
Sickle cell disease is a common condition worldwide, affecting millions. It makes red blood cells take on a sickle shape. This leads to many health problems.
We know how crucial it is to care for those with sickle cell disease. Our team offers a variety of treatment options to meet each patient’s needs. This ensures the best results for them.
We’re dedicated to providing world-class healthcare. We offer full support to international patients. This helps us tackle the challenges of sickle cell anemia treatment.
Key Takeaways
- Understanding the prevalence and impact of sickle cell disease
- Comprehensive treatment approaches for managing the condition
- Importance of tailored care for individual patients
- Support services available for international patients
- Commitment to delivering world-class healthcare
Understanding Sickle Cell Disease
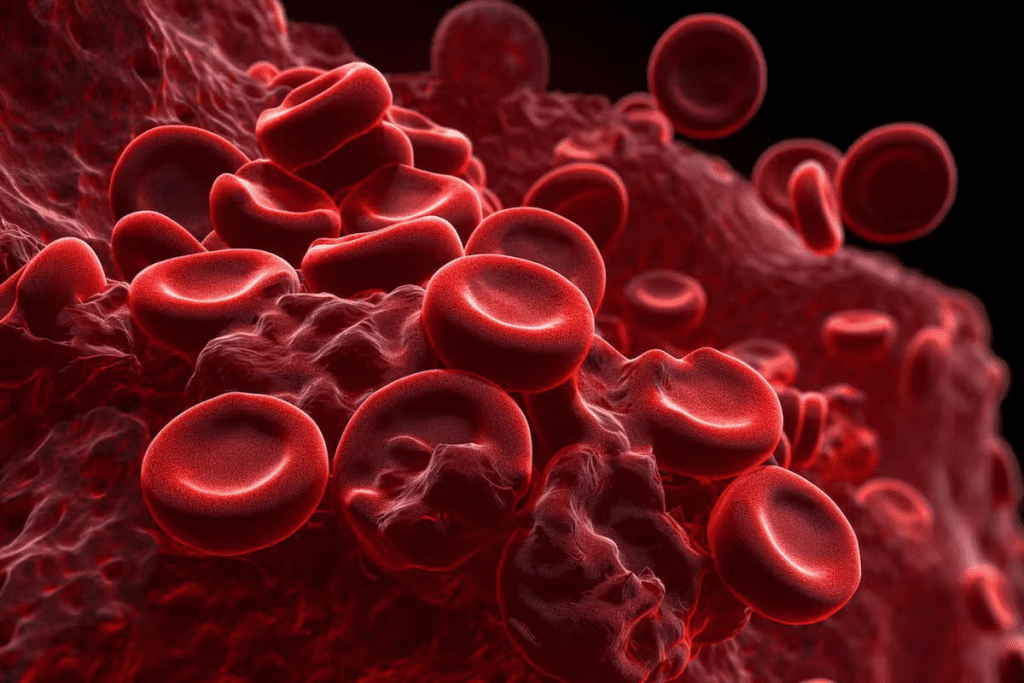
Sickle cell disease is a complex condition shaped by genetics and the environment. It affects hemoglobin, a key molecule in red blood cells. Hemoglobin carries oxygen to the body’s tissues.
The Genetic Basis of Sickle Cell Disease
Sickle cell disease comes from a mutation in the HBB gene. This gene codes for a part of hemoglobin. The mutation creates abnormal hemoglobin, called hemoglobin S (HbS).
Having two copies of this mutated gene, one from each parent, often leads to sickle cell disease. This explains why it’s more common in certain areas, especially where malaria was once common. The sickle cell trait helps protect against malaria.
How Abnormal Hemoglobin Affects Red Blood Cells
HbS makes red blood cells sickle-shaped under low oxygen conditions. These sickled cells are more likely to break down. They can also block small blood vessels, causing pain, infections, and anemia.
The sickling of red blood cells is a key feature of the disease. Knowing this helps in managing it better.
Different Types of Sickle Cell Disease
Sickle cell disease includes several types:
- HbSS (homozygous for HbS): The most common and often severe form.
- HbSC (compound heterozygote for HbS and HbC): Generally milder than HbSS.
- HbSβ+ thalassemia and HbSβ0 thalassemia: Variants that involve a combination of HbS with beta-thalassemia mutations.
| Type | Description | Severity |
| HbSS | Homozygous for HbS | Most severe |
| HbSC | Compound heterozygote for HbS and HbC | Milder |
| HbSβ+ thalassemia | HbS with beta-thalassemia | Varies |
| HbSβ0 thalassemia | HbS with beta-thalassemia | Severe |
Knowing these types is key for diagnosis, predicting outcomes, and creating treatment plans for each patient.
Diagnosing Sickle Cell Disease
Early diagnosis of sickle cell disease is key to better patient outcomes. Tests are used to find the abnormal hemoglobin that causes the disease.
Newborn Screening for Sickle Cell
Newborn screening is crucial for catching sickle cell disease early. It involves a simple blood test during routine newborn checks. This early detection leads to better care for children with the disease.
Studies show that early detection through newborn screening greatly helps manage sickle cell disease. This is seen in reports from places like Jamaica’s National Census Report in 2001.
Blood Tests for Sickle Cell Diagnosis
Blood tests are vital for diagnosing sickle cell disease. The most common test is hemoglobin electrophoresis. It separates hemoglobin types to spot sickle hemoglobin. Tests like HPLC and isoelectric focusing also help confirm the diagnosis.
These tests are key for finding sickle cell disease and knowing the type.
Genetic Testing and Counseling
Genetic testing reveals the genetic mutations behind sickle cell disease. This info is crucial for families, helping them understand their genetic risks. Genetic counseling supports families, offering guidance and support.
Knowing their genetic risks helps families plan better. They can make informed decisions about family planning and get the right medical care.
Common Symptoms and Complications
It’s important to know the symptoms and complications of sickle cell disease. This genetic disorder affects how red blood cells make hemoglobin. It leads to several health problems.
Recognizing Sickle Cell Crisis Episodes
A sickle cell crisis happens when abnormal red blood cells block small blood vessels. This causes severe pain. It’s crucial to treat these episodes quickly to avoid serious problems.
Symptoms of a sickle cell crisis include:
- Severe pain in the back, chest, arms, or legs
- Swelling in the hands and feet
- Pale skin or nail beds
- Fatigue or weakness
- Jaundice or yellowing of the skin and eyes
Acute Chest Syndrome and Other Complications
Acute chest syndrome is a serious issue in sickle cell disease. It causes chest pain, cough, and trouble breathing. It often comes with fever and can be deadly if not treated fast. Other problems include:
| Complication | Description |
| Acute Chest Syndrome | Causes chest pain, cough, and trouble breathing, often with fever. |
| Stroke | Occurs when sickled red blood cells block blood vessels in the brain. |
| Splenic Sequestration | A condition where red blood cells gather in the spleen, leading to severe anemia. |
Organ Damage from Sickle Cell Disease
Repeated sickling episodes can damage organs over time. The spleen, kidneys, liver, and heart are often affected. Regular monitoring and care can reduce organ damage risk.
Long-term effects of sickle cell disease on organs include:
- Splenic dysfunction or autosplenectomy
- Kidney damage or failure
- Liver dysfunction
- Cardiac complications, such as heart failure
Knowing these complications helps patients and doctors manage the disease better. This improves life quality.
Sickle Cell Anemia Treatment Approaches

Treating sickle cell anemia requires a mix of preventive steps, pain control, and ways to lessen complications. Each patient’s needs are different, so a custom plan is key.
Treatment Goals and Strategy
The main goal is to manage symptoms, prevent complications, and enhance life quality. Our strategy includes regular checks, lifestyle changes, and medical treatments. Effective treatment can greatly reduce crisis severity and frequency.
According to the Revista Cubana de Investigaciones Biomédicas, sickle cell disease treatment is complex. It includes preventive steps, pain management, and ways to lower complication risks. This comprehensive approach is vital for better patient results.
| Treatment Component | Description | Benefits |
| Preventive Measures | Vaccinations, regular check-ups | Reduces risk of infections and complications |
| Pain Management | Medications, hydration, rest | Alleviates pain during crises |
| Interventions | Blood transfusions, medication | Reduces severity of crises and complications |
Individualized Treatment Plans
Because sickle cell anemia affects people differently, individualized treatment plans are essential. Healthcare teams work with patients to create a plan that fits their unique needs. This plan considers their condition severity, medical history, and lifestyle.
“The treatment of sickle cell disease requires a personalized approach, considering the unique needs and circumstances of each patient.”
Expert Opinion
Emergency Treatment for Sickle Cell Crisis
In a sickle cell crisis, quick and effective treatment is vital. Emergency care often includes pain meds, hydration, and sometimes blood transfusions. Knowing the crisis signs and getting medical help fast can greatly improve outcomes.
Medications for Managing Sickle Cell Disease
Medications play a big role in managing sickle cell disease. They help lessen the number of painful episodes and other issues. Using the right medicines can greatly enhance the life quality of those with sickle cell disease.
Hydroxyurea: Mechanism and Benefits
Hydroxyurea is a key drug for sickle cell disease. It boosts the production of fetal hemoglobin, which is less likely to cause sickling. This leads to fewer painful episodes and might cut down on blood transfusions.
Benefits of Hydroxyurea:
- Reduces frequency of painful crises
- May reduce the need for blood transfusions
- Can improve overall survival
L-glutamine (Endari) and Other FDA-Approved Drugs
L-glutamine, known as Endari, is also approved for sickle cell disease. It’s thought to lessen oxidative stress in sickle red blood cells. This helps reduce the number of painful episodes.
| Medication | Mechanism | Benefits |
| Hydroxyurea | Increases fetal hemoglobin production | Reduces painful crises, may reduce need for transfusions |
| L-glutamine (Endari) | Reduces oxidative stress in sickle red blood cells | Reduces frequency of painful crises |
Pain Management Medications
Pain management is key in sickle cell disease care. Various pain meds are used, from over-the-counter options to stronger opioids for severe pain.
It’s crucial for patients to work closely with their healthcare provider to find the most effective pain management strategy.
Antibiotics for Infection Prevention
People with sickle cell disease face a higher risk of infections, especially from encapsulated bacteria. To prevent this, prophylactic antibiotics like penicillin are often given, especially to kids.
Knowing about the different medications helps those with sickle cell disease and their caregivers manage the condition better. This can greatly improve their quality of life.
Blood Transfusions in Sickle Cell Disease
Blood transfusions are key in managing sickle cell disease. They help reduce the risk of serious complications. We will look at how transfusions work, their benefits, and the risks.
Simple vs. Exchange Transfusions
There are two main types of blood transfusions for sickle cell disease: simple and exchange transfusions. Simple transfusions add normal hemoglobin to reduce sickled red blood cells. Exchange transfusions replace the patient’s red blood cells with donor ones, lowering sickled cells.
Exchange transfusions are for severe cases or high risk of stroke. They are more complex and need careful management to avoid issues.
When Transfusions Are Recommended
Transfusions are suggested in several situations for sickle cell disease patients. These include:
- Preventing stroke in children with abnormal transcranial Doppler ultrasound results
- Managing acute chest syndrome
- Treating severe anemia
- Preparing for surgery
The choice to transfuse depends on the patient’s needs and clinical judgment. It considers the risks and benefits of transfusions.
Managing Iron Overload from Repeated Transfusions
Repeated blood transfusions can lead to iron overload. This happens because transfused red blood cells carry iron. Over time, this can damage organs. To tackle iron overload, patients may get iron chelation therapy. This therapy uses medications to remove excess iron from the body.
It’s vital to monitor iron levels in patients getting frequent transfusions. Regular blood tests help healthcare providers adjust treatment to prevent iron overload.
Bone Marrow and Stem Cell Transplantation
Bone marrow and stem cell transplantation are new ways to cure sickle cell disease. They replace the patient’s bone marrow with healthy stem cells. This could get rid of the disease’s symptoms and problems.
Potential Cure through Transplantation
Transplantation can cure sickle cell disease by using healthy stem cells. These stem cells make normal hemoglobin. The patient’s bone marrow is prepared to accept these new cells, making healthy red blood cells.
Key benefits of transplantation include:
- Potential elimination of sickle cell crises
- Improved quality of life
- Reduction in disease-related complications
Finding a Compatible Donor
Finding a compatible donor is a key step in transplantation. Human leukocyte antigen (HLA) matching is used to find suitable donors. These are usually siblings or unrelated donors with matching HLA types.
| Donor Type | HLA Matching Requirement | Success Rate |
| Sibling Donor | Matched or partially matched | Higher success rate |
| Unrelated Donor | Fully matched | Comparable to sibling donors |
Risks and Recovery
Transplantation is not risk-free. It can lead to graft-versus-host disease (GVHD), infections, and organ damage. Patients need careful monitoring and care during recovery.
Recovery process involves:
- Monitoring for GVHD and infections
- Managing pain and discomfort
- Follow-up care to ensure engraftment
Choosing to have a transplant is a big decision. Patients should talk to their healthcare provider about the benefits and risks. This helps them make an informed choice.
Gene Therapy: The Future of Sickle Cell Treatment
Gene therapy is changing how we treat sickle cell disease. It aims to fix the disease at its source by changing the genetic code. This method corrects the mutation that causes sickle cell disease.
Current Clinical Trials in Gene Therapy
Many clinical trials are testing gene therapy for sickle cell disease. These trials use viral vectors to give healthy HBB genes to stem cells. Then, these cells are put back into the patient.
Key aspects of these trials include:
- Evaluating the safety and efficacy of different gene therapy approaches
- Assessing the durability of the treatment response
- Monitoring for potential side effects
CRISPR and Gene Editing Approaches
CRISPR/Cas9 gene editing is a new technology for precise genetic changes. It can fix the specific mutation causing sickle cell disease.
CRISPR and other gene editing technologies are promising for sickle cell disease treatment. Researchers are looking into several methods, including:
- Correcting the HBB gene mutation in stem cells
- Disrupting genes that contribute to the disease
- Enhancing genes that can help mitigate the effects of the disease
Accessibility of Gene Therapy Treatments
Gene therapy is promising but faces several challenges. These include:
| Challenge | Description |
| Cost | Gene therapy is very expensive, making it hard for many patients to access. |
| Complexity | The process of gene therapy is complex, needing specialized skills and equipment. |
| Regulatory Framework | The rules for gene therapy are still changing and differ by country. |
Overcoming these challenges is key to making gene therapy available to all who could benefit.
Managing Pain in Sickle Cell Disease
Pain management is key to a better life for sickle cell disease patients. It combines medicines and non-medical ways to meet each person’s needs.
Acute Pain Crisis Management
Acute pain crises need quick and effective treatment. We start by checking the pain’s severity and the patient’s history. Hydration and oxygen therapy help ease symptoms.
We use opioids and nonsteroidal anti-inflammatory drugs (NSAIDs) to manage pain. The right medicine and dose depend on the patient’s past experiences and the crisis’s severity.
Chronic Pain Treatment Strategies
Chronic pain is a big challenge in sickle cell disease. We create a long-term plan that includes medicines, lifestyle changes, and alternative therapies. Hydroxyurea helps reduce pain crises.
Cognitive-behavioral therapy (CBT) and other psychological support help with chronic pain. A healthy lifestyle, like regular exercise and a balanced diet, is also important.
Non-Pharmacological Pain Management
Non-medical ways are vital for pain management in sickle cell disease. Physical therapy, acupuncture, and relaxation therapy offer relief. They help reduce pain and boost well-being.
Patient education on pain management and coping strategies empowers individuals. Support from family, friends, and groups also helps manage pain better.
By using these strategies, we can create a detailed pain management plan. This plan improves the lives of those with sickle cell disease.
Preventive Care for Sickle Cell Patients
People with sickle cell disease can greatly benefit from a full preventive care plan. This care is key to managing the disease and lowering the chance of serious problems. We will cover the main parts of preventive care, like getting vaccinated, regular health checks, and ways to stop sickle cell crisis episodes.
Vaccination Schedule and Recommendations
It’s very important for those with sickle cell disease to keep up with their vaccinations. Recommended vaccines include the pneumococcal conjugate vaccine (PCV), pneumococcal polysaccharide vaccine (PPSV), influenza vaccine, and meningococcal vaccine. These shots help fight off infections that can cause sickle cell crises. Always follow the Centers for Disease Control and Prevention (CDC) for the latest vaccine schedule.
Regular Health Screenings and Monitoring
Regular health checks are crucial for catching and managing potential problems early. Annual comprehensive check-ups should include tests for organ damage, like kidney and liver function tests, and eye exams to spot retinopathy. Regular checks help find issues early, so they can be treated quickly.
Preventing Sickle Cell Crisis Episodes
Stopping sickle cell crisis episodes requires both lifestyle changes and medical help. Drinking plenty of water, avoiding extreme temperatures, and managing stress are key lifestyle changes. Also, taking prescribed medicines, like hydroxyurea, can help lessen crisis frequency. It’s also wise to make a personalized plan with your doctor to manage and prevent crises.
By focusing on preventive care, people with sickle cell disease can live healthier lives and lower the risk of serious problems. It’s vital to work closely with healthcare providers to create a care plan that fits your needs.
Lifestyle Modifications for Better Disease Management
Managing sickle cell disease well means making big changes in your life. By changing your daily habits, you can handle your disease better. This can make your life much better.
Nutrition, Hydration, and Diet
Eating a balanced diet is key for sickle cell disease patients. Drinking enough water helps prevent dehydration, which can lead to crises. Eating foods like fruits, veggies, whole grains, and lean proteins is good.
Stay away from foods that can make you dehydrated or worsen symptoms. Drink lots of water all day to manage your disease well.
Safe Physical Activity Guidelines
Exercising regularly can boost your health and lower disease risks. But, it’s important to follow safe exercise rules to avoid crises. Safe activities include walking, swimming, and yoga.
Listen to your body and don’t push too hard. Stay cool and hydrated while exercising to avoid crises.
Avoiding Environmental Triggers
Some environmental factors can cause sickle cell crises. Avoid extreme temperatures and high altitudes to prevent crises. Also, avoid hard activities in hot weather.
- Stay indoors during extreme weather.
- Dress right for the weather.
- Avoid sudden environment changes.
Stress Management Techniques
Stress can make sickle cell disease symptoms worse. Stress management like meditation, deep breathing, and yoga can help.
Doing things you enjoy and having a support network can also help. Building a support network of loved ones and groups can offer emotional support and help manage stress.
By making these lifestyle changes, people with sickle cell disease can manage their condition better. This can reduce crises and improve their quality of life.
Special Considerations for Children with Sickle Cell Disease
Caring for kids with sickle cell disease needs a full approach. This includes medical, educational, and mental health support. It’s vital to meet their unique needs to help them live healthy, happy lives.
Pediatric Treatment Protocols
Pediatric treatment plans for sickle cell disease aim to manage symptoms and prevent problems. Hydroxyurea is a key medicine that helps reduce pain crises and may lower the risk of other issues. Regular health checks and vaccines are also crucial to fight off infections.
“Early action and steady care can greatly improve life for sickle cell kids,” a study on pediatric care says. This shows the importance of being proactive in their care.
Educational Accommodations and Support
Kids with sickle cell disease might need special help in school. This could mean individualized education plans (IEPs) for flexible schedules, extra time, and medical care during school. We support these plans to help kids stay on track with their classmates.
- Regular talks between parents, teachers, and doctors
- Help with homework or tutoring when needed
- A safe and supportive school setting
Transitioning to Adult Care
As kids with sickle cell disease grow up, moving to adult care is essential. This means teaching them to manage their health on their own, finding a doctor who specializes in sickle cell, and keeping care consistent. A smooth transition is crucial for their health and happiness.
By focusing on these special needs, we can help kids with sickle cell disease thrive. It’s a team effort that needs coordination from healthcare, education, and families.
Pregnancy and Family Planning with Sickle Cell Disease
Women with sickle cell disease face special challenges during pregnancy. They need careful care to reduce risks and ensure a healthy baby and mom.
Pre-conception Counseling and Planning
Before getting pregnant, women with sickle cell disease should get pre-conception counseling. This step helps understand the risks and plan for pregnancy care. Key components of pre-conception counseling include:
- Reviewing current medications and adjusting them as necessary to ensure safety during pregnancy
- Assessing overall health and managing any complications related to sickle cell disease
- Discussing genetic counseling to understand the risk of passing sickle cell disease to the offspring
- Planning for prenatal care with a healthcare provider experienced in managing high-risk pregnancies and sickle cell disease
Managing Sickle Cell During Pregnancy
Managing sickle cell disease during pregnancy requires teamwork. Key strategies include:
- Regular prenatal check-ups to monitor the health of both mother and fetus
- Adjusting treatment plans as needed to manage pain and prevent complications
- Monitoring for signs of sickle cell crisis and having a plan in place for emergency situations
- Maintaining a healthy lifestyle, including a balanced diet and adequate hydration
Delivery and Postpartum Considerations
Women with sickle cell disease need a special delivery plan. This plan should be made with a team of healthcare experts. Postpartum care is equally important, focusing on:
- Monitoring for postpartum complications, including infections and sickle cell crises
- Managing pain effectively
- Providing support for breastfeeding, if desired, while managing medications
- Ensuring follow-up care with both obstetric and hematology teams
By working together, women with sickle cell disease can have a safe and successful pregnancy.
Navigating Health Insurance and Treatment Costs
Treating sickle cell disease can be expensive. It’s key to know your health insurance and financial help options. Understanding these can help manage the costs of care.
Insurance Coverage for Sickle Cell Treatments
Knowing your health insurance is vital for sickle cell disease treatment costs. Most plans cover treatments like:
- Medications such as hydroxyurea and L-glutamine
- Blood transfusions
- Hospital stays for sickle cell crises
- Some alternative therapies under certain conditions
Review your policy to see what’s covered, what you’ll pay out-of-pocket, and if your doctor is in-network.
Patient Assistance Programs
Patient assistance programs (PAPs) are crucial for many. They offer help with medications and treatments. These programs come from companies, non-profits, and government agencies.
Key things about PAPs include:
- Eligibility criteria, like income and insurance status
- Application processes, which differ by program
- The types of help, like free or discounted meds
Advocating for Coverage of New Therapies
New therapies, like gene therapy, need insurance coverage. Patients and families can help by:
- Keeping up with new treatments and coverage
- Talking to healthcare providers and insurance
- Joining advocacy groups for better coverage
By understanding insurance, using PAPs, and pushing for new therapy coverage, sickle cell patients can manage treatment costs better.
Finding Specialized Sickle Cell Disease Care
Managing sickle cell disease needs specialized care to improve life quality. This care includes services and expertise for sickle cell disease needs.
Sickle Cell Centers of Excellence
Sickle Cell Centers of Excellence offer comprehensive care for sickle cell disease. They have a team of healthcare experts in managing the disease.
Key features of these centers include:
- Multidisciplinary care teams with expertise in hematology, pain management, and other relevant specialties
- Access to the latest treatments and clinical trials
- Comprehensive support services, including counseling and patient education
- Coordination of care with other healthcare providers
Building Your Healthcare Team
Creating a strong healthcare team is key for sickle cell disease management. This team should have experts in different areas of the disease.
A typical healthcare team for sickle cell disease includes:
| Healthcare Professional | Role |
| Hematologist | Specializes in the diagnosis and treatment of blood disorders, including sickle cell disease |
| Pain Management Specialist | Helps manage acute and chronic pain associated with sickle cell disease |
| Primary Care Physician | Provides general medical care and coordinates with specialists |
Telemedicine Options for Sickle Cell Management
Telemedicine is a valuable tool for managing sickle cell disease. It’s especially helpful for those who find it hard to get in-person care.
Telemedicine offers several benefits for sickle cell disease management:
- Increased access to care, particularly for rural or underserved populations
- Reduced need for hospital visits, minimizing the risk of infections and other complications
- Enhanced patient engagement through regular monitoring and follow-up
- Flexibility in scheduling appointments, accommodating the unpredictable nature of sickle cell disease
By using telemedicine, patients with sickle cell disease can get timely and effective care. This improves their overall quality of life.
Conclusion: Living Well with Sickle Cell Disease
Living with sickle cell disease needs a mix of medical care, lifestyle changes, and support services. This guide has covered many parts of managing the disease. We’ve looked at diagnosis, treatments, preventive care, and how to live better with it.
Managing sickle cell disease well is key to a better life for those with it. A complete care plan helps patients deal with the disease’s challenges. It also lowers the chance of serious problems. We’re dedicated to top-notch healthcare and support for patients from around the world.
Knowing the value of full care and support helps those with sickle cell disease. They can take steps to manage their condition and improve their health.
FAQ
What is sickle cell disease?
Sickle cell disease is a genetic disorder. It affects how red blood cells make hemoglobin. This makes the cells misshapen and break down.
How is sickle cell disease diagnosed?
Doctors use newborn screening, blood tests, and genetic testing to diagnose it. They look for the abnormal hemoglobin gene.
What are the symptoms of sickle cell disease?
Symptoms include pain episodes, anemia, infections, and organ damage. People may also have sickle cell crisis and acute chest syndrome.
How is sickle cell disease treated?
Treatment includes medications like hydroxyurea, pain management, and blood transfusions. Sometimes, bone marrow or stem cell transplantation is used.
What is hydroxyurea, and how does it help in managing sickle cell disease?
Hydroxyurea reduces painful crises and may lower blood transfusion needs. It increases fetal hemoglobin production.
Can sickle cell disease be cured?
Bone marrow or stem cell transplantation is the only cure. But, it’s risky and needs a compatible donor.
What are the benefits and risks of blood transfusions in sickle cell disease?
Transfusions increase normal red blood cells, reducing complications. But, they can cause iron overload, which needs careful management.
How can pain be managed in sickle cell disease?
Pain management uses medications and non-pharmacological approaches. It also includes physical therapy and psychological support for both acute and chronic pain.
What lifestyle changes can help manage sickle cell disease?
Eating a healthy diet, staying hydrated, and avoiding extreme temperatures help. Managing stress and safe physical activities are also important.
Are there any new treatments on the horizon for sickle cell disease?
Yes, gene therapy is being researched. Clinical trials are looking into its safety and effectiveness.
How can families navigate health insurance for sickle cell disease treatments?
Families should check their insurance, look into patient assistance programs, and fight for coverage of new therapies.
What is the importance of finding specialized care for sickle cell disease?
Specialized care from sickle cell centers and a comprehensive team improves management. It also enhances quality of life.
Can people with sickle cell disease lead normal lives?
Yes, with proper management, including medication and lifestyle adjustments, many lead active and fulfilling lives.
References
- World Health Organization. (2025, August 6). Sickle-cell disease. Retrieved from https://www.who.int/news-room/fact-sheets/detail/sickle-cell-disease



































