sickle cell disease symptoms
Sickle Cell Disease (SCD) is a genetic disorder that affects how red blood cells carry oxygen. It makes these cells take on a sickle shape. This shape can cause serious health problems, like severe pain and infections. The Centers for Disease Control and Prevention (CDC) says SCD affects about 100,000 people in the United States.
Knowing the symptoms of Sickle Cell Disease is key to managing it well. We’ll look at how SCD shows itself, including sickle cell crisis. We’ll also see how spotting these signs can help people with SCD live better lives.
Key Takeaways
- Sickle Cell Disease is a genetic disorder affecting hemoglobin production.
- Abnormally shaped red blood cells can cause pain episodes and infections.
- Recognizing symptoms is crucial for effective management of SCD.
- Understanding SCD symptoms can lead to better health outcomes.
- Sickle Cell Disease affects approximately 100,000 people in the U.S.
Understanding Sickle Cell Disease
Sickle Cell Disease red blood cells
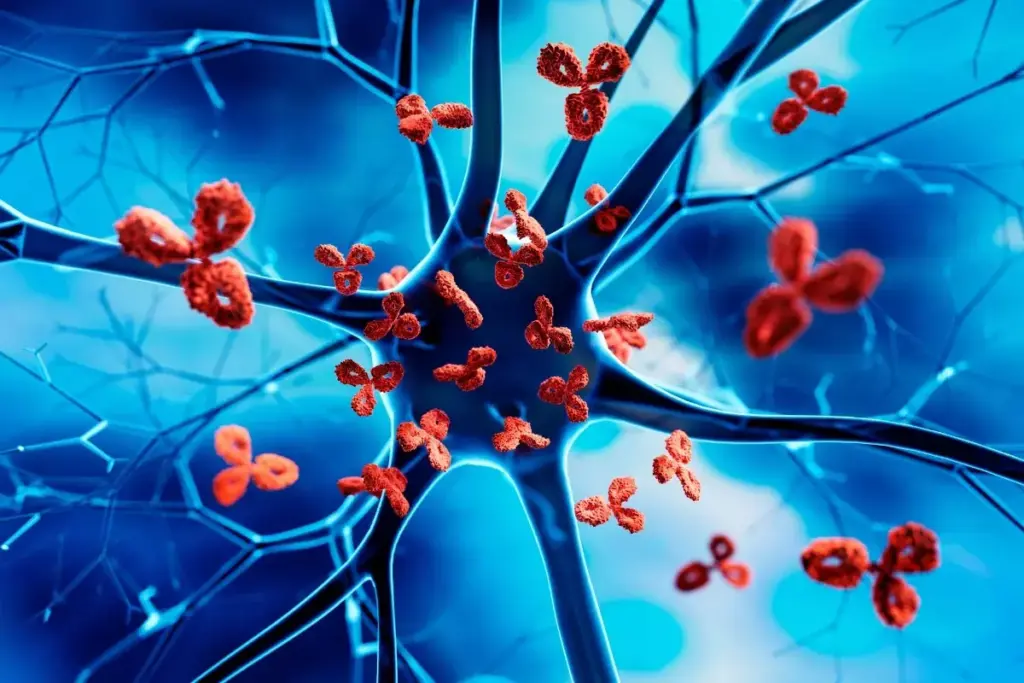
Sickle Cell Disease (SCD) is a genetic disorder that affects how red blood cells make hemoglobin. It’s caused by a mutation in the HBB gene. This mutation leads to the creation of abnormal hemoglobin, known as sickle hemoglobin or HbS.
What Is Sickle Cell Disease?
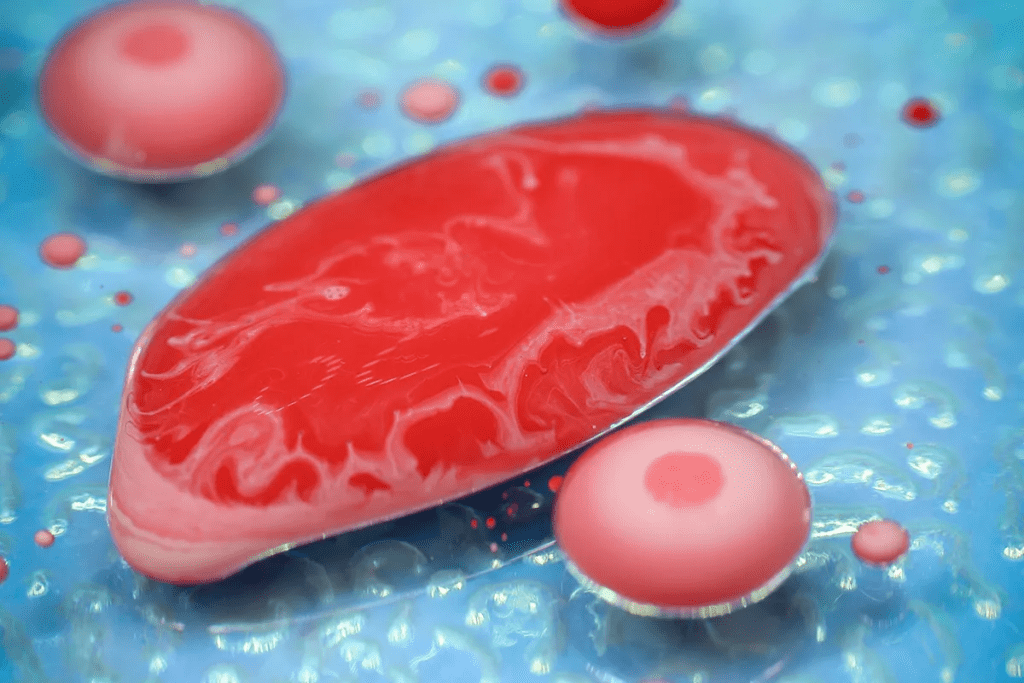
Sickle Cell Disease makes red blood cells take on a sickle shape under certain conditions. These sickled cells are less flexible than normal cells. They can get stuck in small blood vessels, blocking blood flow.
The HBB gene mutation causes the production of abnormal hemoglobin. This abnormal hemoglobin makes red blood cells sickle. This sickling can cause health problems like pain episodes, infections, and anemia.
How Sickle Cell Disease Affects the Body
Sickle Cell Disease can harm many parts of the body. The sickling of red blood cells can cause vaso-occlusive crises. This leads to tissue ischemia and pain. It can also cause chronic anemia, increase the risk of infections, and lead to other complications.
The effects of Sickle Cell Disease on the body can be summarized as follows:
| System Affected | Possible Complications |
| Circulatory | Vaso-occlusive crises, anemia |
| Immune | Increased risk of infections |
| Skeletal | Bone pain, avascular necrosis |
The process of sickling and its impact on red blood cells can be illustrated as follows:
Medical professionals say, “Sickle Cell Disease is a complex condition that needs comprehensive care.” This shows the need for a detailed approach to treating SCD.
The Genetic Basis of Sickle Cell Disease
sickle cell disease inheritance pattern
Sickle Cell Disease comes from a mutation in the HBB gene. This gene codes for a part of hemoglobin. The mutation creates abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
The disease follows an autosomal recessive pattern. This means a person needs two defective HBB genes to have the disease. We’ll look into this pattern more and talk about what it means to carry the sickle cell gene.
Inheritance Patterns
In autosomal recessive inheritance, the disease shows up with two mutated genes. Carriers have one normal and one mutated gene. They usually don’t show symptoms but can pass the mutated gene to their kids.
If both parents are carriers, there’s a 25% chance their child will have Sickle Cell Disease. There’s a 50% chance the child will be a carrier. And a 25% chance the child won’t have the disease or be a carrier.
Difference Between Sickle Cell Trait and Disease
It’s important to know the difference between Sickle Cell Trait (SCT) and Sickle Cell Disease (SCD). People with SCT carry the sickle cell gene but don’t show symptoms most of the time. However, they might face health issues under extreme conditions.
Those with SCD have two sickle hemoglobin genes. They face serious health problems like pain, anemia, and infections.
Knowing the genetic basis of Sickle Cell Disease helps with counseling and managing the condition. We’ll keep exploring SCD, including its symptoms, complications, and how to manage them, in the next sections.
Types of Sickle Cell Disease
types of sickle cell disease
It’s important to know the different types of Sickle Cell Disease to manage it well. Sickle Cell Disease (SCD) is a group of genetic disorders that affect how red blood cells make hemoglobin. Each type of SCD has a different mutation in the HBB gene, leading to abnormal hemoglobin.
Hemoglobin SS Disease
Hemoglobin SS Disease, or HbSS, is the most common and severe form of SCD. It happens when someone gets two mutated HBB genes, one from each parent. This leads to hemoglobin S, causing red blood cells to sickle under certain conditions. People with HbSS often have frequent pain, anemia, and are more likely to get infections.
Hemoglobin SC Disease
Hemoglobin SC Disease, or HbSC, is another significant form of SCD. It’s caused by getting one mutated HBB gene for hemoglobin S and another for hemoglobin C. While HbSC is milder than HbSS, it can still cause serious health problems, like vaso-occlusive crises and splenic sequestration.
Hemoglobin S Beta Thalassemia
Hemoglobin S Beta Thalassemia happens when someone gets one mutated HBB gene for hemoglobin S and another for beta thalassemia. The severity can vary a lot, depending on the mutations. Some people might have mild symptoms, while others face more severe issues.
Other Rare Types
There are other rare types of SCD, like Hemoglobin SD Disease and Hemoglobin SE Disease, among others. These are less common and can have different levels of severity. Getting an accurate diagnosis through genetic testing is key to understanding the specific type of SCD and creating a proper management plan.
In conclusion, Sickle Cell Disease comes in different types, each with its own genetic cause, severity, and symptoms. Knowing these differences is vital for effective care and support for those affected.
Sickle Cell Disease Symptoms
sickle cell disease symptoms
Knowing the symptoms of Sickle Cell Disease is key to managing it well. This genetic disorder affects how red blood cells make hemoglobin. It leads to several health issues.
Pain Episodes (Vaso-occlusive Crisis)
Pain episodes, or vaso-occlusive crises, are a major symptom. They happen when sickled red blood cells block blood vessels. This causes pain and tissue damage.
The pain can be very bad and unpredictable. It can change in how bad it is and how long it lasts.
Anemia and Related Symptoms
Anemia is a common symptom too. It’s caused by red blood cells being destroyed early. This leads to feeling tired, weak, and short of breath.
Anemia symptoms can really affect a person’s quality of life.
| Symptom | Description | Impact on Patient |
| Pain Episodes | Severe pain due to vaso-occlusion | Significant discomfort, potential for hospitalization |
| Anemia | Low red blood cell count | Fatigue, weakness, shortness of breath |
| Fatigue and Weakness | Reduced energy levels | Impact on daily activities and quality of life |
| Jaundice | Yellowing of the skin and eyes | Visible symptom, potential for liver complications |
Fatigue and Weakness
Fatigue and weakness are common in Sickle Cell Disease patients. They are mainly due to anemia. These symptoms make it hard to do daily tasks and affect overall well-being.
Jaundice and Yellowing of the Eyes
Jaundice, or yellowing of the skin and eyes, is a clear sign of Sickle Cell Disease. It happens when red blood cells break down, causing bilirubin to build up.
Managing these symptoms is vital for improving life quality for those with Sickle Cell Disease. Understanding these symptoms helps healthcare providers give better care and support.
Age-Related Symptoms of Sickle Cell Disease
age-related symptoms of Sickle Cell Disease
It’s key to know how Sickle Cell Disease changes with age. From infancy to adulthood, the symptoms shift, bringing unique challenges at each life stage.
Symptoms in Infants and Young Children
Infants and young kids with Sickle Cell Disease show different signs than older kids and adults. They might have anemia, jaundice, and swelling in the hands and feet. These signs can be hard on young patients and their families.
They also get sick more often because their immune system is weak. We need to watch them closely to stop problems and act fast when needed.
Symptoms in Older Children and Adolescents
Older kids with Sickle Cell Disease have pain episodes more often. These can be caused by dehydration, cold, or stress. They might also grow slower than their peers.
Healthcare teams must work with families to handle these symptoms. This helps keep these young patients healthy and happy.
Symptoms in Adults
Adults with Sickle Cell Disease face serious issues like chronic pain, organ damage, and more infections. It can also make it hard for them to work and live their daily lives.
We stress the need for ongoing care to lessen these problems. This helps improve the lives of adults with Sickle Cell Disease.
Acute Complications and Their Symptoms
acute chest syndrome
Managing Sickle Cell Disease is tough because of acute complications. These can be deadly and need quick medical help. We’ll talk about the acute complications of Sickle Cell Disease, their symptoms, and why urgent care is essential.
Acute Chest Syndrome
Acute chest syndrome is a big problem for people with Sickle Cell Disease. It causes a new lung issue, fever, breathing problems, or chest pain. Quick action and treatment are key to avoiding serious problems.
Splenic Sequestration
Splenic sequestration happens when red blood cells get stuck in the spleen. This makes the spleen big and lowers hemoglobin levels fast. It’s very serious and needs quick medical help. Symptoms include severe anemia, belly pain, and a big spleen.
Stroke and Neurological Symptoms
Stroke is a big risk for people with Sickle Cell Disease, especially kids. Symptoms can be mild or severe, like weakness, speech issues, and vision problems. Quick detection and treatment are crucial to avoid lasting damage.
Priapism
Priapism is a long-lasting erection that’s not caused by sex. It’s a Sickle Cell Disease complication that can cause permanent harm if not treated fast. It’s very painful and needs urgent medical care.
Chronic Complications and Their Symptoms
chronic complications of Sickle Cell Disease
Sickle Cell Disease can cause many chronic problems that affect different parts of the body. These issues can really change how well someone can live with the disease.
Organ Damage
Organ damage is a big problem for people with Sickle Cell Disease. The disease can hurt organs like the spleen, kidneys, and liver. The spleen is especially at risk because it helps clean the blood.
Here’s a list of possible organ damage:
| Organ | Complication | Symptoms |
| Spleen | Autosplenectomy | Increased risk of infections |
| Kidneys | Chronic kidney disease | Proteinuria, hematuria |
| Liver | Cholestasis, liver failure | Jaundice, abdominal pain |
Growth and Development Issues
Children with Sickle Cell Disease might grow and develop slower. This is because of chronic anemia and not getting enough nutrients. Regular monitoring and nutritional support are key to helping them catch up.
Skin Ulcers
Skin ulcers are painful and can happen around the ankles. They happen when blood flow to the skin is cut off. Proper wound care and management are important to stop infections and help them heal.
Eye Problems
Eye problems, like proliferative sickle retinopathy, can cause vision loss. It’s important to get regular eye exams. This helps catch and treat problems early to avoid serious vision loss.
Knowing about these chronic complications helps us manage Sickle Cell Disease better. This way, we can improve the lives of those affected.
Understanding Sickle Cell Crisis
A sickle cell crisis is a serious condition that happens in people with sickle cell disease. It causes severe pain and can be very dangerous. Knowing what triggers and symptoms of a sickle cell crisis are is very important for managing the condition.
Many things can start a sickle cell crisis. These include dehydration, infections, and extreme temperatures. When these things happen, sickled red blood cells can block small blood vessels. This can cause tissue ischemia and severe pain.
Triggers of Sickle Cell Crisis
It’s important to know what can start a sickle cell crisis. Common triggers include:
- Dehydration, which can make the blood more likely to sickle
- Infections, which can cause inflammation and increase the risk of a crisis
- Extreme temperatures, either hot or cold, which can affect blood flow and trigger a crisis
- Physical stress or overexertion
Symptoms of Sickle Cell Crisis
The symptoms of a sickle cell crisis can vary. But they usually include severe pain in the bones, chest, or abdomen. Other symptoms may include:
- Pain that is sudden and severe
- Fever or chills
- Nausea or vomiting
- Shortness of breath
Duration and Severity
The length and how bad a sickle cell crisis is can differ a lot. Some crises may go away in a few days, but others can last longer and need hospital care. The crisis’s severity often depends on the person’s health and how quickly they get medical help.
Knowing how long and how severe a sickle cell crisis can be is key to managing it well. This helps lower the chance of serious long-term problems.
Pain Management in Sickle Cell Disease
For those with Sickle Cell Disease, pain management is more than just relief. It’s about improving their overall well-being. Good pain management helps patients live better, more active lives.
Types of Pain in Sickle Cell Disease
Sickle Cell Disease causes different kinds of pain. Most pain comes from vaso-occlusive crises. This happens when sickled red blood cells block blood vessels, causing pain and tissue damage.
- Acute Pain: This pain starts suddenly and can be very severe. It’s often due to vaso-occlusive events.
- Chronic Pain: This pain lasts a long time. It can be caused by ongoing inflammation, organ damage, or other issues.
- Neuropathic Pain: This pain is from nerve damage. It’s a complication of Sickle Cell Disease.
Acute vs. Chronic Pain
It’s important to know the difference between acute and chronic pain. Acute pain is sudden and severe, often from vaso-occlusive crises. Chronic pain lasts longer and can be from organ damage or other issues.
Pain Assessment Strategies
Getting pain right is key to managing it well. Doctors use tools like pain scales and pain diaries to assess pain. They also look at the pain’s location, intensity, and how long it lasts.
- Pain scales (e.g., numeric rating scale, faces pain scale)
- Pain diaries or journals
- Clinical evaluation of pain characteristics (location, intensity, duration)
Home Management Techniques
At home, managing pain involves medicine and non-medicine ways. Medicine includes NSAIDs or opioids, as doctors prescribe. Non-medicine ways include staying hydrated, using heat or cold, and practicing relaxation techniques.
- Hydration and maintaining fluid balance
- Heat or cold therapy
- Relaxation techniques (e.g., deep breathing, meditation)
- Physical therapy and gentle exercises
Understanding Sickle Cell Disease pain and using good pain management can help people cope better. It can also improve their quality of life.
Diagnosing Sickle Cell Disease
Diagnosing Sickle Cell Disease involves several steps. These include screening tests and genetic analysis. Accurate diagnosis is key to managing the disease well.
Newborn Screening
Newborn screening is vital for catching Sickle Cell Disease early. It uses a simple blood test, done when the baby is 24 to 48 hours old.
This early detection helps start treatment quickly. It can greatly improve the baby’s health.
Blood Tests and Genetic Testing
Blood tests look for abnormal hemoglobin. The most common is hemoglobin electrophoresis. It separates hemoglobin types by electrical charge.
Genetic testing confirms the disease by finding the genetic mutation. It’s helpful when the diagnosis is unsure.
| Test Type | Purpose | Benefits |
| Hemoglobin Electrophoresis | Identify abnormal hemoglobin | Accurate diagnosis |
| Genetic Testing | Confirm genetic mutation | Certain diagnosis, family planning |
Prenatal Diagnosis
Pregnant women can get prenatal diagnosis for Sickle Cell Disease. CVS or amniocentesis can check if the fetus is affected.
“Prenatal diagnosis provides expectant parents with crucial information about the health of their baby, allowing them to make informed decisions about their pregnancy.”
Differential Diagnosis
Differential diagnosis is about telling Sickle Cell Disease apart from other similar conditions. It involves a detailed check-up, including medical history and tests.
Treatment Options for Sickle Cell Disease Symptoms
Managing Sickle Cell Disease (SCD) needs a mix of treatments to ease symptoms and prevent problems. We’ll look at how to manage SCD symptoms, making life better for those affected.
Medications
Medicines are key in treating SCD symptoms. Hydroxyurea is often used to lessen pain episodes and reduce blood transfusion needs. Other drugs help with pain, infections, and other SCD issues.
We use pain meds, from over-the-counter to prescription, based on pain level. We also give medicines to prevent infections and other SCD complications.
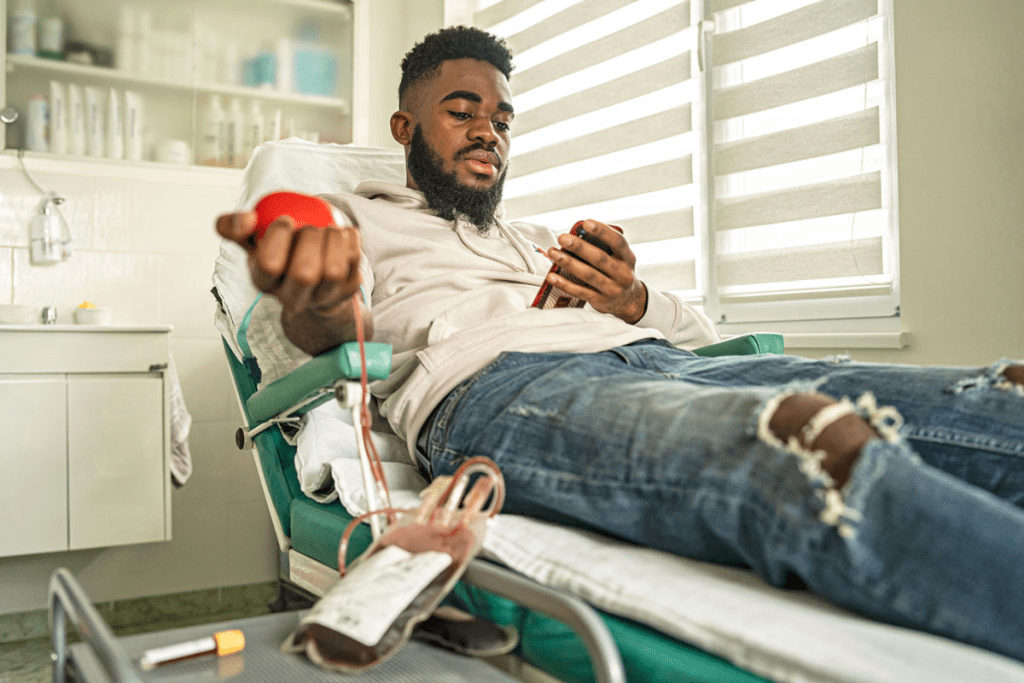
Blood Transfusions
Blood transfusions are vital in SCD care. They increase normal red blood cells, helping avoid serious issues like anemia and stroke.
There are simple and exchange transfusions for SCD. Exchange transfusions replace sickled cells with donor cells.
Stem Cell Transplantation
Stem cell transplantation is the only cure for SCD. It replaces the patient’s marrow with healthy donor marrow. Though risky, it’s considered for severe cases.
This process is complex, needing a perfect donor match to avoid complications. Advances are making it safer for more patients.
Emerging Therapies
New treatments give hope for SCD management. Gene therapy aims to fix the genetic issue causing SCD. New meds also help manage symptoms and prevent complications.
SCD treatment is evolving fast, with many promising therapies in trials. These could change how we treat SCD, offering better, more targeted options.
Living with Sickle Cell Disease
Living with sickle cell disease means making lifestyle changes and getting preventive care. It also means finding support resources. These steps can greatly improve life for those with the disease.
Lifestyle Modifications
Changing your lifestyle can help manage sickle cell disease symptoms. Staying hydrated is key, as dehydration can cause crises. Drink lots of water and avoid extreme temperatures.
Eating a balanced diet with fruits, veggies, and whole grains is also important. Regular, low-impact exercises like walking or swimming are good. Getting enough rest and using stress-reducing techniques like meditation can also help.
Preventive Care
Preventive care is crucial for managing sickle cell disease. Regular health check-ups can catch problems early. Vaccinations are also important, as sickle cell patients are more prone to infections.
Psychological Impact
Sickle cell disease can affect mental health, not just physically. The chronic nature and unpredictable crises can lead to anxiety and depression. Mental health support is key to managing these feelings.
Counseling or therapy can help manage emotional challenges. Support groups, online or in-person, offer a sense of community. They help reduce feelings of isolation.
Support Resources
Access to the right support can greatly improve life with sickle cell disease. This includes medical, educational, financial, and social support. Patient advocacy organizations provide valuable information and connections.
Family members and caregivers also need support. They play a big role in managing the disease. Educational programs and support groups for families can help them understand and support themselves better.
When to Seek Medical Attention
People with Sickle Cell Disease need to know when to get medical help fast. Spotting these signs early can stop serious problems and make treatment better.
Emergency Warning Signs
Some symptoms mean you need to see a doctor right away. These include:
- Severe pain not relieved by home treatment
- Shortness of breath or trouble breathing
- Chest pain or feeling tight in the chest
- Severe headache or feeling confused
- Weakness or numbness in the face, arm, or leg
Symptoms Requiring Immediate Care
Even small symptoms can be serious and need quick doctor visits. These include:
- Fever over 101.5 °F (38.6 °C)
- Pain that’s different or worse than usual
- Swelling or redness in the hands or feet
- Jaundice or yellow eyes
Regular Monitoring Guidelines
Keeping an eye on your health is key for managing Sickle Cell Disease. We suggest:
- Regular visits to your healthcare provider
- Keeping a record of your symptoms and pain
- Staying current on vaccinations
- Living a healthy lifestyle, including a balanced diet and enough water
| Symptom | Action |
| Severe pain | Seek immediate medical attention |
| Fever above 101.5 °F | Seek immediate medical attention |
| Shortness of breath | Seek immediate medical attention |
“Quickly spotting emergency signs and regular check-ups can greatly improve life for those with Sickle Cell Disease.”
A Hematologist
Conclusion
Managing Sickle Cell Disease (SCD) well means understanding it, knowing its symptoms, and getting the right care. We’ve looked at SCD’s genetic roots, its types, and the symptoms people face.
Living with SCD needs ongoing support and quick medical help. Knowing when to get medical help is key. Treatments like medicines, blood transfusions, and new therapies help manage symptoms and prevent problems.
Effective SCD management also means making lifestyle changes and preventive care. A healthy lifestyle and staying up-to-date with treatments help people with SCD live well. We stress the need for awareness and support for those with SCD, so they can thrive.
FAQ
What is Sickle Cell Disease?
Sickle Cell Disease (SCD) is a genetic disorder that affects how red blood cells are made. It causes these cells to be abnormally shaped. This can lead to health issues like pain episodes and a higher risk of infections.
How is Sickle Cell Disease inherited?
SCD is inherited in an autosomal recessive pattern. This means a person needs two abnormal HBB genes, one from each parent, to have the disease. Carriers have one normal and one abnormal gene. They usually don’t show all the symptoms but can pass the abnormal gene to their kids.
What are the symptoms of Sickle Cell Disease?
Symptoms include pain episodes, anemia, fatigue, jaundice, and yellow eyes. How often and how severe these symptoms are can vary a lot among people with SCD.
What is a Sickle Cell Crisis?
A Sickle Cell Crisis happens when sickled red blood cells block small blood vessels. This causes tissue ischemia and pain. Crises can be triggered by dehydration, infection, and extreme temperatures.
How is Sickle Cell Disease diagnosed?
Diagnosis is usually through newborn screening, blood tests, and genetic testing. Prenatal diagnosis is also available for pregnant individuals.
What are the treatment options for Sickle Cell Disease?
Treatments include medications for pain and preventing complications, blood transfusions, stem cell transplantation in some cases, and new therapies to modify the disease.
How can pain be managed in Sickle Cell Disease?
Pain management uses medicines and non-medical strategies. This includes analgesics, staying hydrated, resting, and alternative therapies like heat therapy. Good pain management is key to a better quality of life.
What lifestyle modifications can help manage Sickle Cell Disease?
People with SCD should stay hydrated, avoid extreme temperatures, get regular vaccinations, eat healthily, and avoid activities that can trigger crises. Regular monitoring and preventive care are also important.
When should medical attention be sought for Sickle Cell Disease?
Seek medical help right away for severe pain, trouble breathing, fever, or signs of infection. Regular check-ups and follow-up care are also crucial for managing complications.
Are there support resources available for individuals with Sickle Cell Disease?
Yes, there are many support resources like patient organizations, counseling services, and support groups. These offer valuable information, emotional support, and guidance on managing the disease.
References
- National Heart, Lung, and Blood Institute. (2022, July 15). Sickle Cell Disease: Symptoms. National Institutes of Health. https://www.nhlbi.nih.gov/health/sickle-cell-disease/symptoms
- Kato, G. J., Piel, F. B., Reid, C. D., Gaston, M. H., Ohene-Frempong, K., Krishnamurti, L., Smith, W. R., Panepinto, J. A., Weatherall, D. J., Costa, F. F., & Vichinsky, E. P. (2018). Sickle cell disease. Nature Reviews Disease Primers, *4*, 18010. https://www.nature.com/articles/nrdp201810
- National Human Genome Research Institute. (2024, April 17). About Sickle Cell Disease. https://www.genome.gov/Genetic-Disorders/Sickle-Cell-Disease