Millions of people worldwide face issues with their blood cells. This includes red blood cells, white blood cells, and platelets. Blood disorders can greatly change a person’s life, making it key to know about them.We unveil the three most common blood disorders in a shocking new list. Get critical details and essential information on these powerful conditions.
Anemia, leukemia, and lymphoma are big concerns. Anemia lowers the number of healthy red blood cells, causing tiredness and other issues. Leukemia and lymphoma are cancers that hit the blood and lymphatic system, respectively.
It’s vital for both patients and doctors to grasp these common hematology disorders. We’ll dive into their symptoms, how to diagnose them, and treatment choices. This knowledge is key to handling these serious health issues.
Key Takeaways
- Anemia, leukemia, and lymphoma are the three most prevalent blood disorders.
- These conditions affect millions of people worldwide, impacting their quality of life.
- Understanding the symptoms, diagnosis, and treatment options is key for managing these conditions.
- Early detection and proper medical care can greatly improve patient outcomes.
- Patients and healthcare providers must work together to manage these common hematology disorders effectively.
The Vital Role of Blood in Human Health
Blood is a vital fluid that moves through our bodies. It carries the necessary components for our tissues and organs to work well. It helps keep our body balanced by moving oxygen, nutrients, and hormones to cells and organs. It also removes waste products.
Blood Composition and Functions
Blood is made up of several important parts. It has plasma, red blood cells, white blood cells, and platelets. Plasma makes up about 55% of blood and is mostly water. It also has proteins, nutrients, hormones, gases, waste products, and ions.
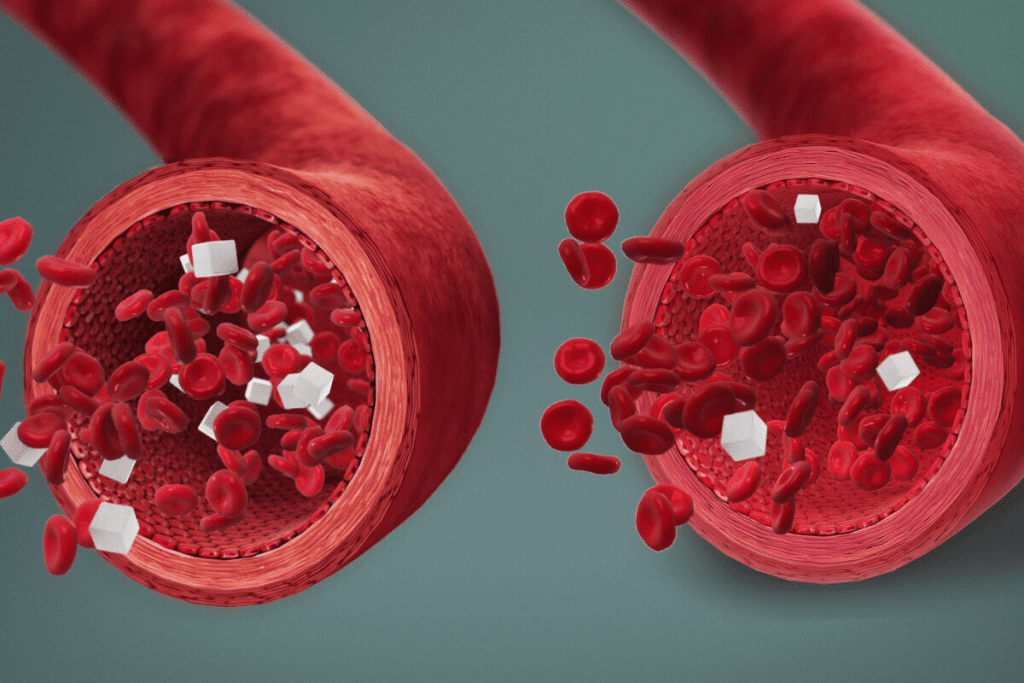
Red blood cells, or erythrocytes, carry oxygen to our tissues. They have hemoglobin, a protein that binds oxygen. This lets oxygen travel from the lungs to our body’s tissues. White blood cells, or leukocytes, help fight infections. Platelets, or thrombocytes, are key for blood clotting. They help stop bleeding when a blood vessel is injured.
| Blood Component | Function |
| Plasma | Transports proteins, nutrients, hormones, gases, waste products |
| Red Blood Cells (Erythrocytes) | Delivers oxygen to tissues |
| White Blood Cells (Leukocytes) | Defends against infections |
| Platelets (Thrombocytes) | Essential for blood clotting |
The Hematopoietic System
The hematopoietic system makes blood cells. It includes the bone marrow, where stem cells turn into different blood cells. This system is key for keeping blood cells balanced and healthy throughout our lives.
“The hematopoietic system is a complex network that ensures the continuous production of blood cells, adapting to the body’s needs and responding to stress or damage.”
How Blood Maintains Homeostasis
Blood is vital for keeping our body’s internal environment balanced. It carries hormones that control our body’s functions, like metabolism and growth. It also helps keep pH levels balanced and maintains the right balance of nutrients and waste.
Understanding blood’s role in health is key to grasping blood disorders. By knowing how blood composition, the hematopoietic system, and blood functions help our health, we can better understand blood-related diseases.
What Constitutes a Blood Disorder?
Blood disorders are many and varied. They affect how blood carries oxygen, fights off infections, or clots. This can lead to serious health problems.
Classification of Blood Disorders
Blood disorders fall into several groups. These include anemia, leukemia, lymphoma, and bleeding disorders. Each group shows a different kind of blood problem.
- Anemia: A lack of red blood cells or hemoglobin. This means tissues don’t get enough oxygen.
- Leukemia: A blood or bone marrow cancer that messes with white blood cell production.
- Lymphoma: A cancer that starts in the lymph system, part of the immune system.
- Bleeding Disorders: Issues like hemophilia that make it hard for blood to clot, causing long bleeding.
Knowing how to classify blood disorders helps doctors diagnose and treat them better.
| Category | Description | Common Symptoms |
| Anemia | Deficiency in red blood cells or hemoglobin | Fatigue, weakness, pale skin |
| Leukemia | Cancer of the blood or bone marrow | Fever, weight loss, frequent infections |
| Lymphoma | Cancer of the lymph system | Swollen lymph nodes, fever, weight loss |
| Bleeding Disorders | Conditions affecting blood clotting | Prolonged bleeding, bruising easily |
Common Symptoms of Blood Disorders
Different blood disorders show different symptoms. Anemia might cause fatigue, weakness, and shortness of breath. Leukemia and lymphoma can lead to fever, weight loss, and infections. Bleeding disorders might cause long bleeding or easy bruising.
It’s important to recognize these symptoms. This helps you get the right medical care and treatment.
The Three Most Common Blood Disorders
It’s important to know about the three main blood disorders. These include anemia, leukemia, and lymphoma. They are big health issues that affect many people around the world.
Global Prevalence Statistics
Anemia, leukemia, and lymphoma are big problems globally. Anemia hits about 1.62 billion people, or 24.8% of the world’s population. Leukemia affects around 437,000 new people each year. Lymphoma is also a big cancer issue worldwide.
These disorders are more common in some places than others. For example, anemia is more common where food is scarce and healthcare is hard to get. Leukemia and lymphoma can be more common in areas with certain environmental or genetic risks.
Impact on Public Health

Anemia, leukemia, and lymphoma have a big impact on health. Anemia can cause tiredness, weakness, and brain fog. This can hurt work and life quality. Leukemia and lymphoma, being blood cancers, need strong treatments and can deeply affect patients’ lives.
These disorders also cost a lot to treat. The costs include medical bills, lost work time, and the toll on caregivers. It’s key to have public health efforts to prevent, catch early, and manage these diseases well.
Common Risk Factors
There are many things that can lead to anemia, leukemia, and lymphoma. For anemia, not getting enough iron is a big risk. For leukemia and lymphoma, genetic risks, certain chemicals, and infections like Epstein-Barr virus play a part.
Knowing these risks helps us find ways to prevent them. For example, eating better can help avoid anemia. Staying away from harmful chemicals and radiation can lower the risk of leukemia and lymphoma.
Anemia: The Most Widespread Blood Disorder
Anemia is a common condition found in millions around the world. It happens when there are fewer red blood cells or less hemoglobin. This can make it hard for the body to get enough oxygen, leading to tiredness, weakness, and other health problems.
Definition and Pathophysiology
Anemia is when there are not enough red blood cells or hemoglobin. Hemoglobin is a protein in red blood cells that carries oxygen. The causes of anemia include problems with making red blood cells, losing them too fast, or losing blood.
Understanding how anemia works is key to treating it. We will look at why it happens, including not getting enough nutrients, having chronic diseases, or genetic disorders.
Major Types of Anemia
There are many types of anemia, each with its own cause and symptoms. The main types are:
- Iron deficiency anemia: Happens when you don’t get enough iron.
- Vitamin deficiency anemia: Caused by not getting enough vitamins like B12 or folate.
- Anemia of chronic disease: Linked to long-term illnesses like cancer or HIV/AIDS.
- Sickle cell anemia: A genetic disorder that affects hemoglobin production.
| Type of Anemia | Causes | Characteristics |
| Iron Deficiency Anemia | Inadequate iron intake or absorption | Low hemoglobin levels, fatigue |
| Vitamin Deficiency Anemia | Lack of vitamins B12 or folate | Neurological symptoms, weakness |
| Anemia of Chronic Disease | Chronic illnesses like cancer or HIV/AIDS | Normocytic anemia, chronic inflammation |
Who Is Most at Risk for Anemia?
Some groups are more likely to get anemia. These include:
- Women of childbearing age, specially during pregnancy
- Children and teens because they grow fast
- People with long-term diseases or infections
- Vegetarians or vegans who might not get enough iron or vitamin B12
Knowing who is at risk helps catch anemia early. We will talk about why it’s important to be aware and how to prevent it.
Iron Deficiency Anemia in Detail
Iron deficiency anemia is a common problem worldwide. It happens when the body doesn’t have enough iron. This is needed to make hemoglobin, a key protein in red blood cells that carries oxygen.
Causes of Iron Deficiency
There are many reasons why people get iron deficiency anemia. Not getting enough iron from food is a big one. People who don’t eat meat or animal products often struggle to get enough iron.
Another reason is losing blood too much. This can happen from gastrointestinal bleeding, heavy periods, or giving blood too often. Women who are pregnant or breastfeeding also need more iron, which can be hard to get from food alone.
Clinical Manifestations
Iron deficiency anemia can cause many symptoms. People often feel fatigued, weak, and have shortness of breath. They might also have pale skin, cold hands and feet, and dizziness.
In severe cases, it can lead to heart problems and affect how well the brain works.
Diagnostic Approach
To diagnose iron deficiency anemia, doctors use several methods. They start with a complete blood count (CBC) to check hemoglobin levels. Then, they might do tests like serum ferritin and transferrin saturation to confirm the diagnosis and see how bad it is.
Treatment Strategies
Treatment usually involves taking iron supplements. The type of supplement depends on how severe the deficiency is and how well the patient can take oral iron. Eating foods rich in iron is also important. Sometimes, treating the cause of the iron deficiency is key to managing it well.
Sickle Cell Disease: A Genetic Blood Disorder
Sickle cell disease is a serious genetic disorder. It affects many people and has significant health impacts. The disease causes abnormal hemoglobin production, leading to distorted red blood cells.
Genetic Basis and Inheritance
The disease is caused by a mutation in the HBB gene. This mutation leads to hemoglobin S (HbS) production. Under low oxygen, HbS causes red blood cells to become sickle-shaped.
The disease is inherited in an autosomal recessive pattern. This means a person needs two defective HBB genes to have the disease.
Inheritance Patterns: Carriers have one normal and one mutated HBB gene. They usually don’t show symptoms but can pass the mutated gene to their children.
Pathophysiology of Sickle Cell Crisis
A sickle cell crisis happens when sickled red blood cells block small blood vessels. This causes tissue ischemia and pain. Various factors can trigger a crisis, like dehydration or infection.
The pathophysiology involves complex interactions between sickled red blood cells, endothelial cells, and inflammatory mediators. Understanding these interactions is key to managing the disease.
Clinical Manifestations
Sickle cell disease shows many symptoms, including pain, anemia, infections, and splenic sequestration. The severity and frequency of these symptoms vary among individuals.
- Chronic anemia due to reduced red blood cell lifespan
- Recurrent infections due to splenic dysfunction
- Acute pain episodes resulting from vaso-occlusive crises
Epidemiology and Demographics
Sickle cell disease is common in sub-Saharan Africa and among people of African descent. It is also found in the Middle East and India.
Epidemiological Data: The World Health Organization says sickle cell disease affects millions globally. It has a big impact on public health in affected areas.
“Sickle cell disease is a major public health issue in many parts of the world, requiring extensive management strategies to improve the quality of life for those affected.” – World Health Organization
Managing Sickle Cell Disease
Managing sickle cell disease requires a mix of treatments, pain control, and new therapies. It’s key to better patient care and quality of life.
Standard Treatment Protocols
Standard treatments aim to lessen crisis frequency and severity. They also manage symptoms and prevent complications. These include:
- Hydroxyurea therapy to reduce crisis frequency
- Blood transfusions to boost oxygen delivery
- Medications for pain and infection prevention
A hematologist says, “Hydroxyurea has changed sickle cell disease management. It cuts down on painful crises and improves outcomes.”
“Hydroxyurea has transformed sickle cell disease treatment. It makes the condition more manageable for patients.”
Pain Management Strategies
Pain control is vital in sickle cell disease care. Strategies include:
- Pharmacological methods, like NSAIDs and opioids
- Non-pharmacological methods, such as cognitive-behavioral therapy and relaxation
| Pain Management Approach | Description |
| Pharmacological | Medications like NSAIDs and opioids for pain |
| Non-pharmacological | Cognitive-behavioral therapy, relaxation, and more |
Preventive Care Approaches
Preventive care is critical for sickle cell disease patients. It includes:
- Regular vaccinations to prevent infections
- Monitoring for complications like splenic sequestration
- Healthy lifestyle choices, like a balanced diet and staying hydrated
Emerging Therapies
New therapies bring hope for sickle cell disease patients. These include:
- Gene therapy to fix the disease’s genetic cause
- Novel drugs, like voxelotor, that improve hemoglobin function
As research advances, we’ll see more innovative treatments. This will further improve patient outcomes.
Hemophilia: Understanding Clotting Disorders
It’s key to understand hemophilia to manage it well. Hemophilia is a bleeding disorder. It happens when there’s not enough clotting factors, which are proteins that stop bleeding.
Types of Hemophilia
There are two main types: Hemophilia A and Hemophilia B. Hemophilia A is caused by a lack of factor VIII. Hemophilia B is due to a lack of factor IX. Both lead to prolonged bleeding, which can cause serious health issues if not treated right.
Inheritance Patterns
Hemophilia is often passed down through genes. It’s X-linked recessive, meaning the genes are on the X chromosome. This is why it’s more common in males, who have only one X chromosome. Females can be carriers but it’s rare for them to have it.
Clinical Presentation and Severity
The symptoms of hemophilia vary by how severe the clotting factor deficiency is. Mild cases might only bleed after surgery or major injuries. Severe cases can have bleeding in joints or muscles without any injury. The severity is based on how much clotting factor is in the blood.
Knowing the symptoms and severity helps tailor treatments. This improves the quality of life for those with hemophilia.
Comprehensive Management of Hemophilia
Managing hemophilia well means using factor replacement therapy and prophylactic treatment. This approach greatly improves patients’ lives.
Factor Replacement Therapy
Factor replacement therapy is key in treating hemophilia. It involves giving the missing clotting factor to help blood clot normally.
- On-demand treatment: Stops bleeding episodes.
- Prophylactic treatment: Prevents bleeding by regular infusions.
The World Federation of Hemophilia says, “Prophylaxis is the best treatment for hemophilia A and B.”
Prophylactic Treatment Approaches
Prophylactic treatments have changed how we manage hemophilia. They cut down on bleeding and its problems.
- Primary prophylaxis: Starts before 3 years old.
- Secondary prophylaxis: Begins after many bleeding episodes.
Management of Bleeding Episodes
Handling bleeding episodes well is vital in hemophilia care. It means quick diagnosis and right treatment.
- Spotting bleeding symptoms early.
- Using clotting factor concentrates.
Gene Therapy and Future Directions
Gene therapy is a new hope for hemophilia treatment. It aims to fix the genetic problem at its source.
“Gene therapy could change hemophilia treatment, giving a cure for this serious disorder.”
” Hemophilia Expert
As research grows, we’ll see new treatments. These will make patient care even better.
Other Significant Blood Disorders
Several blood disorders, like thrombocytopenia, leukemia, lymphoma, and polycythemia, are important. They affect many people and have a big impact on health. These conditions are not as well-known as anemia or sickle cell disease but are just as significant.
Thrombocytopenia
Thrombocytopenia means you have too few platelets in your blood. Platelets help your blood clot. Without enough, you might bleed more easily.
Causes can include bone marrow problems or certain medicines. Symptoms include easy bruising and bleeding that doesn’t stop. Doctors use a CBC to diagnose and treat it, depending on the cause.
Leukemia
Leukemia is a blood cancer that grows out of control. It affects the blood and bone marrow. There are different types, like ALL and AML.
Symptoms include feeling tired, losing weight, and getting sick often. Doctors use blood tests and bone marrow exams to diagnose. Treatment can be chemotherapy, targeted therapy, or stem cell transplants.
Lymphoma
Lymphoma is a cancer of the immune system. It’s divided into Hodgkin and non-Hodgkin lymphoma. Each type needs a different treatment plan.
Signs include swollen lymph nodes and fever. Doctors use biopsies and imaging to diagnose. Treatment might be chemotherapy, radiation, or both, based on the type and stage.
Polycythemia
Polycythemia vera is a rare disorder that makes too many blood cells. This increases the risk of blood clots.
Symptoms include headaches and itching. Doctors use blood tests and sometimes bone marrow exams to diagnose. Treatment aims to prevent complications and may include phlebotomy and medications.
Diagnostic Approaches for Blood Disorders
Accurate diagnosis of blood disorders is key for good treatment and care. We use lab tests and clinical checks to find these conditions.
Complete Blood Count and Interpretation
A Complete Blood Count (CBC) is a basic test for blood disorders. It shows the blood’s parts, like red and white cells, and platelets. A CBC helps doctors spot problems that might mean a blood disorder.
For example, a CBC can spot anemia by showing low red blood cells or hemoglobin. It can also find infections or inflammation by looking at white blood cells.
Specialized Blood Tests
Specialized blood tests are also vital for diagnosing specific blood disorders. These include blood smear exams, reticulocyte counts, and erythropoietin tests.
For instance, a blood smear can diagnose sickle cell disease by seeing the sickle-shaped red blood cells.
Bone Marrow Examination
A bone marrow examination takes a bone marrow sample for analysis. It’s key for finding blood disorders like leukemia and lymphoma.
Looking at the bone marrow lets doctors check blood cell production and development. This helps find any problems or cancers.
Genetic Testing for Blood Disorders
Genetic testing is very important for blood disorders caused by genes, like hemophilia and sickle cell disease. These tests find the specific genetic changes that cause the condition.
Genetic testing helps not just in diagnosing but also in planning families. It shows the risk of passing the condition to future generations.
Treatment Modalities for Blood Disorders
Managing blood disorders needs a mix of treatments. This approach helps meet the complex needs of patients. A detailed treatment plan is key to better patient outcomes.
Pharmacological Interventions
Medicines are essential in treating blood disorders. They help make more blood cells, stop bleeding, or prevent clots. For example, iron pills or special medicines can help with anemia.
“Pharmacological agents have changed how we treat blood disorders,” says a top hematologist. “They offer targeted and effective treatments.”
We use many medicines, including:
- Iron supplements for iron deficiency anemia
- Anticoagulants to prevent thrombosis
- Corticosteroids to manage immune-mediated blood disorders
- Immunosuppressants to treat conditions like aplastic anemia
Blood Transfusion Therapy
Blood transfusions are also key in treating blood disorders. They replace missing or damaged blood cells. This improves oxygen delivery and lowers bleeding risks.
We make sure blood transfusions are safe. We match blood types carefully to avoid bad reactions.
The benefits of blood transfusions include:
- Quick improvement in oxygen delivery to tissues
- Lower risk of bleeding
- Help for patients having surgery or chemotherapy
Stem Cell Transplantation
Stem cell transplantation can cure some blood disorders, like leukemia and lymphoma. It replaces the patient’s bad bone marrow with healthy stem cells. These can come from the patient or a donor.
We consider stem cell transplants for patients with:
- Severe aplastic anemia
- Acute leukemia
- Certain types of lymphoma
Surgical Approaches
Surgery is needed for some blood disorders, like splenectomy for hypersplenism. We work with surgical teams to give patients full care.
Surgical options include:
- Splenectomy for conditions like hereditary spherocytosis
- Surgical repair of bleeding sites
- Insertion of vascular access devices for chemotherapy or transfusion
In conclusion, treating blood disorders requires many approaches, from medicines to surgery. Knowing these options helps us tailor care to each patient’s needs.
Living with Chronic Blood Disorders
People with chronic blood disorders face many challenges. They deal with physical, emotional, and psychological hurdles. To manage these conditions, a mix of medical care, lifestyle changes, and mental support is needed.
Psychological Impact
Getting a diagnosis of a chronic blood disorder can deeply affect a person. They might feel anxious, depressed, or scared. The emotional weight can be as heavy as the physical symptoms, impacting their life quality.
Research shows that those with chronic illnesses, like blood disorders, are more likely to struggle with mental health. It’s important to treat the mind as well as the body.
Lifestyle Adaptations
Living with chronic blood disorders means making big lifestyle changes. This includes eating differently, avoiding certain activities, and sticking to medication.
For example, people with anemia might eat more iron-rich foods. Those with hemophilia might avoid sports to avoid injuries. Making these lifestyle changes is key to managing symptoms and improving life quality.
| Lifestyle Adaptation | Benefit |
| Dietary Changes | Helps manage symptoms and improve overall health |
| Avoiding Risky Activities | Reduces the risk of complications associated with the disorder |
| Medication Adherence | Essential for managing the condition and preventing complications |
Support Systems and Resources
Having a strong support system is essential for those with chronic blood disorders. This includes family, friends, healthcare providers, and support groups. Connecting with others who get it can offer emotional support and useful advice.
There are also many resources to help manage these conditions. These include educational materials, counseling, and online forums.
Quality of Life Considerations
Improving life quality is a main goal in managing chronic blood disorders. It’s not just about controlling symptoms but also dealing with the emotional and social impacts.
By taking a holistic approach to care, patients can live full and meaningful lives despite their condition. Improving life quality should be the focus of any treatment plan.
Prevention and Risk Reduction Strategies
It’s important to know how to prevent blood disorders. By taking action early, we can lower our risk of getting these conditions.
Nutritional Approaches
Eating right is key to avoiding some blood disorders. Nutritional deficiencies, like iron lack, can cause anemia. It’s vital to get all the nutrients we need.
- Iron-rich foods can help prevent iron deficiency anemia.
- Folate and vitamin B12 are essential for preventing megaloblastic anemia.
- A balanced diet that includes fruits, vegetables, and whole grains keeps us healthy.
Genetic Counseling
If you have a family history of genetic blood disorders, genetic counseling is helpful. It helps figure out your risk of passing on these conditions to your kids.
Genetic counseling helps you make smart choices about having children. It also helps you manage your risk.
Screening Programs
Screening programs are key for catching blood disorders early. Regular health checks and screenings can spot problems before they start.
- Newborn screening programs can find certain blood disorders early in life.
- Regular blood tests can check blood cell counts and find any issues.
Public Health Initiatives
Public health initiatives are vital for spreading awareness and prevention of blood disorders. These efforts include educational campaigns, community programs, and funding for research.
Together, we can lessen the impact of blood disorders. This improves the lives of those affected.
Research Frontiers in Blood Disorders
Recent breakthroughs in gene therapy and personalized medicine are changing how we treat blood disorders. Our understanding of these complex conditions is getting better as we explore new research areas.
Advances in Gene Therapy
Gene therapy is a promising way to treat genetic blood disorders. It aims to fix or replace the faulty gene causing the condition. This could lead to a cure. We’re seeing big steps forward, with trials for sickle cell disease and hemophilia underway.
Using viral vectors to deliver the gene to cells has shown great promise. For example, lentiviral vectors have been used to treat beta-thalassemia and sickle cell disease. This shows they can fix the genetic defect for a long time.
| Disease | Gene Therapy Approach | Status |
| Sickle Cell Disease | Lentiviral Vector | Clinical Trials |
| Hemophilia A | AAV Vector | Ongoing Research |
| Beta-Thalassemia | Lentiviral Vector | Clinical Trials |
Novel Therapeutic Agents
Researchers are also working on new treatments for blood disorders. These include small molecule inhibitors and monoclonal antibodies that target specific disease pathways.
For sickle cell disease, new treatments aim to reduce painful crises. For hemophilia, researchers are exploring new factor replacement therapies and non-factor treatments. These could improve treatment outcomes and reduce patient burden.
Global Research Collaborations
Dealing with blood disorders requires a team effort. Global research collaborations bring together experts from different fields and places. This sharing of knowledge and resources speeds up the discovery of new treatments.
Groups like the Blood Disorders Research Consortium help share best practices and coordinate research worldwide. These collaborations are key to advancing the field and finding effective treatments.
Personalized Medicine Approaches
Personalized medicine is changing how we treat blood disorders. It tailors treatments to each patient’s genetic and molecular profile. Advances in genetic sequencing and biomarker identification help predict how patients will respond to treatments.
In leukemia, genetic profiling helps find the best targeted therapies. For hemophilia, knowing the patient’s genetic mutation helps choose the right factor replacement therapy.
As we move forward in these research areas, the future of treating blood disorders looks bright. We’re on the path to more effective and personalized treatments.
Conclusion
Blood disorders are big health issues affecting millions globally. We’ve looked at the three main ones: anemia, sickle cell disease, and hemophilia. Knowing about these is key to better care and outcomes.
Anemia is the most common, caused by too few red blood cells or hemoglobin. Sickle cell disease and hemophilia also have a big impact. Knowing how to spot symptoms and treat them is vital for doctors.
New research and treatments, like gene therapy, offer hope. Keeping up with new findings and using preventive steps can help people live better lives.
Dealing with blood disorders needs teamwork between patients, doctors, and researchers. Together, we can learn more and find better ways to treat these conditions. This will help improve life for those with blood disorders.
FAQ
What are the three most common blood disorders?
The top three blood disorders are anemia, leukemia, and lymphoma. These issues affect millions globally, impacting their lives greatly.
What is anemia, and what are its symptoms?
Anemia is when you don’t have enough red blood cells or hemoglobin. Symptoms include feeling tired, weak, and short of breath. There are different types, like iron deficiency and sickle cell anemia.
How is iron deficiency anemia diagnosed and treated?
Doctors use physical checks, medical history, and lab tests to find iron deficiency anemia. These tests include a complete blood count and iron tests. Treatment often means taking iron supplements and eating more iron-rich foods.
What is sickle cell disease, and how is it managed?
Sickle cell disease is a genetic issue that messes with hemoglobin, making red blood cells break down. To manage it, doctors focus on pain relief, preventive care, and new treatments like gene therapy.
What is hemophilia, and how is it treated?
Hemophilia is a bleeding disorder due to missing clotting factors. Treatment usually involves replacing these factors, preventing bleeding, and managing any episodes.
What are the symptoms and treatment options for leukemia and lymphoma?
Leukemia and lymphoma are cancers that can make you feel tired, lose weight, and have swollen lymph nodes. Doctors treat them with chemotherapy, radiation, and sometimes stem cell transplants.
How are blood disorders diagnosed?
Doctors use lab tests like complete blood counts, specialized tests, bone marrow exams, and genetic tests to diagnose blood disorders.
What are the treatment modalities for blood disorders?
Treatments for blood disorders include medicines, blood transfusions, stem cell transplants, and surgery.
How can patients live with chronic blood disorders?
Patients with chronic blood disorders need a full plan. This includes mental support, making lifestyle changes, and finding support groups and resources.
What are the prevention and risk reduction strategies for blood disorders?
To prevent blood disorders, focus on good nutrition, genetic counseling, screening, and public health efforts.
What are the current research frontiers in blood disorders?
Research is advancing with gene therapy, new medicines, global studies, and personalized care.
References
Modell, B., & Darlison, M. (2008). Global epidemiology of haemoglobin disorders and derived service indicators. Bulletin of the World Health Organization, 86(6), 480-487. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2647473/
World Health Organization. (2025, February 9). Anaemia. https://www.who.int/news-room/fact-sheets/detail/anaemia