Last Updated on October 21, 2025 by mcelik

Every year, thousands of babies are born with sickle cell disease. This condition affects the hemoglobin in red blood cells. Now, prenatal testing can find this genetic disorder early in pregnancy. This gives parents important information about their baby’s health.Learn about the sickle cell disease test for babies, how prenatal testing works, and how parents can detect sickle cells before birth.
At our institution, we know how vital early detection and support are for families with sickle cell disease. Our genetic testing services give accurate and reliable results. This helps parents make informed decisions about their care.
We will talk about prenatal testing for sickle cell disease. We’ll cover the testing options, their benefits, and what to expect during the process.
Key Takeaways
- Prenatal testing can detect sickle cell disease early in pregnancy.
- Genetic testing provides accurate and reliable results.
- Early detection enables informed decision-making for families.
- Comprehensive support is available for families affected by sickle cell disease.
- Advanced testing services are key for managing the condition.
Understanding Sickle Cell Disease and Its Genetic Basis

It’s important to know the genetic basis of sickle cell disease. This knowledge helps in managing the condition. Sickle cell disease is a genetic disorder that affects hemoglobin production. Hemoglobin is a protein in red blood cells that carries oxygen.
What Is Sickle Cell Disease?
Sickle cell disease is caused by abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S. This abnormality makes red blood cells sickle-shaped, mainly when oxygen levels are low. The sickling of red blood cells leads to their early destruction and can cause them to get stuck in small blood vessels. This results in various health problems.
The Genetic Mutation Behind Sickle Cell Disease
The genetic mutation behind sickle cell disease is in the HBB gene. This gene provides instructions for making the beta-globin subunit of hemoglobin. A single point mutation in this gene causes the production of the abnormal beta-globin chain. This chain, when combined with normal alpha-globin chains, forms hemoglobin S. The mutation is inherited in an autosomal recessive pattern. This means a person must inherit two defective HBB genes (one from each parent) to have the disease.
Inheritance Patterns of Sickle Cell Disease
Understanding the inheritance pattern of sickle cell disease is key. When both parents are carriers of the mutated HBB gene, there’s a 25% chance with each pregnancy that the child will have sickle cell disease. There’s a 50% chance that the child will be a carrier like each parent. And there’s a 25% chance that the child will neither have the disease nor be a carrier.
| Parent 1 | Parent 2 | Chance of Child Having Sickle Cell Disease | Chance of Child Being a Carrier | Chance of Child Not Being Affected |
| Carrier | Carrier | 25% | 50% | 25% |
| Carrier | Not a Carrier | 0% | 50% | 50% |
| Has Sickle Cell Disease | Carrier | 50% | 50% | 0% |
Understanding sickle cell disease’s genetic basis and inheritance patterns helps families. It allows them to better navigate risks and make informed health decisions.
Sickle Cell Disease vs. Sickle Cell Trait: Important Distinctions
It’s key to know the difference between sickle cell disease and sickle cell trait. Both are linked to the sickle cell gene but have different health effects and management needs.
Defining Sickle Cell Trait
Sickle cell trait happens when someone has one normal and one sickle hemoglobin gene. They carry the sickle cell gene but usually don’t show all the disease symptoms. Yet, they can pass the gene to their kids.
People with sickle cell trait often live normal lives without major health problems. But, they might face issues in high places or when they’re very active.
Health Implications of Sickle Cell Trait vs. Disease
Sickle cell disease is much more serious than sickle cell trait. It happens when someone has two sickle hemoglobin genes. This causes long-term anemia, pain episodes, and a higher risk of infections and other problems.
On the other hand, sickle cell trait carriers usually don’t have symptoms but can pass the gene to their children. Knowing your status is vital, mainly when planning a family, as you might pass the gene to your kids.
Getting tested for sickle cell trait is important, mainly for family planning and understanding health risks. A simple blood test can show if you carry the sickle cell gene.
The Importance of Prenatal Screening for Sickle Cell Disease
The role of prenatal screening for sickle cell disease is huge. It helps make big decisions about how to care for a baby during pregnancy. This screening is key for parents to know if their baby might have sickle cell disease.
Why Early Detection Matters
Getting a diagnosis early through prenatal screening helps families plan better. It lets them get the right care for their baby. This can really help the baby’s health.
“Early diagnosis and complete care can greatly improve life for kids with sickle cell disease.”
Also, finding out early means starting treatments sooner. This is very important for managing the disease’s problems.
Who Should Consider Prenatal Screening
People with a family history of sickle cell disease should get screened. Those from African, Caribbean, Middle Eastern, Indian, and Mediterranean backgrounds are at higher risk. Genetic counseling can help understand the disease’s risks and what it means.
- Families with a history of sickle cell disease or trait
- Individuals from high-risk ethnic backgrounds
- Couples who are carriers of the sickle cell gene
Risk Factors and Family History Considerations
A family history of sickle cell disease is a big risk. If both parents carry the sickle cell gene, their child is more likely to have it. Knowing these risk factors helps make better choices about having children.
| Risk Factor | Description |
| Family History | A history of sickle cell disease in the family |
| Ethnic Background | Being of African, Caribbean, Middle Eastern, Indian, or Mediterranean descent |
| Carrier Status | Both parents being carriers of the sickle cell gene |
Understanding the value of prenatal screening for sickle cell disease helps families prepare. Early detection and good care can make a big difference. So, prenatal screening is a key part of caring for a baby during pregnancy.
Preconception Carrier Screening for Sickle Cell Disease
Preconception carrier screening is key for couples planning a family. It shows if they might pass sickle cell disease to their kids. This test finds carriers, even if they don’t have the disease.
Knowing if you’re a carrier helps couples plan their family. They can talk about genetic counseling or other ways to have a child.
Testing Before Pregnancy
Testing before pregnancy helps couples understand their genetic risks. A simple blood test checks for the sickle cell gene.
Early testing has many benefits: it helps make quick decisions, lowers stress, and opens up options if both are carriers.
Understanding Your Genetic Risk
If both parents carry the sickle cell gene, there’s a 25% chance of passing it to each child. Knowing this is key for planning a family.
Genetic counseling offers support and detailed info. It helps couples grasp their risks and what it means for their future kids.
Available Testing Options and Locations
Preconception carrier screening is available at many places. It usually involves a blood test to check for the sickle cell gene.
| Testing Option | Description | Location |
| Blood Test | Checks for the presence of the sickle cell gene | Local hospitals, clinics, and genetic testing laboratories |
| Genetic Counseling | Provides detailed information and support for carriers | Genetic counseling centers, hospitals, and online services |
| At-Home Testing Kits | Allows individuals to collect samples at home for lab analysis | Online retailers, some pharmacies |
It’s important to talk to a healthcare provider. They can help choose the best testing option based on your situation and health history.
First Trimester Screening Options for Sickle Cell Disease
Expectant parents have important screening options in the first trimester for sickle cell disease. These tests help find the disease early. They also give valuable info for managing the pregnancy.
Chorionic Villus Sampling (CVS)
Chorionic Villus Sampling, or CVS, is a prenatal test. It takes a small sample of cells from the placenta. These cells are checked for genetic issues, like sickle cell disease. CVS is done between the 10th and 13th weeks of pregnancy.
Benefits of CVS: It lets parents and doctors plan early for the baby’s care.
CVS is best for women with sickle cell disease in their family or who are carriers.
Cell-Free DNA Testing
Cell-Free DNA Testing is a non-invasive prenatal test. It looks at DNA in the mother’s blood for genetic conditions. It’s mainly for chromosomal issues but can also find single-gene disorders like sickle cell disease.
Advantages of Cell-Free DNA Testing: It’s safe for the fetus and can be done as early as 10 weeks.
Timing and Procedure Details
CVS and Cell-Free DNA Testing give early insights into the fetus’s health. CVS is usually done between weeks 10 and 13. Cell-Free DNA Testing is available from about the 10th week.
The choice between these tests depends on several factors. These include the risk of sickle cell disease, the mother’s health, and personal choices. Healthcare providers can help decide based on individual needs.
Knowing the options in the first trimester helps expectant parents make informed choices. Talking to a healthcare provider can help find the best way to detect sickle cell disease.
Second Trimester Diagnostic Tests for Sickle Cell Disease
The second trimester offers new ways to diagnose sickle cell disease. One key test is amniocentesis.
Amniocentesis Procedure
Amniocentesis takes a sample of amniotic fluid around the fetus. This fluid has cells that can show genetic issues, like sickle cell disease. The test is done between the 15th and 20th weeks of pregnancy.
Choosing to have amniocentesis is a big decision. It’s often suggested for women at risk of having a sickle cell disease child. This includes those with a family history or who tested positive early in pregnancy.
Interpreting Amniocentesis Results
Amniocentesis results can tell if the fetus has sickle cell disease. Our team will help you understand these results. This ensures you know about your baby’s health.
Understanding the results means knowing the fetus’s genetic makeup. The test can spot the sickle cell gene. This lets parents prepare for their child’s birth or explore other options.
Recovery and Follow-up Care
After amniocentesis, it’s important to follow recovery advice. Most women can go back to normal activities in a day or two.
We’re here to support you all through your pregnancy. If your baby has sickle cell disease, we’ll talk about what it means. We’ll also discuss how to ensure the best for your child.
Comprehensive Sickle Cell Disease Test Methods and Procedures
Diagnosing sickle cell disease requires several lab tests. These tests are key to finding sickle hemoglobin and understanding the disease’s genetics.
Hemoglobin Electrophoresis
Hemoglobin electrophoresis is a common test for sickle cell disease. It separates hemoglobin types by electrical charge. This helps spot abnormal hemoglobin, like sickle hemoglobin (HbS).
The test uses a blood sample on a gel or paper. An electric current makes the hemoglobin types move at different speeds. This creates bands that show if sickle cell disease or trait is present.
DNA Analysis for Sickle Cell Mutations
DNA analysis is precise for finding sickle cell disease’s genetic cause. It looks for the sickle cell gene in a blood or tissue sample.
This test is great for prenatal checks. It can be done on fetal cells from amniocentesis or CVS. This helps make early pregnancy decisions.
High-Performance Liquid Chromatography (HPLC)
High-Performance Liquid Chromatography (HPLC) is another advanced test for sickle cell disease. It separates and counts hemoglobin types based on their interaction with phases.
HPLC is very sensitive and can find and measure HbS and other abnormal hemoglobins. It’s often paired with other tests to confirm diagnosis and give detailed hemoglobin info.
Accuracy and Limitations of Prenatal Sickle Cell Testing
Knowing how accurate prenatal sickle cell testing is important for making good choices during pregnancy. This testing uses different methods, each with its own good and bad points.
Understanding Test Sensitivity and Specificity
The accuracy of prenatal sickle cell testing is based on its sensitivity and specificity. Sensitivity is how well the test finds people with the disease. Specificity is how well it finds people without the disease. Most tests are very good at both.
Tests like CVS and amniocentesis, followed by DNA analysis, are very accurate. But, how accurate they are can change based on when the test is done and the quality of the sample.
Potential for False Results
Even though prenatal sickle cell testing is very accurate, there’s a small chance of getting wrong results. A false negative is when the test misses the disease in a fetus that has it. A false positive is when the test says a fetus has the disease when it doesn’t. Errors in the lab, contaminated samples, or the timing of the test can cause these issues.
Healthcare providers should talk to parents about the chance of getting wrong results. They should explain what would happen if a wrong result is found. This might mean doing the test again or getting more tests to confirm the first one.
When Additional Testing May Be Needed
There are times when more testing is needed after the first prenatal sickle cell test. This could be if the first test wasn’t clear, if the test results don’t match what’s happening in the body, or if the test shows a need for more checking.
More testing can give more detailed info about the fetus’s health. This helps parents and doctors make better choices about the pregnancy. It might mean doing more genetic tests or other tests to understand how severe the condition is and plan the best care.
By knowing about the accuracy and limits of prenatal sickle cell testing, expectant parents can better understand the testing process. This helps them make informed choices about their pregnancy.
Risks and Costs Associated with Prenatal Sickle Cell Testing
Prenatal sickle cell testing is key to knowing your unborn baby’s health. But, it’s important to know the risks and costs. We’ll look at the risks, costs, and how to manage them.
Procedure-Related Risks
Testing for sickle cell disease in pregnancy comes with some risks. Chorionic villus sampling (CVS) and amniocentesis are tests that might cause miscarriage. It’s good to know about these risks.
CVS and amniocentesis take cells from the placenta or amniotic fluid. They check for genetic issues like sickle cell disease. Though rare, there could be infection, bleeding, or amniotic fluid leakage.
Finding Affordable Testing Options
If costs worry you, there are ways to make testing more affordable. Talk to your doctor about cheaper options. Some places offer financial help or lower fees based on income.
Genetic counseling can also help with insurance and finding cheaper tests. Look for local or national programs that offer free or low-cost testing for sickle cell disease.
Sickle Cell Disease and Thalassemia: Related Hemoglobinopathies
Sickle cell disease and thalassemia are complex genetic disorders. They affect how the body makes hemoglobin. Each has its own unique traits and needs for care.
Understanding Thalassemia
Thalassemia is a genetic disorder that affects hemoglobin production. It leads to anemia and other health issues. There are two main types: alpha-thalassemia and beta-thalassemia, each with different levels of severity.
We will look into how thalassemia is diagnosed and the differences between its types. Early diagnosis is key to managing the condition well.
Differences in Testing and Diagnosis
Thalassemia is tested through blood tests to check hemoglobin levels and types. Unlike sickle cell disease, thalassemia is diagnosed by looking for missing or reduced globin chains.
Key diagnostic tests include:
- Complete Blood Count (CBC)
- Hemoglobin Electrophoresis
- DNA analysis
These tests help figure out the type of thalassemia and its severity.
Combined Sickle Cell-Thalassemia Disorders
People with both sickle cell and thalassemia genes have sickle-thalassemia. This condition can cause a variety of health problems, from mild to severe.
We will discuss the effects of having both conditions. We will also look at how diagnosis and treatment might differ.
It’s important to understand the connection between sickle cell disease and thalassemia for effective care. Below is a table that highlights their differences and similarities:
| Condition | Cause | Diagnostic Tests |
| Sickle Cell Disease | Specific mutation in HBB gene | Hemoglobin Electrophoresis, DNA analysis |
| Thalassemia | Reduction or absence of globin chains | CBC, Hemoglobin Electrophoresis, DNA analysis |
| Sickle-Thalassemia | Combination of sickle cell and thalassemia genes | Combination of tests for both conditions |
Managing Pregnancy with Sickle Cell Disease
Managing pregnancy with sickle cell disease is complex. It involves a detailed plan to avoid complications. Sickle cell disease affects how the body makes hemoglobin, leading to abnormal red blood cells. Pregnancy can raise the risk of problems for both mom and baby.
Maternal Health Considerations
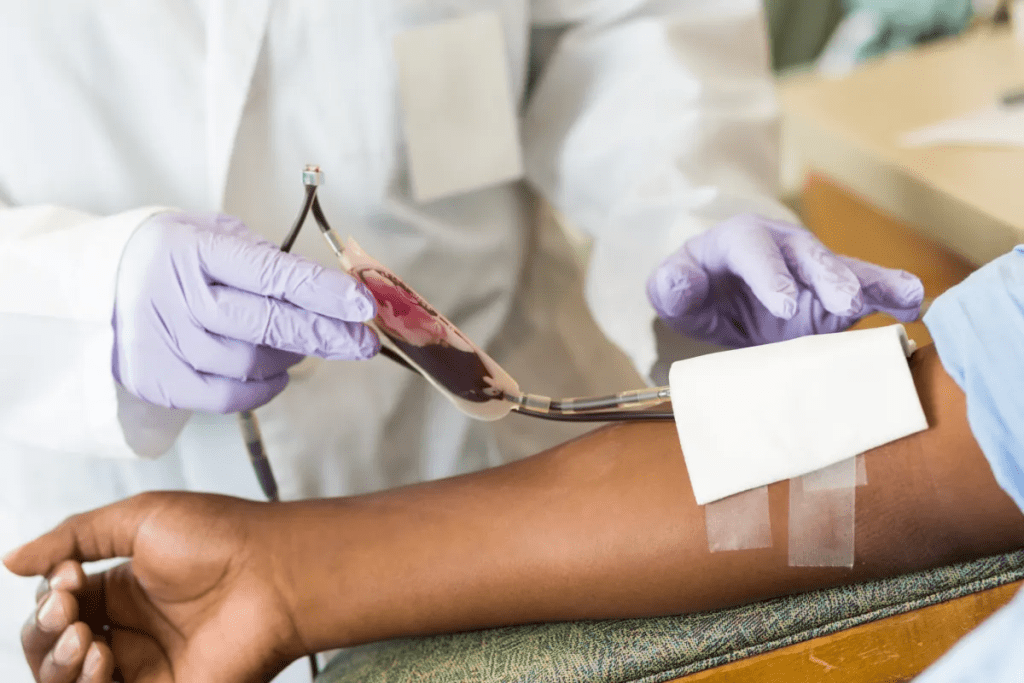
Pregnant women with sickle cell disease need close health monitoring. Regular check-ups with a healthcare provider are key. Important things to watch for include anemia, infections, and other sickle cell disease complications.
Anemia is common in these pregnancies because of sickle cell disease. We treat it with iron supplements, folic acid, and sometimes blood transfusions.
Specialized Care Requirements
Women with sickle cell disease need a team of specialists. This team includes obstetricians, hematologists, and others. This team approach helps manage pregnancy well, lowering the risk of problems.
| Specialized Care Aspect | Description |
| Regular Prenatal Visits | More frequent visits than typical pregnancies to monitor the health of both mother and fetus. |
| Hematology Consultations | Expert advice on managing sickle cell disease during pregnancy. |
| Pain Management | Strategies to manage pain crises associated with sickle cell disease. |
Potential Pregnancy Complications
Pregnant women with sickle cell disease face higher risks. These include preeclampsia, preterm labor, and fetal growth restriction. We watch for these closely to act quickly if needed.
Understanding these risks and working with healthcare providers can lead to a healthier pregnancy. We stress the value of preconception counseling and planning for the best outcomes.
Emotional and Psychological Aspects of Prenatal Sickle Cell Diagnosis
When a prenatal test shows sickle cell disease, families go through a lot. They feel shocked, deny it, and worry about the future. It’s a tough emotional ride.
Coping with Test Results
Dealing with this diagnosis needs a lot of support. Families get help from doctors, support groups, and family. “The diagnosis of sickle cell disease in a fetus can be a challenging experience, but with the right support, families can navigate this journey,” says a healthcare professional.
It’s key to remember that families are not alone. Talking to others who’ve been through it can offer comfort and advice.
Support Resources for Families
There are many resources for families with a prenatal sickle cell diagnosis:
- Genetic counseling to understand the diagnosis
- Support groups, both online and in-person, to connect with others
- Mental health professionals to address anxiety, depression, or other emotional challenges
- Educational materials to inform about sickle cell disease and its management
These resources are vital in helping families cope and make informed choices.
Decision-Making After Diagnosis
After a prenatal diagnosis of sickle cell disease, families must make big decisions. These choices are personal and depend on many factors. This includes the disease’s severity, family values, and personal beliefs.
Supportive care is key during this time. It ensures families have the info and emotional support they need to make the best decisions for them.
“The journey through a prenatal sickle cell diagnosis is not easy, but with complete support and care, families can find the strength to make informed decisions and navigate the challenges ahead.” – A healthcare provider
By creating a supportive and understanding space, we help families deal with the emotional and psychological sides of a prenatal sickle cell diagnosis.
Advances in Treatment and Research for Sickle Cell Disease
Treatment for sickle cell disease has made big strides thanks to research and new ideas. We’re learning more about this genetic disorder. This means new treatments are giving hope for better lives for those with it.
Current Treatment Options
Today, sickle cell disease treatment aims to manage symptoms and prevent serious problems. Hydroxyurea is a key drug that helps reduce pain crises and may cut down on blood transfusions. Blood transfusions are also key, as they increase normal red blood cells and lower risks of complications.
Pain management is also a big part of treatment. It uses both medicines and other methods to help patients feel better.
Emerging Therapies and Gene Editing
New treatments for sickle cell disease are on the horizon. Gene editing technologies like CRISPR/Cas9 might fix the genetic problem at its source. This could lead to a cure by making normal hemoglobin.
Other new treatments include gene therapy and new medicines. These aim to lessen the disease’s impact.
Future Outlook for Sickle Cell Management
The future for managing sickle cell disease looks bright. Ongoing research and new treatments are on the way. As we learn more, we’ll see treatments that are more precise and effective.
The use of gene editing and regenerative medicine could change treatment forever. This could bring us closer to a cure or better disease management.
It’s important for patients, doctors, and researchers to keep working together. With the speed of today’s research, we’re hopeful for big improvements in treating sickle cell disease.
Conclusion: Making Informed Decisions About Sickle Cell Testing During Pregnancy
Expectant parents need to make smart choices about sickle cell testing during pregnancy. This is key for the health of their baby. We’ve looked at sickle cell disease, its genetic roots, testing choices, and why prenatal screening matters.
Knowing your risks helps parents take action. With the right support and care, families can handle sickle cell disease well. We urge expectant parents to talk with their doctor about their situation and testing options.
Understanding testing and sickle cell disease helps parents get ready for their baby. We aim to provide top-notch healthcare and support for international patients. This way, families can make wise choices about sickle cell testing during pregnancy.
FAQ
What is sickle cell disease and how is it diagnosed?
Sickle cell disease is a genetic disorder that affects hemoglobin production. This causes red blood cells to be misshapen and break down. It is diagnosed through tests like hemoglobin electrophoresis, DNA analysis, and high-performance liquid chromatography (HPLC).
What is the difference between sickle cell trait and sickle cell disease?
Sickle cell trait means an individual has one copy of the mutated gene. Sickle cell disease happens when someone has two copies of the mutated gene, one from each parent. Sickle cell trait usually doesn’t cause health issues, but sickle cell disease can lead to serious problems.
Why is prenatal screening for sickle cell disease important?
Prenatal screening for sickle cell disease is key. It allows for early detection and management. This helps parents make informed decisions about their pregnancy and prepare for their child’s care.
What are the available testing options for sickle cell disease during pregnancy?
There are several testing options. These include chorionic villus sampling (CVS) and cell-free DNA testing in the first trimester. Amniocentesis is available in the second trimester. These tests can diagnose sickle cell disease and give expectant parents valuable information.
How accurate are prenatal sickle cell testing methods?
Prenatal sickle cell testing methods, like CVS and amniocentesis, are very accurate. But, there’s a small chance of false results. Sometimes, more testing is needed to confirm the diagnosis.
What are the risks associated with prenatal sickle cell testing?
Prenatal sickle cell testing has risks, such as miscarriage and costs. But, these risks are low. The benefits of testing usually outweigh the risks.
Can thalassemia be tested alongside sickle cell disease?
Yes, thalassemia can be tested with sickle cell disease. Tests like hemoglobin electrophoresis and DNA analysis are used. This is important because some people may have both conditions, affecting their health and management.
How is pregnancy managed in women with sickle cell disease?
Pregnancy for women with sickle cell disease needs special care. This includes regular monitoring, medication, and other interventions. These steps help ensure the best outcomes for both mother and baby.
What support is available for families dealing with a prenatal diagnosis of sickle cell disease?
Families with a prenatal diagnosis of sickle cell disease can find support. This includes counseling, support groups, and medical professionals. These resources help families cope with the diagnosis and make informed decisions about their care.
What are the current treatment options and emerging therapies for sickle cell disease?
Current treatments for sickle cell disease include medications and blood transfusions. Emerging therapies, like gene editing, offer hope for better management. They promise improved outcomes and quality of life.
Where can I find affordable sickle cell testing options?
Affordable sickle cell testing options are available. Look for healthcare providers, genetic testing laboratories, and non-profit organizations. It’s important to research and compare to find the best and most cost-effective testing.
How does sickle cell disease affect pregnancy?
Sickle cell disease can increase pregnancy risks, like preterm labor and preeclampsia. Women with sickle cell disease need close monitoring and specialized care. This helps manage risks and ensure a healthy pregnancy.
References
- World Health Organization. (2022, August 19). Sickle-cell disease and other haemoglobin disorders. Retrieved from https://www.who.int/news-room/fact-sheets/detail/sickle-cell-disease-and-other-haemoglobin-disorders