Stem cells can develop into many cell types and act as the body’s repair system. They replace or restore damaged tissues, offering new possibilities for treating diseases.
Send us all your questions or requests, and our expert team will assist you.

Recovery following Allogeneic Stem Cell Transplantation for myelofibrosis is a gradual, transformative process that extends well beyond the hospital stay. Unlike other hematologic malignancies, myelofibrosis patients face unique challenges due to the pre-existing state of their bodies: massive spleens, a history of inflammatory wasting, and the physical presence of marrow scars.

GVHD remains the primary long-term complication to manage. This occurs when the donor’s immune system attacks the recipient’s tissues.
The GVL Balance: In myelofibrosis, a mild degree of GVHD is sometimes associated with a lower risk of relapse. This is because the same donor immune cells causing GVHD are also attacking any remaining cancer cells (the Graft-Versus-Leukemia effect). Clinicians carefully balance immunosuppressive medications to maintain this beneficial effect while preventing severe toxicity.

Survivorship care involves frequent monitoring of blood counts and chimerism studies.

Recovery involves physical and psychological rehabilitation.

For patients managed with drug therapies (JAK inhibitors), follow-up focuses on disease stability.
Send us all your questions or requests, and our expert team will assist you.
The reversal of fibrosis is a slow process. While healthy blood production can start within weeks, the actual structural remodeling of the bone marrow takes time. Significant reduction in scarring is typically seen in biopsies performed 6 to 12 months after the transplant, and improvement can continue for years.
Chimerism testing is a DNA test done on your blood after a transplant. It checks whose cells are circulating—yours or the donor’s. The goal is to see 100% donor DNA. If the percentage of donor cells drops, it might indicate that the old marrow is trying to grow back, signaling a risk of relapse.
The high-dose chemotherapy used for the transplant wipes out your immune system’s memory. Even though you had vaccines as a child, your new immune system (from the donor) is “naive” to those specific diseases. You must receive your childhood vaccines again to be protected against things like measles, mumps, and polio.
After a successful stem cell transplant, the spleen typically shrinks and remains small because the bone marrow is functioning correctly. However, if the transplant fails or the disease relapses, the spleen can enlarge again as the body tries to restart extramedullary hematopoiesis.
Relapse risk varies based on the genetic risk profile and the stage of the disease at the time of transplant. Generally, the risk is around 15-20%. Relapse is most common in the first two years. Doctors monitor chimerism and blood counts closely to catch any signs of relapse early, when it is most treatable.

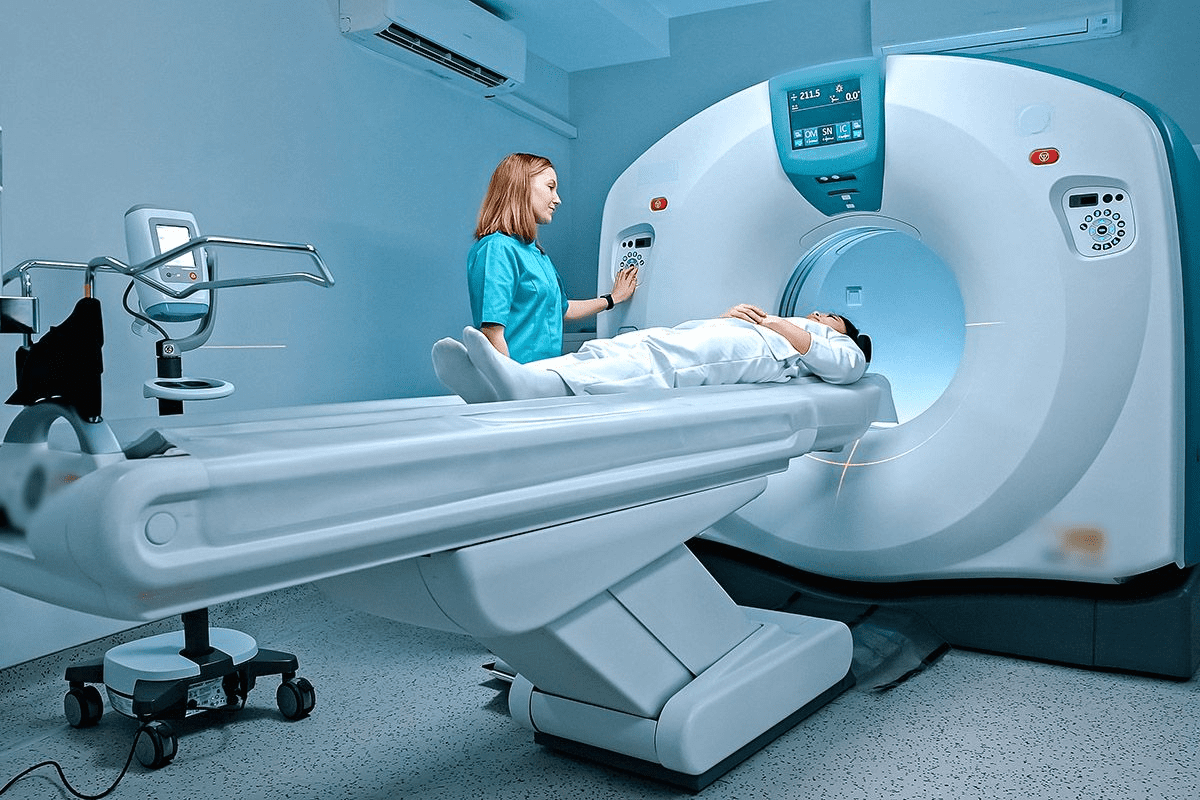
Getting ready for a kidney CT scan is key to getting clear images. These images help find different kidney problems. At Liv Hospital, we make sure


Millions of aging men deal with Benign Prostatic Hyperplasia (BPH). They face issues like needing to pee a lot, weak urine, and waking up at


Urinary incontinence affects millions globally, causing significant distress and impacting quality of life. It’s embarrassing and frustrating to leak urine involuntarily. Stress urinary incontinence often

Getting a cancer diagnosis for your child is incredibly tough. The road ahead is filled with tough moments, from the first shock to the long

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)