Blood clots can take many forms, from hard to jelly-like. Their shape and size depend on where they form and what they’re made of. At Liv Hospital, we know that blood clots are a natural response to injury. But when they form in the wrong way, they can cause serious health problems.
We look into the different types of blood clots, what makes them unique, and what causes them. Blood clots can occur in arteries or veins in your heart, brain, lungs, abdomen, arms, and legs. Knowing about these variations is key to finding and treating them.
Key Takeaways
- Blood clots can be hard or jelly-like, depending on their composition.
- They can occur in various parts of the body, including arteries and veins.
- Abnormal blood clot formation can lead to serious health issues.
- Understanding different blood clot types is critical for diagnosis.
- Liv Hospital is dedicated to providing trusted, patient-focused care.
The Science Behind Blood Clotting
Learning about blood clotting is key to understanding its importance. It’s a complex process that stops bleeding when a blood vessel is injured. This process is vital but can also be dangerous.
Normal Clotting Process: A Life-Saving Mechanism
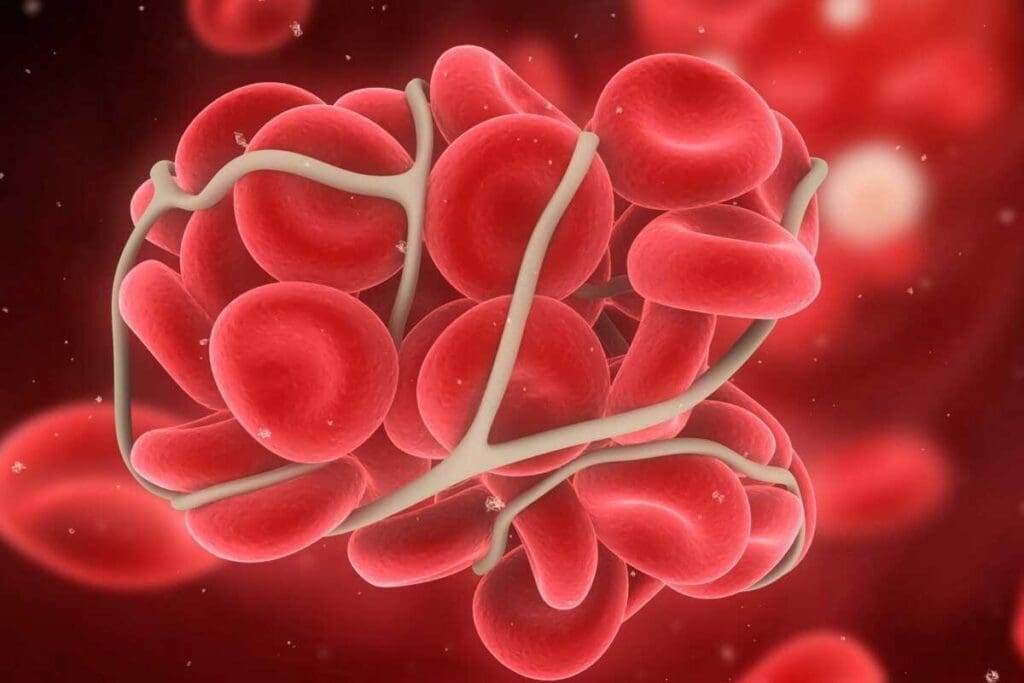
The clotting process starts when platelets meet the injured blood vessel. They form a platelet plug. Coagulation factors then help create a fibrin clot, making the plug stable.
There are two main types of blood clots. Arterial clots are mostly platelets and are linked to artery diseases. Venous clots, rich in red blood cells, are found in veins.
When Clotting Goes Wrong: Pathological Thrombus Formation
But sometimes, clotting goes wrong. This leads to a pathological thrombus. A thrombus is a clot that stays in a blood vessel and can block blood flow. If it moves, it becomes an embolus and can block other parts of the body.
| Type of Clot | Description | Characteristics |
| Thrombus | Stationary blood clot | Remains in one place, potentially blocking blood flow |
| Embolus | Moving blood clot | Travels through the bloodstream, potentially causing blockages elsewhere |
Knowing the difference between a stationary clot (thrombus) and a moving clot (embolus) is vital. This knowledge helps doctors diagnose and treat blood clots.
Understanding the Different Types of Blood Clots
Blood clots vary in type, each with its own risks and characteristics. The type of clot depends on its composition and where it forms. Let’s look at the main types of blood clots and their differences.
Arterial (White) Thrombi: Platelet-Rich Clots
Arterial thrombi, or white thrombi, are made mostly of platelets. They usually form in arteries. These clots happen when platelets gather at injuries or inflammation in artery walls.
Arterial clots can block blood and oxygen to vital organs. This can cause tissue damage or organ failure. For example, a clot in a coronary artery can lead to a heart attack by blocking blood to the heart muscle.
High blood pressure, atherosclerosis, and other heart conditions can cause arterial thrombi. Knowing the risks and how these clots form is key to preventing and treating them.
Venous (Red) Thrombi: Red Blood Cell-Rich Clots
Venous thrombi, or red thrombi, are full of red blood cells and found in veins. They form more slowly than arterial clots and are linked to deep vein thrombosis (DVT). Venous clots can be very serious and can lead to pulmonary embolism if they break loose.
The makeup of venous thrombi is influenced by blood flow, vessel injury, and how prone the blood is. Spotting signs like swelling and pain in a limb is vital for early treatment.
The Difference in Composition and Formation
Arterial and venous thrombi differ in what they’re made of and how they form. Arterial clots are platelet-rich and form fast after artery injury. Venous clots are red blood cell-rich and grow slower.
| Characteristics | Arterial Thrombi | Venous Thrombi |
| Primary Composition | Platelets | Red Blood Cells |
| Typical Location | Arteries | Veins |
| Formation Speed | Rapid | Gradual |
| Common Risk Factors | Atherosclerosis, High Blood Pressure | Immobility, Hypercoagulability |
Stationary vs. Moving Blood Clots: Terminology Explained
It’s important to know the difference between stationary and moving blood clots. This knowledge helps doctors diagnose and treat heart problems better. Blood clots can form anywhere in the body. They can stay in one place or move through the blood, affecting health differently.
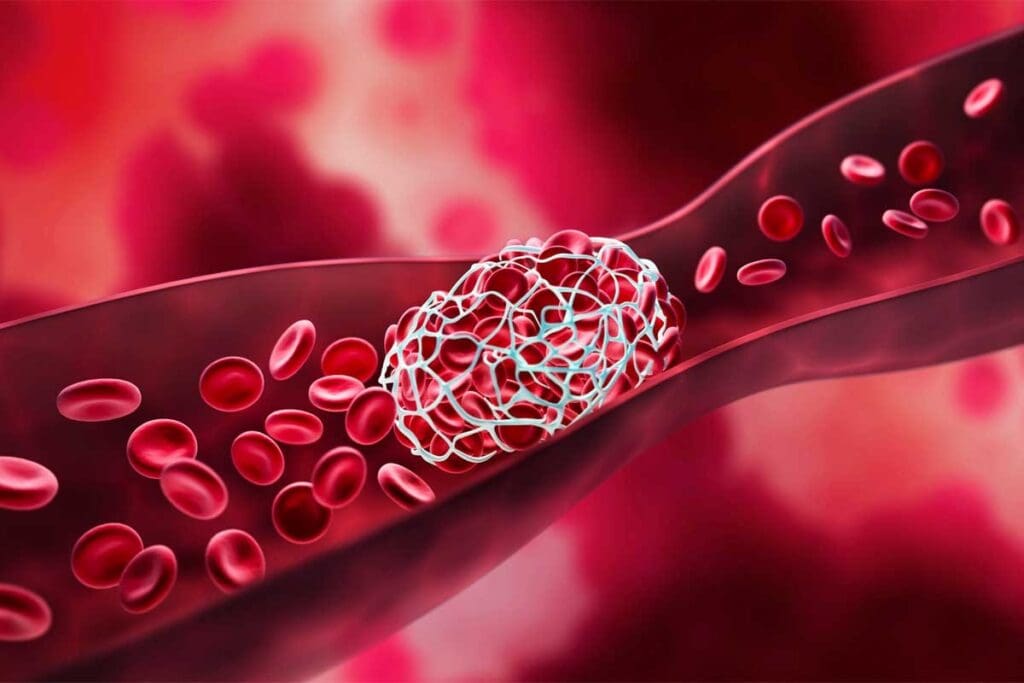
Thrombus: The Stationary Blood Clot
A thrombus is a blood clot that stays in one place in a blood vessel. It can block blood flow and harm the tissue around it. The clot forms due to blood composition and the condition of the blood vessel walls.
Embolus: When Blood Clots Travel Through Circulation
An embolus is a blood clot that moves through the blood. It can get stuck in a smaller vessel, causing serious problems. This can lead to issues like a pulmonary embolism or stroke.
The Danger of Transformation: When Thrombi Become Emboli
When a thrombus turns into an embolus, it’s a serious situation. A piece of the clot breaks off and travels, causing blockages in other parts of the body. This shows why treating thrombi quickly is so important.
Doctors need to know the difference between thrombi and emboli to understand the risks. This knowledge helps them choose the right treatment. It’s key to managing both stationary and moving blood clots effectively.
7 Types of Blood Clots Based on Location
It’s important to know about the different blood clots and where they form. This helps doctors find the best treatment for each patient. Blood clots can happen in many places in the body.
Deep Vein Thrombosis (DVT): Clots in the Deep Veins
Deep Vein Thrombosis (DVT) happens in the deep veins, usually in the legs. It can cause a lot of pain and swelling. If the clot breaks loose, it can lead to a Pulmonary Embolism (PE). Seek medical help right away if you have leg pain or swelling.
Pulmonary Embolism (PE): Clots in the Lungs
A Pulmonary Embolism (PE) is when a clot from the leg travels to the lungs. It’s very dangerous because it can block blood flow. Look out for symptoms like shortness of breath, chest pain, and coughing up blood. Get medical help fast if you notice these signs.
Coronary Thrombosis: Clots in the Heart
Coronary Thrombosis is when a clot forms in the heart’s blood vessels. It can cause a heart attack by stopping blood flow. You might feel chest pain or discomfort. A doctor said, “Coronary thrombosis is a big problem worldwide.”
“Coronary thrombosis is a medical emergency that requires immediate attention to restore blood flow to the heart.”
— Senior Cardiologist
Cerebral Thrombosis and Embolism: Clots in the Brain
Cerebral Thrombosis is a clot in the brain’s blood vessels. Cerebral Embolism is when a clot from elsewhere reaches the brain. Both can cause a stroke. Look out for symptoms like weakness, vision changes, and trouble speaking. Get medical help quickly to prevent brain damage.
In summary, knowing about blood clots and where they form is key for good medical care. Each type of clot has its own risks and needs. Understanding these differences helps doctors treat patients better.
The Texture Spectrum of Blood Clots
Blood clots can be soft and jelly-like or hard and organized. This difference shows how complex clotting is. It depends on where the clot forms and how old it is.
Soft, Jelly-Like Blood Clots: Characteristics and Formation
Soft, jelly-like clots are common in heavy menstrual bleeding. They have lots of red blood cells and feel gelatinous. The body makes these clots quickly to stop bleeding.
Hard, Organized Blood Clots: Structure and Development
Hard, organized clots are more structured. They have more platelets and fibrin. These clots are found in deep vein thrombosis (DVT) and are firm. They form through a process where the initial clot matures.
How Age and Location Affect Clot Consistency
The age and location of a clot change its consistency. Older clots are harder, while younger ones are softer. Clots in veins are red and full of red blood cells. Clots in arteries are white and have more platelets.
| Clot Characteristic | Soft/Jelly-Like Clots | Hard/Organized Clots |
| Composition | High proportion of red blood cells | High proportion of platelets and fibrin |
| Typical Location | Often associated with menstrual bleeding | Commonly found in DVT and arterial thrombosis |
| Texture | Gelatinous or jelly-like | Firm and stable |
Microclots: Small But Significant
Microclots are small but very important in health issues like long COVID and chronic ischemia. They can block tiny blood vessels, causing health problems. Knowing about microclots helps doctors diagnose and treat these conditions.
What Sets Microclots Apart
Microclots are different from big clots because of their size and how they affect the body. Big clots can cause serious symptoms right away. But microclots might lead to long-term or mild health problems. They are hard to find with the usual tests because they are so small.
Key characteristics of microclots include:
- Small size, often obstructing capillaries
- Potential to cause chronic health issues
- Difficulty in detection using standard methods
- Association with conditions like long COVID and chronic ischemia
The Role of Microclots in Health Conditions
Studies show microclots play a big part in health issues. In long COVID, they can keep symptoms going by blocking blood flow. In chronic ischemia, they make the condition worse by cutting off blood to areas that need it.
Understanding microclots helps doctors find better ways to diagnose and treat these conditions. For example, finding microclots in long COVID patients could lead to new treatments that help improve symptoms.
Detection Challenges and Research Developments
Finding microclots is hard because they are small and current tests can’t see them well. But scientists are working on new ways to spot and count microclots. They are using advanced imaging and special blood tests.
Emerging research areas include:
- Advanced imaging techniques for microclot detection
- Specialized blood tests to identify microclot-related biomarkers
- Studies on the role of microclots in various health conditions
- Development of targeted therapies for microclot resolution
As research goes on, we’ll learn more about microclots and how they affect our health. This knowledge will help doctors find better ways to diagnose and treat conditions linked to microclots.
Epidemiology of Blood Clots in the United States
It’s important to understand blood clots to tackle their health issues in the US. Knowing how common they are helps in planning for public health and healthcare.
Venous Thromboembolism: 900,000 Cases Annually
Venous thromboembolism (VTE) includes deep vein thrombosis (DVT) and pulmonary embolism (PE). It affects up to 900,000 people in the US each year, says the American Heart Association. This number shows we need to spread awareness and take steps to prevent it.
VTE’s effects go beyond the immediate issue. It also leads to long-term health problems and high healthcare costs. It’s key to manage and prevent VTE to lessen these impacts.
Demographic Patterns in Blood Clot Formation
Demographic factors like age, gender, and ethnicity are key in blood clot epidemiology. These factors affect the risk of getting blood clots.
- Age: Blood clot risk grows with age, more so after 40.
- Gender: Men might face a higher VTE risk than women, but women’s risk goes up during pregnancy and with hormone therapy.
- Ethnicity: Some ethnic groups might be more prone to blood clots due to genetics.
Mortality and Morbidity Statistics
Blood clots lead to a lot of deaths and health issues each year. VTE causes a significant number of deaths, many of which could be prevented with the right care.
VTE is a top cause of death in hospitalized patients. Also, those who survive VTE often face long-term health problems like post-thrombotic syndrome and chronic thromboembolic pulmonary hypertension.
The data on blood clots show we need more research, better prevention, and better care for patients. This can help reduce their occurrence and impact.
Risk Factors for Developing Different Types of Blood Clots
Blood clots can form due to genetics, lifestyle, and health issues. Knowing these risk factors helps prevent and treat blood clot conditions early.
Genetic Predispositions and Inherited Clotting Disorders
Genetics plays a big role in blood clot formation. Disorders like Factor V Leiden and Antithrombin III deficiency raise the risk of VTE.
Lifestyle Factors: Immobility, Smoking, and Obesity
Lifestyle choices also affect blood clot risk. Being immobile for long, smoking, and being obese are major factors. For example, long flights or bed rest can cause DVT.
Medical Conditions That Increase Clotting Risk
Some health conditions increase blood clot risk. These include cancer, heart disease, and autoimmune disorders. For instance, cancer patients are at a higher risk of VTE due to tumor cells.
Medications That Can Trigger Clot Formation
Some medicines can also cause blood clots. Hormonal contraceptives, HRT, and some chemotherapy agents are examples. It’s important to consider these risks, even with other risk factors.
| Risk Factor Category | Specific Risk Factors |
| Genetic | Factor V Leiden, Antithrombin III deficiency |
| Lifestyle | Immobility, smoking, and obesity |
| Medical Conditions | Cancer, heart disease, and autoimmune disorders |
| Medications | Hormonal contraceptives, HRT, chemotherapy agents |
“The interplay between genetic predispositions, lifestyle factors, and medical conditions can significantly influence an individual’s risk of developing blood clots.”
Diagnosis and Treatment Approaches for Various Blood Clot Types
Diagnosing and treating blood clots needs a careful approach. Each clot’s type and location affect both diagnosis and treatment. This is why different strategies are used for different clots.
Recognizing Symptoms Based on Clot Location
Symptoms of blood clots vary based on where they are. For example, deep vein thrombosis (DVT) causes swelling, pain, and warmth in the affected limb. On the other hand, a pulmonary embolism (PE) might lead to sudden shortness of breath, chest pain, and serious complications.
It’s important to spot these symptoms early. This way, we can act quickly. Knowing how blood clots present differently helps us give the right care.
Diagnostic Procedures: From D-dimer Tests to Advanced Imaging
Diagnosing blood clots involves several tests. These include simple blood tests like the D-dimer assay and advanced imaging like ultrasound and computed tomography (CT) scans. The right test depends on the clot’s location and type.
D-dimer tests are often the first step because they’re very sensitive. But they’re not always specific. Advanced imaging gives more detailed info about the clot’s size, location, and how it affects nearby tissues.
Treatment Strategies: Anticoagulants, Thrombolytics, and Surgical Options
Treatment for blood clots is tailored to each patient. It considers the clot’s location, the patient’s health, and the risk of complications. Anticoagulants are used to stop clot growth and prevent new ones. Thrombolytics are used for severe cases where quick clot dissolution is needed.
In some cases, surgical intervention is needed to remove the clot or repair damaged vessels. We carefully consider the benefits and risks of each treatment to ensure the best outcome for our patients.
Emerging Therapies and Clinical Trials
The field of blood clot management is always changing. New treatments and technologies are being developed. Emerging treatments include new anticoagulants and targeted therapies that focus on specific clot formation.
Joining clinical trials gives patients access to new treatments and helps advance medical knowledge. We’re committed to keeping up with these advancements to provide the best care for our patients.
Conclusion: The Importance of Understanding Blood Clot Diversity
It’s key to know about different blood clots for good care. Clots can show up in many ways and places. This means we need to understand them well to treat them right.
There are many kinds of blood clots, each with its own risks. Knowing about these helps doctors find the best way to help patients. This way, they can treat each case differently.
We’ve talked about how blood clots can be hard or soft. Knowing this helps doctors make better choices for their patients. As we learn more about blood clots, we can find better ways to stop them and treat them.
FAQ
What are the different types of blood clots?
Blood clots come in two main types. Arterial (white) thrombi form in arteries and are hard. Venous (red) thrombi form in veins and are soft.
What is the difference between a thrombus and an embolus?
A thrombus stays in one place in a blood vessel. An embolus moves through the blood and can block other areas.
What is a deep vein thrombosis (DVT)?
A DVT is a blood clot in the deep veins, usually in the legs.
Are blood clots hard or soft?
Blood clots can be soft and jelly-like or hard and organized. This depends on their age and where they form.
What are microclots?
Microclots are small clots in the tiny blood vessels. They are linked to long COVID and chronic ischemia.
What are the risk factors for developing blood clots?
Risk factors include genetics, lifestyle choices like immobility and smoking, and certain health conditions.
How are blood clots diagnosed?
Doctors use tests like D-dimer tests, ultrasound, and imaging to find blood clots.
What are the treatment options for blood clots?
Treatment includes anticoagulants, thrombolytics, and surgery. It depends on the clot’s type and location.
Can blood clots be prevented?
Yes, by managing risk factors. This includes staying active, avoiding smoking, and keeping a healthy weight.
What is the epidemiology of blood clots in the United States?
In the U.S., venous thromboembolism affects about 900,000 people each year. It causes a lot of illness and death.
What is a moving blood clot called?
A moving clot is called an embolus.
What is a stationary clot called?
A clot that doesn’t move is called a thrombus.
Are there different kinds of blood clots based on their location?
Yes, clots are classified by location. This includes DVT, PE, coronary thrombosis, and cerebral thrombosis and embolism.
References:
- Arber, D. A., Orazi, A., Hasserjian, R., Thiele, J., Borowitz, M. J., Le Beau, M. M., Bloomfield, C. D., Cazzola, M., & Vardiman, J. W. (2016). The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood, 127(20), 2391–2405. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4876473/


































