Last Updated on October 21, 2025 by mcelik
Did you know over 1.6 billion people worldwide suffer from anemia? Among them, sickle cell anemia is a major contributor. In fact, sickle cell disease affects over 20 million people globally, making it a critical condition to understand.
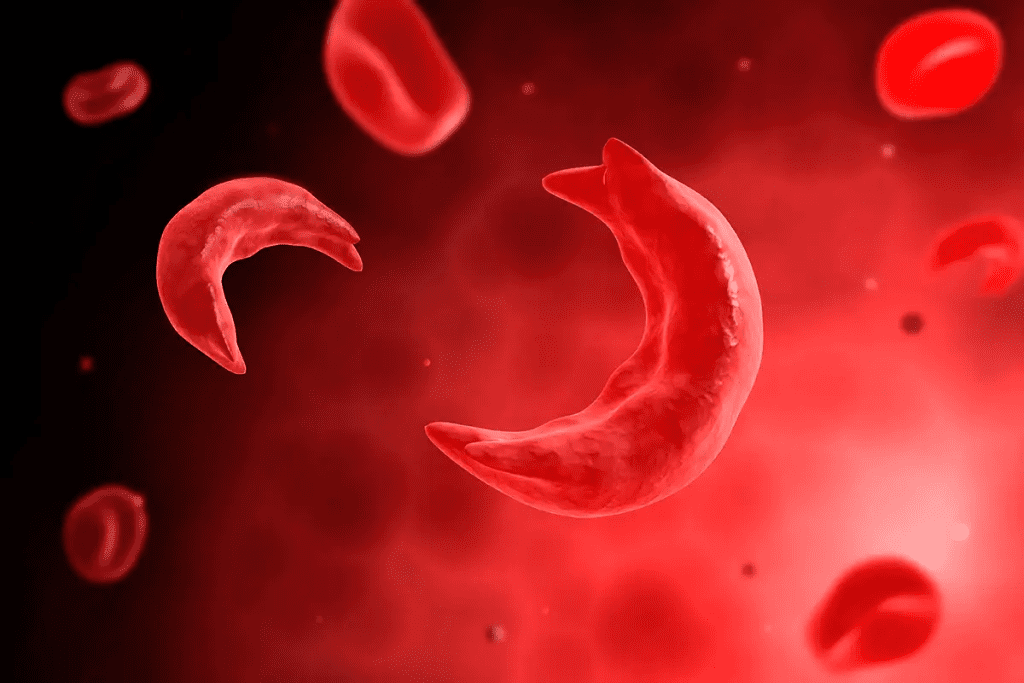
We aim to give you a clear picture of sickle cell anemia, including its causes, symptoms, and treatment options. This genetic disorder disrupts hemoglobin production, causing red blood cells to take on an abnormal sickle shape. These irregular cells can block blood flow, leading to pain and other health complications.
Understanding sickle cell anemia is key to managing its effects and improving quality of life. In this article, we’ll explore its prevalence, common symptoms, and the most effective treatments available today.
Key Takeaways
- Sickle cell disease is a significant global health burden.
- Over 20 million people worldwide are affected by sickle cell disease.
- Sickle cell anemia is a genetic disorder affecting hemoglobin production.
- Abnormally shaped red blood cells characterize the condition.
- Understanding the causes, symptoms, and treatments is key for management.
Understanding Sickle Cell Anemia
To grasp sickle cell anemia, we must explore its definition and history. We’ll look into its core aspects. This will help us understand more about it.
Definition and Classification
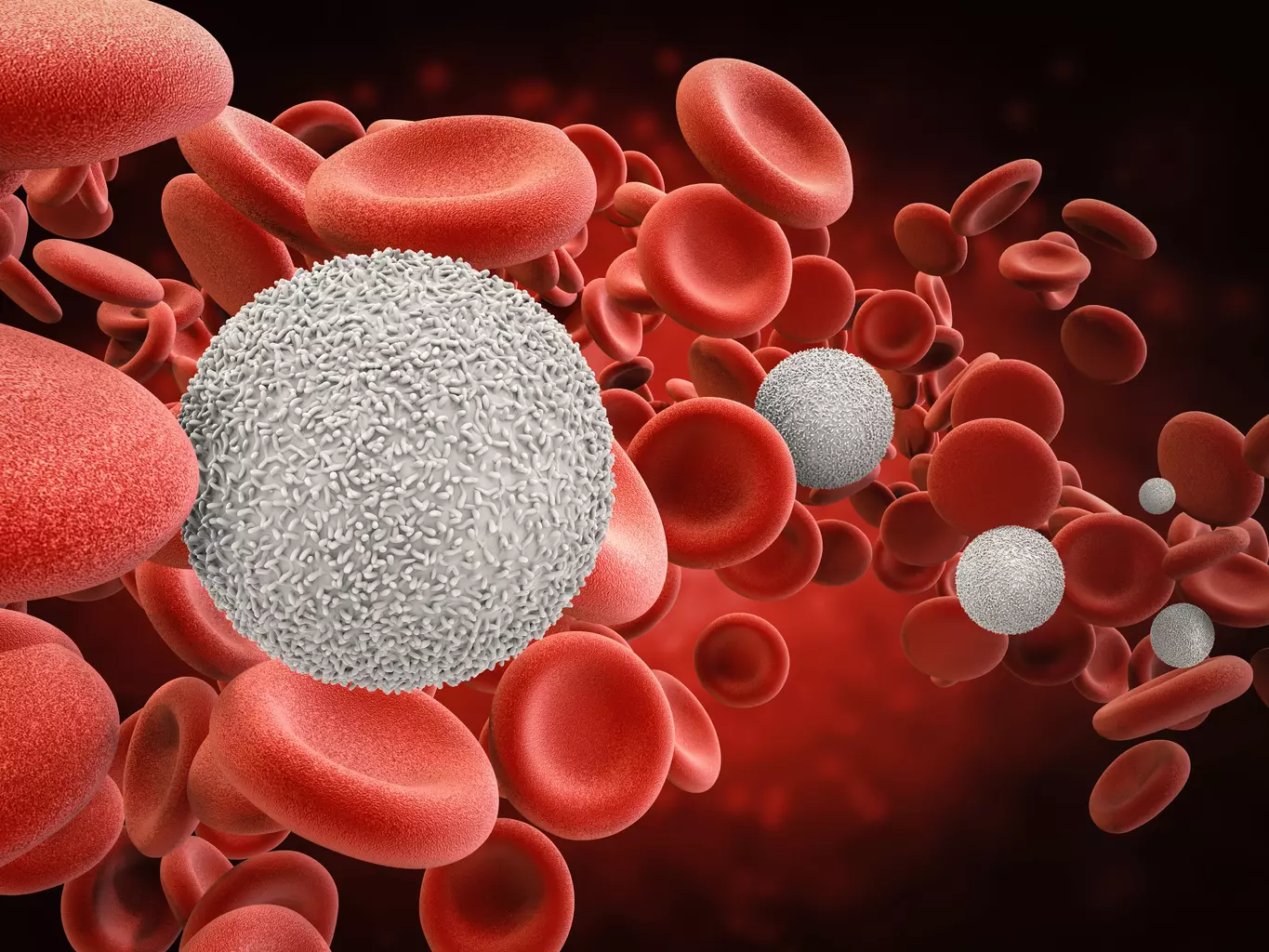
Sickle cell anemia is a genetic disorder. It causes abnormally shaped red blood cells. These cells can’t carry oxygen well and often break down early, causing anemia.
The types of sickle cell disease are based on certain genes. The main types are HbSS, HbSC, and HbS beta-thalassemia. Sickle cell anemia happens when someone has two HbS genes, one from each parent.
Historical Background
Sickle cell anemia was first noted in the early 1900s. It started a long journey to understand this complex disease. It was known for its severe anemia and unique red blood cells.
Understanding sickle cell anemia has grown over time. From early findings to today’s genetic studies, our knowledge has grown. This has led to better sickle cell anemia treatment options.
The Science Behind Sickle Cell Anemia
Sickle cell anemia is a genetic disorder that affects hemoglobin production. Hemoglobin is a protein in red blood cells that carries oxygen. It’s vital for our bodies to function properly.
Normal Hemoglobin vs. Sickle Hemoglobin
Normal hemoglobin, or hemoglobin A, is key for red blood cells to work right. It keeps these cells flexible and able to move through blood vessels easily. On the other hand, sickle hemoglobin, or hemoglobin S, makes red blood cells stiff and sickle-shaped under certain conditions.
The main difference between normal and sickle hemoglobin is their molecular structure. Normal hemoglobin has glutamic acid at the sixth position of the beta-globin chain. Sickle hemoglobin has valine instead. This change comes from a point mutation in the HBB gene.
The Genetic Mutation
The genetic mutation causing sickle cell anemia is a single nucleotide change in the HBB gene. This change leads to sickle hemoglobin instead of normal hemoglobin A. The mutation is inherited in an autosomal recessive pattern.
People who inherit only one copy of the mutated gene are carriers of sickle cell trait. They usually don’t show all the symptoms of sickle cell anemia. But, they can pass the mutated gene to their children.
| Hemoglobin Type | Molecular Structure | Effect on Red Blood Cells |
| Normal Hemoglobin (A) | Glutamic acid at the sixth position of the beta-globin chain | Flexible, normal shape |
| Sickle Hemoglobin (S) | Valine at the sixth position of the beta-globin chain | Rigid, sickle shape under low oxygen conditions |
Knowing the genetic basis and the differences between normal and sickle hemoglobin is key. It helps in developing diagnostic tools and treatments for sickle cell anemia.
Causes of Sickle Cell Anemia
Sickle cell anemia is a genetic disorder passed down in an autosomal recessive pattern. This means a person needs two abnormal genes, one from each parent, to have the disease.
We will look into how this genetic pattern works and the risks of sickle cell anemia.
Genetic Inheritance Patterns
Sickle cell anemia comes from a mutation in the HBB gene. This gene codes for a part of hemoglobin. If someone gets two mutated genes, one from each parent, they will have sickle cell anemia.
If someone gets only one mutated gene, they are a carrier. They usually don’t show all the disease’s symptoms but might have some mild ones under certain conditions.
Carrier Status and Inheritance:
- If both parents are carriers, there’s a 25% chance with each pregnancy that the child will have sickle cell anemia.
- There’s a 50% chance the child will be a carrier like each parent.
- There’s a 25% chance the child will neither have the disease nor be a carrier.
Risk Factors
Several risk factors are linked to sickle cell anemia, mainly because of its genetic pattern.
| Risk Factor | Description |
| Family History | A family history of sickle cell anemia or trait increases the risk. |
| Ethnic Background | Sickle cell anemia is more common in individuals of African, Caribbean, Middle Eastern, and South Asian descent. |
| Carrier Status of Parents | If both parents are carriers of the mutated gene, their children are at higher risk. |
Epidemiology of Sickle Cell Anemia
It’s important to know about sickle cell anemia’s spread to help public health. This genetic disorder messes with red blood cells’ hemoglobin, causing health problems. It’s found all over, but its impact changes a lot by region and population.
Global Distribution
Sickle cell disease hits hard in Sub-Saharan Africa, the Middle East, and parts of India. These areas face a big public health challenge because of the sickle cell gene’s commonness.
- In Sub-Saharan Africa, a big part of the population deals with sickle cell disease. Some countries see a lot of sickle cell traits.
- The Middle East also struggles with sickle cell disease, with some countries seeing high rates.
- In India, certain tribal groups face a high risk of sickle cell disease.
Prevalence in the United States
In the U.S., sickle cell disease hits African Americans hard, though it’s found in other groups too.
Key stats on sickle cell disease in the U.S. are:
- 1 in 500 African Americans have sickle cell disease.
- 1 in 12 African Americans carry the sickle cell trait.
- Hispanic/Latino Americans, mainly from the Caribbean and Central America, also get sickle cell disease.
Demographics and Racial Considerations
The spread of sickle cell disease ties closely to racial and ethnic groups. In the U.S., African Americans are hit the hardest, but other groups are affected too.
Racial factors are key in sickle cell anemia’s spread. For example, people of African descent are more likely to carry the sickle cell trait. This raises the risk of sickle cell disease in their kids.
- African Americans face a higher risk of sickle cell disease.
- Hispanic/Latino groups, mainly from the Caribbean, are also at risk.
- People from the Middle East and India might also carry the sickle cell trait.
Knowing these racial and demographic facts is vital for making public health plans to fight sickle cell disease.
Signs and Symptoms of Sickle Cell Anemia
Sickle cell anemia shows different signs in different people. It’s a genetic disorder that affects how red blood cells are made. These cells can get stuck in blood vessels, causing health problems.
Acute Symptoms
Acute symptoms of sickle cell anemia come on suddenly and can be very bad. A common symptom is a pain crisis. This happens when sickled cells block blood vessels, causing pain.
Other acute symptoms include:
- Severe pain episodes
- Swelling in the hands and feet
- Infections
- Anemia
These symptoms need quick medical help to manage pain and avoid worse problems.
Chronic Symptoms
People with sickle cell anemia also face chronic symptoms. These include:
- Persistent anemia
- Jaundice
- Increased risk of infections
- Delayed growth and development in children
These symptoms can really affect someone’s life, making ongoing care very important.
Pain Crises
Pain crises, or vaso-occlusive crises, are a key symptom of sickle cell anemia. They happen when sickled cells block blood flow, causing pain. Many things can trigger these crises, such as:
- Cold temperatures
- Dehydration
- Stress
- Infections
Managing pain crises involves using pain medicines, staying hydrated, and resting. Knowing what triggers them and taking steps to prevent them can help lessen their impact.
We know that dealing with sickle cell anemia is tough. Our healthcare team is here to offer full support. We aim to help manage symptoms and improve life quality.
Complications Associated with Sickle Cell Anemia
Sickle cell anemia can lead to serious complications that affect a person’s quality of life. These issues stem from the disease’s impact on hemoglobin and various body systems.
Organ Damage
Organ damage is a major complication of sickle cell anemia. It can harm organs like the spleen, kidneys, and liver. This damage is caused by the abnormal sickling of red blood cells.
The spleen is often hit hard, becoming dysfunctional or shrinking. This makes it harder for the body to fight off infections, as the spleen helps filter out pathogens.
Infections
People with sickle cell anemia face a higher risk of infections. This is mainly because their spleens don’t work well. Such infections can be severe and even deadly, making it vital to prevent them and treat them quickly.
They often get infections like pneumonia and other bacterial infections. Their immune system is weakened, making them more susceptible to these dangers.
Other Health Complications
There are also other health complications for those with sickle cell anemia. These include stroke, acute chest syndrome, and priapism, among others.
Stroke is a big worry because it can happen when sickled red blood cells block brain blood vessels. Acute chest syndrome is another serious issue that can be deadly and needs immediate care.
It’s important to understand these complications to manage sickle cell anemia well. By knowing the risks and taking steps to prevent them, healthcare teams can help lessen their impact on patients’ lives.
Diagnosis of Sickle Cell Anemia
We use various tests to diagnose sickle cell anemia, from newborn screening to genetic testing. Finding the disease early is key to managing it well. It helps improve life quality for those with sickle cell disease.
Newborn Screening
Newborn screening is a vital first step. It’s done in the first few days of life. It spots babies with the disease or who carry it. Early detection leads to better outcomes.
Blood Tests
Blood tests confirm sickle cell anemia. They include:
- Hemoglobin electrophoresis to spot abnormal hemoglobin
- High-performance liquid chromatography (HPLC) to check hemoglobin levels
- Complete Blood Count (CBC) to look at blood health
These tests help doctors understand the disease’s severity. They then plan the best treatment.
Genetic Testing
Genetic testing finds the genetic causes of sickle cell anemia. It’s useful for families to know their risk. Genetic counseling often goes with this testing.
Together, newborn screening, blood tests, and genetic testing help doctors diagnose sickle cell anemia. They offer detailed care.
Sickle Cell Trait vs. Sickle Cell Anemia
Sickle cell trait and sickle cell anemia are two related but different conditions. They affect how the blood makes hemoglobin. Both involve sickle hemoglobin but have different health and family planning implications.
Differences in Symptoms and Severity
People with sickle cell trait usually don’t have the severe symptoms of sickle cell anemia. They have one normal and one sickle hemoglobin gene, leading to mild or no symptoms. On the other hand, sickle cell anemia happens when someone has two sickle hemoglobin genes, causing more serious health problems.
The main differences in symptoms and severity are:
- Frequency and Severity of Pain Crises: Those with sickle cell anemia have frequent pain crises due to blocked blood flow. People with sickle cell trait rarely experience these episodes.
- Anemia: Sickle cell anemia often causes significant anemia due to red blood cell destruction. This is not common in those with sickle cell trait.
- Infections and Organ Damage: Sickle cell anemia makes people more likely to get infections and organ damage. These complications are less common in those with sickle cell trait.
Implications for Carriers
Carrying the sickle cell trait affects not just the person but also their family planning. Carriers are usually healthy but can pass the sickle cell gene to their kids. If both parents are carriers, there’s a 25% chance with each pregnancy that the child will have sickle cell anemia.
It’s important for carriers to understand the genetic risks. Genetic counseling can help with family planning decisions. Key points include:
- Genetic Testing: Carriers should know about genetic testing for their partners and the risks to their kids.
- Family Planning Options: Knowing about the condition helps carriers make informed family planning choices.
- Monitoring and Management: Even though carriers are usually healthy, knowing their status helps manage health issues that might arise, like under extreme physical exertion.
We stress the importance of understanding sickle cell trait and sickle cell anemia for carriers and those affected. This knowledge leads to better health outcomes and informed decisions.
Treatment Options for Sickle Cell Anemia
When it comes to treating sickle cell anemia, each patient needs a plan that fits them best. This plan might include medicines, blood transfusions, and sometimes stem cell transplantation. It’s all about finding the right mix for each person.
Medications
Medicines are key in managing sickle cell anemia. Hydroxyurea is often used to lessen pain crises and may cut down on blood transfusions. Other drugs help with pain, prevent infections, and tackle other disease-related issues.
- Pain Management: Pain is a big part of sickle cell anemia. Doctors use NSAIDs, opioids, and other pain relievers to help manage it.
- Preventive Care: Preventive medicines, like antibiotics and vaccines, are vital. They help lower the risk of infections, which are a big concern for those with sickle cell anemia.
Blood Transfusions
Blood transfusions are also a big part of managing sickle cell anemia. They help by reducing the chance of complications by lowering the number of sickled red blood cells. Chronic transfusion therapy is often used for those with severe cases or who have faced serious complications.
“Regular blood transfusions can significantly improve the quality of life for patients with sickle cell anemia by reducing the frequency of pain crises and other complications.”
Stem Cell Transplantation
Stem cell transplantation, or bone marrow transplantation, is the only cure for sickle cell anemia. It involves swapping the patient’s bone marrow with healthy marrow from a donor. While it’s a cure, it comes with risks and is usually considered for those with severe disease and a suitable donor.
We’re always learning more about sickle cell anemia and finding new ways to help patients and their families.
Research and Future Treatments
Researchers are making big steps in finding new treatments for sickle cell disease, including gene therapy. This progress is changing how we manage the condition. It brings new hope to patients.
Gene Therapy
Gene therapy fixes the genetic problem that causes sickle cell anemia. It tries to make normal hemoglobin again, which could cure the disease. Clinical trials have shown promising results, with some patients seeing big improvements.
The process takes a patient’s bone marrow cells, fixes the genetic defect with a viral vector, and then puts the fixed cells back in. While there are challenges, gene therapy could be a cure for sickle cell anemia.
Emerging Treatments
Other new treatments are being looked into too. These include new medicines to manage symptoms and prevent problems. Also, new ways like stem cell transplantation are being explored.
Emerging treatments are not just about curing the disease. They also aim to improve patients’ quality of life. For example, drugs to reduce pain crises are being developed.
The future for managing sickle cell disease looks bright. Ongoing research and clinical trials are leading to better treatments. As we learn more about the disease, we’ll get better at managing and possibly curing it.
Conclusion
Managing sickle cell disease well needs a team effort. This includes medical care, support, and research. Knowing the causes, symptoms, and issues it can cause is key to good care. We’ve seen how a complete approach is vital. New treatments like gene therapy and others show hope for those with sickle cell anemia. Dealing with sickle cell disease is a long-term effort. We need to keep researching and supporting each other. Together, we can make life better for those with this condition.
FAQ
What is sickle cell anemia?
Sickle cell anemia is a genetic disorder. It affects how red blood cells carry oxygen. This leads to anemia and other health issues.
What causes sickle cell anemia?
It’s caused by a genetic mutation. This mutation affects hemoglobin, a key protein in red blood cells.
How is sickle cell anemia inherited?
It’s inherited in an autosomal recessive pattern. This means a person needs two copies of the mutated gene to have the disease.
What are the symptoms of sickle cell anemia?
Symptoms include anemia, pain crises, and infections. These can vary in severity and how often they happen.
How is sickle cell anemia diagnosed?
It’s diagnosed through newborn screening and blood tests. Genetic testing also detects the mutated gene or abnormal hemoglobin.
What is the difference between sickle cell trait and sickle cell anemia?
Sickle cell trait has one copy of the mutated gene. Sickle cell anemia has two, leading to a more severe disease.
What are the treatment options for sickle cell anemia?
Treatments include medications, blood transfusions, and stem cell transplantation. These help manage symptoms and prevent complications.
Can sickle cell anemia be cured?
There’s no cure yet, but gene therapy and other treatments are being explored. They might change how we manage the disease.
How common is sickle cell anemia?
It’s more common in certain groups, like those of African, Caribbean, and Middle Eastern descent. In the U.S., about 1 in 500 African Americans have it.
What are the complications of sickle cell anemia?
Complications include organ damage and infections. These can be managed with proper care and medical attention.
Can white people get sickle cell anemia?
Yes, anyone can get sickle cell anemia if they inherit the mutated gene. It’s not limited to certain racial or ethnic groups.
What is the life expectancy for someone with sickle cell anemia?
With good care, people with sickle cell anemia can live into their 40s and 50s. Life expectancy varies based on disease severity and other factors.
References:
- Centers for Disease Control and Prevention. (2023). Sickle cell disease (SCD). https://www.cdc.gov/ncbddd/sicklecell/index.html
- Piel, F. B., Steinberg, M. H., & Rees, D. C. (2017). Sickle cell disease. New England Journal of Medicine, 376(16), 1561-1573. https://www.nejm.org/doi/full/10.1056/nejmra1510865