Last Updated on October 21, 2025 by mcelik

Myelodysplastic syndromes (MDS) are a group of disorders caused by poorly formed or dysfunctional blood cells. Understanding the symptoms of MDS progression is crucial for managing the condition effectively.
Recognizing the signs that MDS is getting worse can be challenging, but it’s essential for timely medical intervention. As MDS progresses, patients may experience a range of symptoms, including fatigue, infections, and bleeding complications.
Key Takeaways
- Understanding MDS progression is vital for effective management.
- Recognizing symptoms early can improve treatment outcomes.
- MDS progression can lead to severe health complications.
- Regular monitoring is crucial for patients with MDS.
- Timely medical intervention can significantly impact patient care.
Understanding Myelodysplastic Syndrome and Disease Progression
Myelodysplastic syndrome (MDS) is a complex condition characterized by the bone marrow’s inability to produce healthy blood cells. This disorder leads to ineffective hematopoiesis, resulting in low blood cell counts and various health complications.
What is MDS, and how does it affect the body?
MDS is a group of disorders that affect the bone marrow, causing it to produce defective blood cells. These cells, including red blood cells, white blood cells, and platelets, are crucial for oxygen delivery, infection fighting, and blood clotting, respectively. When these cells are dysfunctional, patients may experience anemia, infections, and bleeding disorders.
https://www.youtube.com/watch?v=t8R6BodCxjU
Different risk categories of MDS
MDS is categorized into different risk groups based on the likelihood of the disease progressing to acute myeloid leukemia (AML) and the patient’s overall survival outlook. The International Prognostic Scoring System (IPSS) is commonly used to classify MDS into various risk categories, ranging from very low to very high risk.
| Risk Category | Characteristics | Prognosis |
| Very Low Risk | Low blast percentage, few cytogenetic abnormalities | Better survival, lower risk of AML transformation |
| Low Risk | Moderate blast percentage, some cytogenetic abnormalities | Moderate survival, moderate risk of AML transformation |
| Intermediate Risk | Higher blast percentage, more cytogenetic abnormalities | Reduced survival, higher risk of AML transformation |
| High Risk | High blast percentage, complex cytogenetic abnormalities | Poor survival, high risk of AML transformation |
| Very High Risk | Very high blast percentage, multiple cytogenetic abnormalities | Poorest survival, very high risk of AML transformation |
Natural history and progression patterns
The natural history of MDS varies significantly among patients. Some may remain stable for years, while others may experience rapid progression to AML. Understanding the disease’s progression patterns is crucial for managing patient care effectively.
Factors influencing disease progression include the initial risk category, cytogenetic abnormalities, and the patient’s response to treatment. Regular monitoring and adjustments to the treatment plan are essential for managing MDS progression.
Key Signs MDS is Progressing: An Overview
MDS progression can be identified through a combination of clinical and laboratory indicators. Recognizing these signs is crucial for managing the disease effectively.
Clinical vs. Laboratory Indicators of Progression
Clinical indicators of MDS progression include symptoms such as increasing fatigue, frequent infections, and bleeding events. Laboratory indicators, on the other hand, involve changes in blood counts and bone marrow characteristics.
- Clinical Indicators: Fatigue, infections, bleeding events
- Laboratory Indicators: Changes in blood counts, bone marrow blast percentage
Transformation to Acute Myeloid Leukemia (AML)
One of the most significant concerns in MDS progression is the risk of transformation to Acute Myeloid Leukemia (AML). This transformation is characterized by a rapid increase in blast cells in the bone marrow.
- Increase in blast cells in bone marrow
- Rapid progression of disease
- Need for immediate medical intervention
Timeline Considerations for Disease Progression
The timeline for MDS progression varies significantly among patients. Factors influencing this timeline include the specific subtype of MDS, genetic mutations, and the patient’s overall health.
Understanding these factors helps in predicting the disease progression and planning appropriate treatment strategies.
Blood Count Changes That Indicate Worsening Disease

Changes in blood counts, such as declining hemoglobin and neutropenia, are significant indicators of worsening Myelodysplastic Syndrome (MDS). Monitoring these changes is crucial for understanding disease progression and potential complications.
Declining Hemoglobin Levels and Increasing Transfusion Needs
A decline in hemoglobin levels is a common sign of MDS progression. As hemoglobin levels fall, patients may experience increasing fatigue, weakness, and shortness of breath. This often necessitates more frequent blood transfusions to maintain adequate oxygen delivery to tissues and organs.
“The need for frequent transfusions can lead to iron overload, a condition that requires careful management to prevent organ damage,” as noted by experts in the field of MDS management.
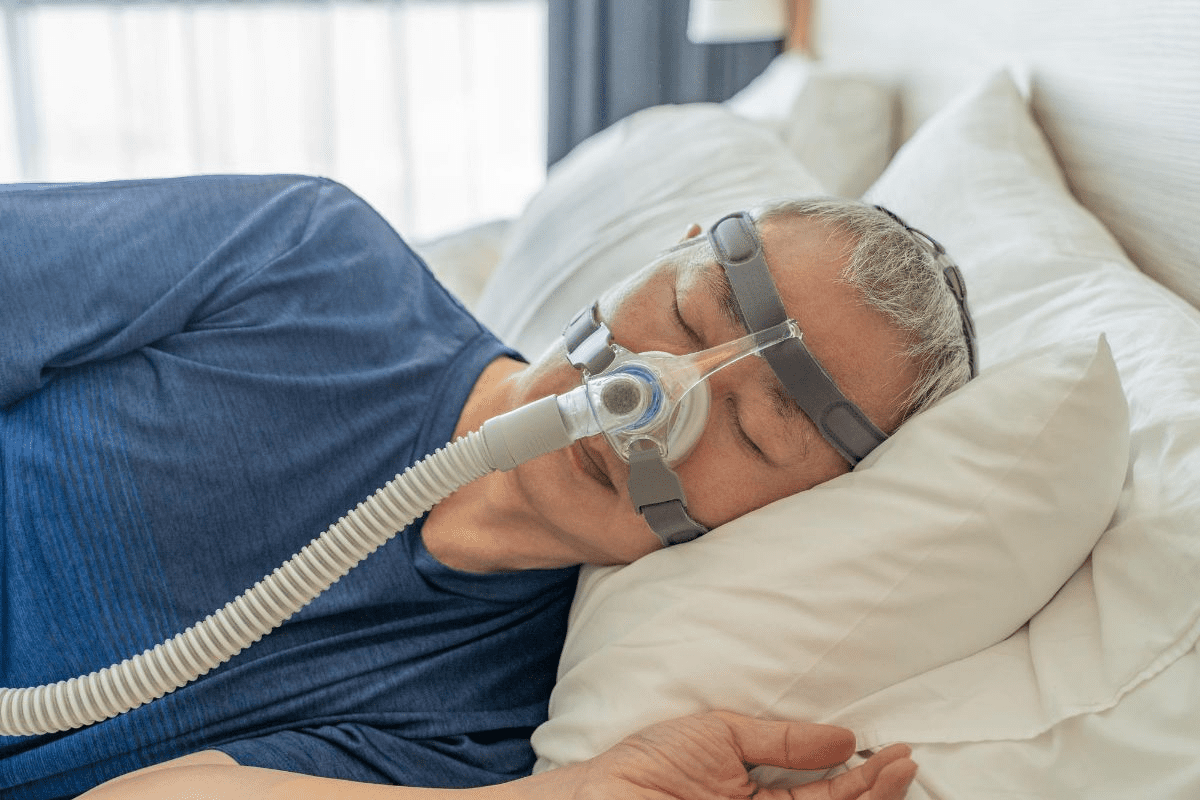
Neutropenia and Infection Risk Escalation
Neutropenia, or low neutrophil count, increases the risk of infections. As MDS progresses, the bone marrow’s ability to produce neutrophils can be further impaired, making patients more susceptible to infections that can be severe and life-threatening.
- Increased frequency of infections
- Prolonged duration of infections
- Severity of infections requiring hospitalization
Thrombocytopenia and Bleeding Complications
Thrombocytopenia, or low platelet count, can lead to bleeding complications. As platelet counts decline, patients are at a higher risk of bruising, nosebleeds, and potentially life-threatening hemorrhages.
Effective management of thrombocytopenia is critical to prevent these complications. This may involve platelet transfusions and other supportive care measures.
In conclusion, monitoring blood count changes is essential for managing MDS progression. By understanding the implications of declining hemoglobin, neutropenia, and thrombocytopenia, healthcare providers can tailor treatment plans to address these complications effectively.
Bone Marrow Changes as Signs MDS is Progressing
As MDS progresses, significant changes occur in the bone marrow that can indicate disease advancement. These changes are critical in understanding the progression of the disease and its impact on the patient’s health.
Increasing Blast Percentage in Bone Marrow
One of the key indicators of MDS progression is the increasing blast percentage in the bone marrow. Blasts are immature cells that are normally present in small numbers in the bone marrow. An increase in blast percentage can signal a transformation towards a more aggressive form of the disease, such as acute myeloid leukemia (AML).
The blast percentage is a crucial parameter monitored through regular bone marrow biopsies. An increase in blasts can indicate a worsening prognosis and may necessitate a change in treatment strategy.
Changes in Cellularity and Dysplasia
Changes in cellularity and dysplasia are also significant indicators of MDS progression. Cellularity refers to the proportion of the bone marrow cavity that is occupied by hematopoietic cells. Dysplasia refers to the abnormal development of cells, which can lead to ineffective hematopoiesis.
As MDS progresses, the bone marrow may become either hypercellular (increased cellularity) or hypocellular (decreased cellularity), and the degree of dysplasia may increase. These changes can lead to a decline in the production of healthy blood cells, contributing to the symptoms and complications associated with MDS.
Cytogenetic and Molecular Evolution
Cytogenetic and molecular evolution are critical aspects of MDS progression. Cytogenetic changes refer to alterations in the chromosomes of bone marrow cells, while molecular evolution involves changes at the genetic level that can affect the behavior of MDS cells.
These changes can lead to the development of new clones of abnormal cells that may be more resistant to treatment. Monitoring cytogenetic and molecular changes through techniques such as karyotyping, FISH, and molecular testing can provide valuable information on the disease’s progression and help guide treatment decisions.
Physical Symptoms That May Worsen During Progression
MDS progression is often characterized by an escalation of physical symptoms, including fatigue, infections, and bleeding events. As the disease advances, patients may experience a decline in their overall physical condition, marked by several worsening symptoms.
Escalating Fatigue and Exercise Intolerance
One of the most common symptoms of MDS progression is escalating fatigue, which can significantly impact a patient’s ability to perform daily activities. This fatigue is often accompanied by exercise intolerance, making it challenging for individuals to engage in physical activities they once enjoyed.
A study published in a leading hematology journal found that patients with MDS experienced a significant decrease in their quality of life due to fatigue, highlighting the need for effective management strategies.
“Fatigue is a pervasive symptom in MDS patients, affecting their daily lives and overall well-being.”
A leading hematologist
Increased Frequency and Severity of Infections
As MDS progresses, patients may experience an increased frequency and severity of infections. This is often due to neutropenia, a condition characterized by low levels of neutrophils, a type of white blood cell crucial for fighting infections.
- Increased susceptibility to bacterial, viral, and fungal infections
- More severe infections require hospitalization
- Prolonged recovery times from infections
Unusual Bleeding Events and Bruising
Patients with progressing MDS may also experience unusual bleeding events and bruising, often due to thrombocytopenia, a condition marked by low platelet counts. This can manifest as easy bruising, nosebleeds, or bleeding gums.
| Symptom | Description |
| Easy Bruising | Bruising without significant trauma |
| Nosebleeds | Frequent or severe nosebleeds |
| Bleeding Gums | Bleeding when brushing teeth or eating |
It is essential for patients to report these symptoms to their healthcare provider to adjust their treatment plan accordingly.
Systemic Manifestations of Progressive MDS
As MDS progresses, patients may experience a range of systemic manifestations that can significantly impact their quality of life. These manifestations can be diverse, affecting various bodily systems and overall health.
Weight Loss and Nutritional Challenges
One of the common systemic effects of progressive MDS is weight loss, often accompanied by nutritional challenges. This can be due to a decrease in appetite, changes in metabolism, or difficulties in consuming and digesting food properly. Ensuring adequate nutrition is crucial, as it can help manage some symptoms and support overall health.
Patients experiencing weight loss and nutritional challenges may benefit from consulting a dietitian or nutritionist to develop a personalized meal plan. This plan can help ensure they receive the necessary calories and nutrients.
Enlargement of the Spleen or Liver
Progressive MDS can also lead to the enlargement of the spleen or liver, a condition that can cause discomfort and other complications. An enlarged spleen (splenomegaly) or liver (hepatomegaly) can be detected during physical examinations or through imaging tests.
The enlargement of these organs is often a sign of the disease’s progression and may require specific management strategies. Monitoring and addressing these changes are crucial for maintaining patient comfort and managing potential complications.
Skin Changes and Pallor
Skin changes are another systemic manifestation of progressive MDS. Patients may notice pallor (pale skin), bruising, or other dermatological changes. These changes can be due to various factors, including anemia, low platelet counts, or other effects of the disease on the body.
Managing skin changes and pallor involves addressing the underlying causes, such as treating anemia or managing bleeding risks. Proper skin care and protection can also help mitigate some of these changes.
When to Seek Immediate Medical Attention
Understanding when to seek immediate medical help is vital for managing MDS effectively. Patients with MDS need to be aware of the signs that indicate a significant progression of their disease, requiring prompt medical evaluation.
Emergency Warning Signs Requiring Urgent Care
Certain symptoms can signal a critical worsening of MDS. These include:
- Severe fatigue that interferes with daily activities
- Frequent or severe infections that do not respond to treatment
- Unusual bleeding or bruising
- Shortness of breath or difficulty breathing
Experiencing any of these symptoms warrants immediate contact with a healthcare provider.
Communicating Effectively with Emergency Providers
When seeking urgent care, it’s crucial to communicate effectively with emergency providers. Patients should:
- Bring a list of their current medications and dosages
- Provide information about their MDS diagnosis, including the specific type and any previous treatments
- Share any relevant medical history, including allergies and other health conditions
Clear communication can help ensure that patients receive the most appropriate care in an emergency situation.
Diagnostic Procedures to Monitor and Assess Progression
Diagnostic procedures play a vital role in monitoring MDS progression and guiding treatment decisions. Regular assessments are crucial for understanding the disease’s progression and making necessary adjustments to the treatment plan.
Frequency of Follow-up Bone Marrow Biopsies
Bone marrow biopsies are a critical diagnostic tool for assessing MDS progression. The frequency of these biopsies depends on the individual’s risk category and the stability of their condition. Generally, bone marrow biopsies are performed at the time of diagnosis and repeated as necessary based on clinical judgment.
For patients with lower-risk MDS, bone marrow biopsies may be repeated every 6 to 12 months if the disease is stable. However, if there’s a suspicion of disease progression or transformation to acute myeloid leukemia (AML), biopsies may be performed more frequently.
In cases of higher-risk MDS, more frequent monitoring may be required, potentially every 3 to 6 months, to closely track disease progression and response to treatment.
Blood Test Monitoring Schedules
Blood tests are another essential diagnostic tool for monitoring MDS progression. Regular blood counts help track changes in hemoglobin levels, neutrophil counts, and platelet counts, providing insights into the disease’s status.
- Complete Blood Counts (CBCs) are typically performed at every clinic visit, which may be as frequent as every 1 to 3 months.
- Blood chemistry tests may also be conducted to assess liver and kidney function, which can be affected by the disease or its treatment.
Advanced Molecular and Genetic Testing
Advanced molecular and genetic testing play an increasingly important role in diagnosing and monitoring MDS. These tests can identify specific genetic mutations that may influence disease progression and treatment response.
Molecular testing can help detect mutations in genes such as TP53, RUNX1, and ASXL1, which are associated with a higher risk of progression. Genetic testing may also be used to monitor the effectiveness of certain treatments and detect emerging resistance.
By combining the results from bone marrow biopsies, blood tests, and molecular and genetic testing, healthcare providers can gain a comprehensive understanding of MDS progression and make informed decisions about treatment.
Treatment Plan Adjustments When MDS Progresses
When myelodysplastic syndrome (MDS) advances, healthcare providers often need to reassess and adjust treatment strategies to manage the disease effectively. As the condition progresses, the initial treatment plan may no longer be sufficient, necessitating changes to ensure the best possible outcomes for patients.
Intensification of Current Therapies
One approach to adjusting treatment plans involves intensifying current therapies. This can include increasing the dosage of medications, adding new drugs to the existing regimen, or switching to more aggressive treatments. The goal is to control the progression of MDS and alleviate symptoms.
Intensification of therapies can be particularly beneficial for patients who have shown an initial response to treatment but are now experiencing disease progression. For instance, patients on hypomethylating agents may require dose adjustments or the addition of other therapies to maintain disease control.
Evaluation for Stem Cell Transplantation
For some patients, stem cell transplantation may become a viable option as MDS progresses. This procedure involves replacing the patient’s diseased bone marrow with healthy stem cells from a donor. It is a potentially curative treatment but comes with significant risks and is typically considered for patients with higher-risk MDS or those who have not responded to other treatments.
The evaluation process for stem cell transplantation includes a thorough assessment of the patient’s overall health, the specific characteristics of their MDS, and the availability of a suitable donor. Candidacy for transplantation is determined on a case-by-case basis, taking into account various factors such as age, comorbidities, and the presence of any other health issues.
Clinical Trials for Progressive Disease
Participation in clinical trials is another important consideration for patients with progressive MDS. These trials offer access to new and innovative treatments that are not yet widely available. They can provide valuable insights into the safety and efficacy of emerging therapies and may offer additional treatment options for patients who have exhausted standard therapies.
Clinical trials may investigate various approaches, including novel medications, combination therapies, or different treatment schedules. Patients interested in participating in a clinical trial should discuss their eligibility with their healthcare provider, considering factors such as the trial’s inclusion and exclusion criteria, potential benefits, and associated risks.
Managing Quality of Life During Disease Progression
Effective management of MDS progression involves not just medical treatment, but also strategies to enhance quality of life. As the disease advances, patients face numerous challenges that impact their daily living, making comprehensive care essential.
Symptom Management Strategies
Symptom management is a critical component of maintaining quality of life for MDS patients. This includes addressing fatigue, managing pain, and mitigating other symptoms that can significantly impact daily activities. According to the MDS Foundation, “symptom management is not just about alleviating suffering; it’s about improving the patient’s ability to function and enjoy life.”
“The goal of symptom management is to enable patients to maintain their independence and quality of life as much as possible.” – MDS Foundation.
Healthcare providers may employ various strategies, including medication adjustments, transfusions, and other supportive therapies tailored to the patient’s needs.
Safe Physical Activity Recommendations
Physical activity is vital for MDS patients, even during disease progression. Gentle exercises such as walking, yoga, or light stretching can help maintain strength, flexibility, and overall well-being. It’s essential to consult with healthcare providers to develop a safe exercise plan that considers the patient’s current health status and capabilities.
Regular physical activity can also help manage fatigue and improve mental health. Patients should be encouraged to stay active within their limits.
Nutritional Support During Progression
Nutritional support plays a vital role in managing MDS progression. A well-balanced diet rich in essential nutrients can help maintain strength and support overall health. Patients may benefit from consulting a dietitian to develop a personalized nutrition plan.
Nutritional challenges are common in advanced MDS, including weight loss and decreased appetite. Healthcare providers can offer guidance on managing these issues, potentially including nutritional supplements.
Managing quality of life during MDS progression requires a multifaceted approach that includes symptom management, safe physical activity, and nutritional support. By focusing on these areas, patients can maintain a better quality of life despite the challenges posed by the disease.
Emotional and Psychological Impact of Progressive MDS
Living with progressive MDS can have a profound impact on a patient’s mental health and overall well-being. The disease’s progression affects not only the patient but also their family and caregivers, creating a ripple effect of emotional and psychological challenges.
Coping with Uncertainty and Changing Prognosis
Coping with the uncertainty of MDS progression is a significant challenge. Patients and caregivers must adapt to changing circumstances, including the possibility of intensified treatment plans or the need for new interventions. Uncertainty can lead to anxiety and fear, making it essential to develop effective coping strategies.
One approach to managing uncertainty is to stay informed about the disease and its progression. Understanding what to expect can help reduce anxiety and allow patients to make informed decisions about their care. Support from healthcare providers, family, and friends is crucial during this time.
Support Resources for Patients and Caregivers
Access to support resources is vital for patients and caregivers dealing with the emotional and psychological impact of progressive MDS. Support groups, either in-person or online, can provide a sense of community and understanding. These groups allow individuals to share their experiences and learn from others facing similar challenges.
In addition to support groups, professional counseling can be beneficial. Mental health professionals can offer strategies to cope with the emotional aspects of the disease, including managing stress, anxiety, and depression. It’s essential to prioritize mental health alongside physical health.
For those seeking additional support, numerous organizations offer resources specifically for patients with MDS and their caregivers. These resources may include educational materials, helplines, and online forums. Utilizing these resources can provide comfort and guidance during a challenging time.
Effective Communication with Your Healthcare Team
Understanding how to communicate effectively with your healthcare team is vital for navigating MDS progression. Effective communication ensures that you receive the best possible care tailored to your specific needs.
Questions to Ask About Disease Progression
Asking the right questions can help you understand your condition better and make informed decisions about your care. Consider asking your healthcare provider about the signs of MDS progression, such as changes in blood counts or the development of new symptoms.
Some key questions to ask include:
- What are the expected changes in my condition as MDS progresses?
- How often should I have follow-up appointments and blood tests?
- What are the potential complications of MDS progression, and how can they be managed?
Building a Comprehensive Care Team
A comprehensive care team can provide you with the support and expertise needed to manage MDS effectively. This team may include hematologists, primary care physicians, nurses, and other specialists.
The benefits of a comprehensive care team include:
- Coordinated care that addresses all aspects of your health
- Access to a range of expertise, from hematology to supportive care
- Improved communication and reduced risk of misunderstandings or misdiagnoses
By working closely with your healthcare team and asking the right questions, you can take an active role in managing your MDS and improving your quality of life.
Research Advances in Understanding and Treating Progressive MDS
As research into MDS continues to advance, new insights into disease progression and treatment options are emerging. Ongoing studies are crucial for understanding the complexities of MDS and developing effective treatments.
Emerging Biomarkers of Disease Progression
Researchers are identifying new biomarkers that can predict MDS progression more accurately. These biomarkers are vital for early intervention and personalized treatment plans.
Key emerging biomarkers include:
- Genetic mutations such as TP53 and RUNX1
- Cytogenetic abnormalities
- Molecular markers indicating disease severity
A recent study highlighted the importance of molecular profiling in predicting disease progression, stating, “Molecular profiling has the potential to revolutionize the way we diagnose and treat MDS.”
Novel Therapeutic Approaches for Advanced MDS
Treatment strategies for MDS are evolving, with several novel therapies showing promise. These include targeted therapies, immunotherapies, and combination regimens designed to improve outcomes for patients with advanced MDS.
| Therapeutic Approach | Description | Potential Benefits |
| Targeted Therapies | Drugs that target specific genetic mutations | Improved efficacy, reduced side effects |
| Immunotherapies | Treatments that harness the immune system to fight cancer | Enhanced immune response against MDS cells |
| Combination Regimens | Combining different therapies to achieve better outcomes | Potential for overcoming resistance, improving survival rates |
The future of MDS treatment looks promising, with ongoing research and clinical trials paving the way for innovative therapies. As our understanding of the disease deepens, we can expect to see more effective and personalized treatment options.
Conclusion
Recognizing the signs of Myelodysplastic Syndrome (MDS) progression is crucial for effective disease management. This article has outlined the key indicators of MDS progression, including changes in blood counts, bone marrow abnormalities, and physical symptoms.
Understanding these signs enables patients to seek timely medical attention and adjust their treatment plans accordingly. By staying informed and working closely with their healthcare team, patients can better manage their condition and improve their quality of life.
A summary of key points discussed in this article highlights the importance of monitoring blood count changes, bone marrow abnormalities, and physical symptoms. By being aware of these indicators, patients can take proactive steps to manage their MDS and address any concerns promptly.
FAQ
What are the common signs that MDS is progressing?
Common signs of MDS progression include worsening anemia, increasing fatigue, frequent infections, unusual bleeding or bruising, and weight loss.
How do blood count changes indicate worsening MDS?
Declining hemoglobin levels, neutropenia, and thrombocytopenia are key indicators of worsening MDS, often resulting in increased transfusion needs, infection risk, and bleeding complications.
What bone marrow changes signify MDS progression?
Increasing blast percentage, changes in cellularity and dysplasia, and cytogenetic and molecular evolution are significant bone marrow changes that indicate MDS progression.
When should I seek immediate medical attention for MDS progression?
Seek immediate medical attention if you experience severe symptoms such as heavy bleeding, severe infections, or significant worsening of fatigue, as these may be emergency warning signs requiring urgent care.
How is MDS progression monitored and assessed?
MDS progression is monitored through regular bone marrow biopsies, blood tests, and advanced molecular and genetic testing to assess changes in disease status and guide treatment decisions.
What adjustments may be made to treatment plans as MDS progresses?
Treatment plans may be adjusted by intensifying current therapies, evaluating for stem cell transplantation, or considering participation in clinical trials for progressive disease.
How can quality of life be maintained during MDS progression?
Maintaining quality of life during MDS progression involves symptom management strategies, safe physical activity recommendations, and nutritional support to address the systemic effects of the disease.
What are the emotional and psychological impacts of MDS progression?
MDS progression can lead to increased uncertainty and changing prognosis, emphasizing the need for coping mechanisms and support resources for patients and caregivers.
How can I effectively communicate with my healthcare team about MDS progression?
Effective communication involves asking questions about disease progression, building a comprehensive care team, and staying informed about the latest research advances and treatment options.
What are the latest research advances in understanding and treating progressive MDS?
Recent research advances include the identification of emerging biomarkers of disease progression and the development of novel therapeutic approaches for advanced MDS.
How does MDS progression affect nutritional status?
MDS progression can lead to weight loss and nutritional challenges, making nutritional support an essential aspect of managing the disease.
Can MDS progression lead to enlargement of organs like the spleen or liver?
Yes, MDS progression can result in the enlargement of organs such as the spleen or liver, which is a systemic manifestation of the disease.
What are the signs of MDS transforming to acute myeloid leukemia (AML)?
Signs of MDS transforming to AML include a rapid increase in blast cells, worsening blood counts, and potentially, an increase in symptoms such as fatigue, infections, and bleeding.
References
- Jain, A. G., et al. (2024). Patterns of lower risk myelodysplastic syndrome progression. Haematologica, 109(1), e1-e13. https://pmc.ncbi.nlm.nih.gov/articles/PMC11215361/