locations and Intensity of Sickle Cell Pain
Pain from sickle cell can hit anywhere but often affects the back, chest, arms, and legs. The pain’s strength can change a lot, both in different people and in the same person over time.
The pain can be mild or very severe. It might feel sharp, dull, or throbbing. Knowing where and how hard the pain hits is key to managing it well.
| Location | Common Descriptions | Intensity Range |
| Back | Dull ache, sharp pain | Mild to Severe |
| Chest | Sharp, stabbing | Moderate to Severe |
| Arms and Legs | Aching, throbbing | Mild to Severe |
Acute vs. Chronic Sickle Cell Pain
It’s important to tell the difference between sudden and ongoing pain in sickle cell disease. Acute pain usually comes from a specific crisis. Chronic pain, on the other hand, can be from long-term organ damage or other issues.
Acute pain often needs quick medical help. Chronic pain management is a long-term plan. It might include medicine, lifestyle changes, and support for the mind.
Sickle Cell Crisis Explained
Sickle cell crisis is a severe condition that causes a lot of pain. It happens when sickle-shaped red blood cells block blood vessels. This leads to tissue damage and pain. Knowing what triggers a crisis and its signs is key to managing it well.
What Triggers a Sickle Cell Crisis
Several things can start a sickle cell crisis, including:
- Infections: Fever and infections can cause a crisis by making red blood cells sickle more.
- Dehydration: Not having enough fluids can make the blood thicker, leading to sickling.
- Extreme Temperatures: Both very hot and very cold temperatures can trigger a crisis.
- Physical Stress: Too much physical activity or stress can also start a crisis.
Duration and Progression of Pain Episodes
Pain episodes, or crises, can last from a few hours to several days. The pain can get worse quickly, often needing immediate medical help.
It’s very important to manage pain well. This means using medicine, staying hydrated, and resting. Knowing how pain episodes progress helps plan the right response.
Emergency Signs During a Crisis
It’s critical to know the emergency signs of a sickle cell crisis. These include:
- Severe Pain: Pain that usual treatments can’t fix.
- Shortness of Breath: Trouble breathing or breathing too fast.
- Pale Lips or Nail Beds: Signs of anemia or poor oxygen.
- Fever: High fever, often with signs of infection.
If you see any of these signs, get medical help right away. Quick treatment can stop serious problems.
Living with sickle cell disease means managing crises well. By knowing what triggers a crisis and its signs, people can get help fast. This reduces the chance of serious problems.
Comprehensive Sickle Cell Anemia Symptoms

It’s important to know the many symptoms of sickle cell anemia for good care. This genetic disorder affects how red blood cells are made. It leads to abnormal cells that can cause health problems, from mild to severe.
Early Symptoms in Infants and Children
Babies and kids with sickle cell anemia might show jaundice. This is when their skin and eyes turn yellow because of too much bilirubin. They might also have swelling in their hands and feet from pain crises.
They often get sick more easily because their spleen, which fights off infections, can be damaged. As they get older, they might have more pain crises. These can be caused by things like not drinking enough water, being cold, or being at high altitudes.
Common Symptoms in Adults
Adults with sickle cell anemia can face many problems. They might have chronic pain, anemia, and get sick more often. They could also have vision problems because of the disease’s effect on blood vessels in the eyes.
They are also at risk for pulmonary hypertension. This can lead to heart failure. The severity and how often these symptoms happen can vary a lot. It depends on the type of the disease and the person’s health.
Severity Spectrum of Symptoms
The symptoms of sickle cell anemia can be mild or very severe. Some people might not have many problems and live a pretty normal life. Others might have to go to the hospital a lot because of bad pain crises or other serious health issues.
It’s key for doctors to understand this severity spectrum. They can then make treatment plans that fit each patient’s needs. By spotting early signs of problems and managing symptoms well, they can help improve life for those with sickle cell anemia.
Beyond Pain: Other Complications of Sickle Cell Disease
Sickle cell disease affects more than just pain. It impacts many areas of health. This can change a person’s quality of life and how long they live.
Organ Damage and Dysfunction
The disease can harm organs because of sickled red blood cells. Organ damage is common. Organs like the spleen, kidneys, and liver are often affected.
- The spleen is very sensitive and often stops working early in life.
- Kidney damage can lead to chronic kidney disease or failure, needing dialysis or a transplant.
- Liver damage can cause jaundice and severe liver problems due to bilirubin buildup.
| Organ | Complication | Consequence |
| Spleen | Dysfunction due to sickling | Increased infection risk |
| Kidneys | Damage from obstructed blood flow | Chronic kidney disease or failure |
| Liver | Accumulation of bilirubin | Jaundice and liver dysfunction |
Increased Infection Risk
People with sickle cell disease face a higher infection risk. This is mainly because their spleen doesn’t work right. It’s important to prevent infections and treat them quickly.
Vaccinations are key in fighting infections. Getting vaccinated against pneumococcus, meningococcus, and Haemophilus influenzae type b is important.
Growth and Development Issues
Sickle cell disease can also affect growth and development in kids. Chronic anemia and frequent pain can hurt nutrition and development.
It’s important to watch how kids grow. Healthcare teams work together to help. Good nutrition and managing anemia are part of the care.
Diagnosing Sickle Cell Disease
Early diagnosis of sickle cell disease is key to providing the right care. There are several methods to diagnose this condition. Each method is important at different stages of life.
Newborn Screening
Newborn screening for sickle cell disease is a first step. It’s done soon after birth with a blood sample from a heel prick. This test can spot abnormal hemoglobin, a sign of the disease.
The Centers for Disease Control and Prevention (CDC) says all 50 states in the U.S. now screen newborns for sickle cell disease. This has greatly improved early detection and care.
Blood Tests and Genetic Testing
Beyond newborn screening, blood tests and genetic testing are key for diagnosing sickle cell disease at any age. Blood tests can find the abnormal hemoglobin that causes the condition.
- Hemoglobin Electrophoresis: This test separates and identifies different types of hemoglobin in the blood, helping diagnose sickle cell disease.
- High-Performance Liquid Chromatography (HPLC): HPLC is another precise method used to detect abnormal hemoglobin levels.
- Genetic Testing: This involves analyzing DNA to identify the genetic mutation causing sickle cell disease. It’s useful for prenatal diagnosis and identifying carriers.
| Test Type | Purpose | Age Group |
| Newborn Screening | Early detection of sickle cell disease | Newborns |
| Hemoglobin Electrophoresis | Diagnose sickle cell disease by identifying abnormal hemoglobin | Any age |
| Genetic Testing | Identify genetic mutations causing sickle cell disease | Prenatal, any age |
Sickle Cell Trait vs. Sickle Cell Disease
Knowing the difference between sickle cell trait and sickle cell disease is key. Both are linked to the sickle cell gene but affect health differently. They also have different effects on future generations.
Understanding Sickle Cell Trait
Sickle cell trait happens when someone has one normal and one sickle hemoglobin gene. This makes them a “carrier” of the sickle cell gene. Carriers are different from those with sickle cell disease, who have two sickle genes.
People with sickle cell trait usually don’t show the full symptoms of sickle cell disease. But, they might face health issues under certain conditions, like intense exercise or high altitudes.
Symptoms of Sickle Cell Trait
Most with sickle cell trait live normal lives without major health problems. But, some might face:
- Microscopic hematuria (blood in the urine)
- Increased risk of dehydration
- Rare complications during intense physical exertion
It’s important for those with sickle cell trait to drink plenty of water, even when they’re very active. This helps avoid health risks.
Genetic Implications for Future Generations
The genetic side of sickle cell trait is very important. If both parents carry the sickle cell gene, there’s a:
- 25% chance with each pregnancy that the child will have sickle cell disease
- 50% chance that the child will be a carrier like the parents
- 25% chance that the child will neither have the disease nor be a carrier
It’s vital to understand these risks for family planning and genetic counseling. Carriers should talk to healthcare providers about their options and the implications for their kids.
Pain Management Strategies for Sickle Cell Disease
Managing pain is key for those with sickle cell disease. We use a mix of medical treatments, lifestyle changes, and support to help. This approach helps manage pain effectively.
Medications for Pain Relief
Medicines are essential for sickle cell pain management. We use everything from over-the-counter drugs to prescription medications. Nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids are often used to reduce pain.
It’s important to know how to use these medicines right. NSAIDs work for mild to moderate pain, while opioids are for severe pain. We also think about the side effects and risks of long-term opioid use.
| Medication Type | Use in Sickle Cell Disease | Notable Side Effects |
| NSAIDs | Mild to moderate pain relief | Gastrointestinal issues, kidney strain |
| Opioids | Severe pain relief | Constipation, risk of dependency |
Hydration and Its Importance
Drinking enough water is vital for sickle cell disease management. It helps prevent dehydration, which can cause pain. We advise drinking lots of water and hydrating fluids.
Staying hydrated is key to preventing pain crises and keeping overall health good. It’s important for those with sickle cell to drink fluids often during the day.
Non-Pharmaceutical Pain Management Techniques
There are many non-medical ways to manage pain. These include physical therapy, deep breathing, meditation, and using heat or cold packs.
These methods can be used with medicines to improve pain relief. For example, cognitive-behavioral therapy (CBT) helps people cope with chronic pain.
By using these methods together, we can create a better pain management plan. This plan meets the complex needs of those with sickle cell disease.
Medical Treatments for Sickle Cell Anemia
There are many treatments for sickle cell anemia. They help manage symptoms and treat the disease itself. Thanks to research, we now have several options to help patients.
Disease-Modifying Medications
Medicines that change the disease’s course are key. They include:
- Hydroxyurea: It cuts down on pain crises and might reduce blood transfusions.
- L-Glutamine: It also lowers pain crisis frequency.
- Crizanlizumab: This drug reduces vaso-occlusive crises.
These medicines work in different ways. They either lessen painful episodes or ease other symptoms of sickle cell anemia.
Blood Transfusions
Blood transfusions are also vital. They give patients normal red blood cells to:
- Lower the chance of sickled red blood cells.
- Boost oxygen to tissues and organs.
- Help prevent strokes.
Getting blood transfusions regularly can greatly improve life quality for those with severe sickle cell disease.
Stem Cell Transplantation
Stem cell transplant is the only cure for sickle cell disease. It replaces the patient’s bone marrow with healthy marrow from a donor.
Benefits and Risks: It’s a cure, but it’s risky. Risks include graft-versus-host disease and needing to take immunosuppressants for life.
Emerging Gene Therapies
Gene therapy is a new hope for sickle cell anemia. It aims to fix the genetic flaw causing the disease, aiming for a cure.
| Therapy Type | Description | Status |
| Lentiglobin | Uses a lentiviral vector to deliver a modified beta-globin gene. | Clinical Trials |
| CRISPR/Cas9 | Edits the HBB gene to correct the sickle mutation. | Early Stage Research |
Gene therapies are in various stages, with some in trials. These new treatments could change how we manage sickle cell anemia.
Living with Sickle Cell Disease
Living with sickle cell disease means managing symptoms and making healthy choices. It’s about avoiding things that could cause a crisis. We know it takes a lot, including medical care, lifestyle changes, and emotional support.
Lifestyle Modifications
Changing your lifestyle can help manage sickle cell disease. Avoiding extreme temperatures is key. Also, steer clear of high altitudes and too much exercise.
| Lifestyle Change | Benefit |
| Avoiding extreme temperatures | Reduces risk of crisis |
| Regular, moderate exercise | Improves overall health and well-being |
| Healthy diet | Supports overall health and reduces complication risk |
Avoiding Crisis Triggers
Knowing and avoiding crisis triggers is vital. Common ones include infections, dehydration, and extreme weather. It’s important to know what triggers you and how to avoid them.
By being proactive, making smart lifestyle choices, and watching out for crisis triggers, you can live a full life with sickle cell disease. We’re here to support you with care and guidance.
Psychological Impact of Chronic Sickle Cell Pain
Chronic pain from sickle cell disease is more than just physical. It deeply affects a person’s mental health and daily life. This condition can change how someone feels about themselves and their life.
Depression and Anxiety
People with sickle cell disease often face depression and anxiety. This is because their pain is constant and unpredictable. Research shows they are more likely to have these mental health issues than others.
Key statistics on depression and anxiety in sickle cell patients:
| Condition | Prevalence in Sickle Cell Patients | Prevalence in General Population |
| Depression | 25% | 7% |
| Anxiety | 30% | 10% |
Impact on Quality of Life
Chronic sickle cell pain greatly lowers a person’s quality of life. It makes it hard to work, keep friends, and do everyday things. The pain and fear of more pain can make someone feel alone and hopeless.
Coping Mechanisms and Support
It’s important to find ways to cope and get support for sickle cell disease. This includes talking to a therapist, joining support groups, and learning to manage stress. Techniques like meditation and deep breathing can help.
Coping strategies for patients with sickle cell disease:
- Regular psychological counseling
- Participation in support groups
- Stress management techniques
- Family and social support
By understanding the psychological effects of chronic sickle cell pain and using effective coping strategies, people can improve their lives. They can better manage their condition and feel better overall.
Special Considerations for Children with Sickle Cell
Children with sickle cell disease need a detailed care plan. This includes educational support, regular health checks, and getting ready for adult care. A thorough approach is key to bettering their lives.
Educational Needs and Accommodations
Students with sickle cell disease might need special help at school. They might miss school often, feel tired, or need pain relief. Schools can help by being flexible with attendance, providing rest spots, and training staff to handle sickle cell emergencies.
Growth and Development Monitoring
It’s important to keep an eye on how children with sickle cell grow and develop. Doctors should watch their height, weight, and overall health. This helps catch any growth or development problems early.
Transitioning to Adult Care
When kids with sickle cell grow up, they need help learning to manage their disease. This includes learning about self-care, making healthy choices, and understanding the adult healthcare system.
In summary, caring for kids with sickle cell involves meeting their educational needs, tracking their growth, and preparing them for adult care. Here’s a quick overview:
| Aspect | Considerations |
| Educational Needs | Flexible attendance, rest areas, trained staff |
| Growth Monitoring | Regular height, weight checks, nutritional counseling |
| Transitioning to Adult Care | Self-management education, lifestyle counseling, healthcare navigation |
Advances in Sickle Cell Research and Treatment
Recent years have brought big steps forward in sickle cell research. This gives new hope to those with the disease. New treatments and ways to manage the condition are being developed.
Recent Breakthroughs
Gene therapy is a big breakthrough in treating sickle cell disease. Gene editing technologies like CRISPR/Cas9 can fix the genetic problem. Early trials show these therapies could greatly reduce symptoms.
Disease-modifying therapies are also making progress. Medications like hydroxyurea help lessen pain crises. They might also lower the risk of other sickle cell complications.
“The advent of gene therapy and disease-modifying treatments marks a significant shift in the management of sickle cell disease, providing patients with more effective and sustainable treatment options.”
Clinical Trials and Research Opportunities
Clinical trials are key to improving sickle cell disease treatment. Many trials are exploring new treatments. These include:
- Gene therapies to fix the sickle cell mutation
- New drugs to reduce sickling and improve blood flow
- Stem cell transplantation to replace sick bone marrow with healthy one
Joining clinical trials can give patients access to new treatments. It also helps us learn more about the disease.
| Treatment | Description | Potential Benefits |
| Gene Therapy | Corrects the genetic mutation causing sickle cell disease | Potential cure, reduction in pain crises |
| Disease-Modifying Therapies | Reduces frequency and severity of symptoms | Improved quality of life, reduced complications |
| Stem Cell Transplantation | Replaces diseased bone marrow with healthy marrow | Potential cure, elimination of disease symptoms |
Future Directions in Treatment
As research keeps moving forward, sickle cell disease treatment will likely change a lot. Future steps might include:
- More targeted therapies based on each patient’s genetic and molecular traits.
- Improvements in gene editing to make it safer and more effective.
- More people getting to join clinical trials and try new treatments.
The future of sickle cell disease treatment looks bright. Ongoing research and trials are leading to better management and possibly cures.
Conclusion: Living Well Despite Sickle Cell Pain
Living with sickle cell disease means you need a full plan to handle its pain. Knowing the disease well and using good pain management can really help. This way, people can live better lives.
Handling sickle cell pain takes medical help, changes in lifestyle, and support from others. We’ve looked at sickle cell disease from its genetic roots to new treatments. It shows the need for a care plan that covers all bases.
Being proactive about health can lower the risk of problems and improve well-being. With the right knowledge, medical care, and support, living well with sickle cell is possible. It lets those affected enjoy life, even with its challenges.
FAQ
What is sickle cell disease?
Sickle cell disease is a genetic disorder. It affects how red blood cells make hemoglobin. This makes the cells misshapen and break down, leading to health problems.
What are the symptoms of sickle cell anemia?
Symptoms include pain episodes, anemia, infections, and swelling in hands and feet. These symptoms can vary in severity and frequency.
How is sickle cell disease diagnosed?
Diagnosis is through newborn screening, blood tests, and genetic testing. These tests find the abnormal hemoglobin causing the condition.
What is the difference between sickle cell trait and sickle cell disease?
Sickle cell trait means having one mutated gene copy. It usually doesn’t cause full disease symptoms. Sickle cell disease happens with two mutated gene copies, showing full symptoms.
How is sickle cell pain managed?
Pain management includes medicines, hydration, and non-medical methods like relaxation and heat therapy. These help reduce sickle cell pain.
What are the complications of sickle cell disease?
Complications include organ damage, increased infection risk, growth issues, and other serious health problems.
Can sickle cell disease be cured?
The only cure now is stem cell transplantation, but it’s not for everyone. It has risks. Gene therapy is also being explored as a future cure.
How can individuals with sickle cell disease manage their condition daily?
Daily management includes staying hydrated, avoiding extreme temperatures, managing stress, and following treatments. This helps prevent crises and manage symptoms.
What are the psychological impacts of living with sickle cell disease?
Living with sickle cell disease can lead to depression, anxiety, and other mental health issues. This is due to chronic pain and unpredictable crises. It requires strong support.
Are there any new treatments being developed for sickle cell disease?
Yes, research is ongoing for new treatments. This includes gene therapy, new medicines, and other innovative methods. They aim to reduce symptoms and improve life quality.
How does sickle cell disease affect children?
Children with sickle cell disease may face delayed growth, more infections, and other complications. They need special care and monitoring to manage their condition well.
What lifestyle changes can help manage sickle cell disease?
Lifestyle changes like a healthy diet, staying hydrated, avoiding smoking, and stress management can help manage the condition. They can also reduce crisis frequency.
References
- World Health Organization. (2025). WHO recommendations on the management of sickle-cell disease during pregnancy, childbirth, and the interpregnancy period. Retrieved from https://www.who.int/publications/i/item/9789240109124



































