Last Updated on December 2, 2025 by Bilal Hasdemir
Page readers will be shocked. Almost 30% of patients experience some form ofnauseaor vomiting. Is vomiting after colon surgery normal? Get the facts. This critical warning sign could mean an ileus or something more serious.
Colon surgery is a big challenge. Symptoms like vomiting can worry patients. We know that nausea and vomiting are common after surgery.
We are here to help guide you through your postoperative symptoms. We want to make sure you get the care you need during recovery.
Key Takeaways
- erstwhile causes of postoperative nausea and vomiting.
- Strategies for managing and alleviating these symptoms.
- The importance of postoperative care in preventing complications.
- How to identify when to seek medical attention for postoperative symptoms.
- Tips for a smooth and comfortable recovery process.
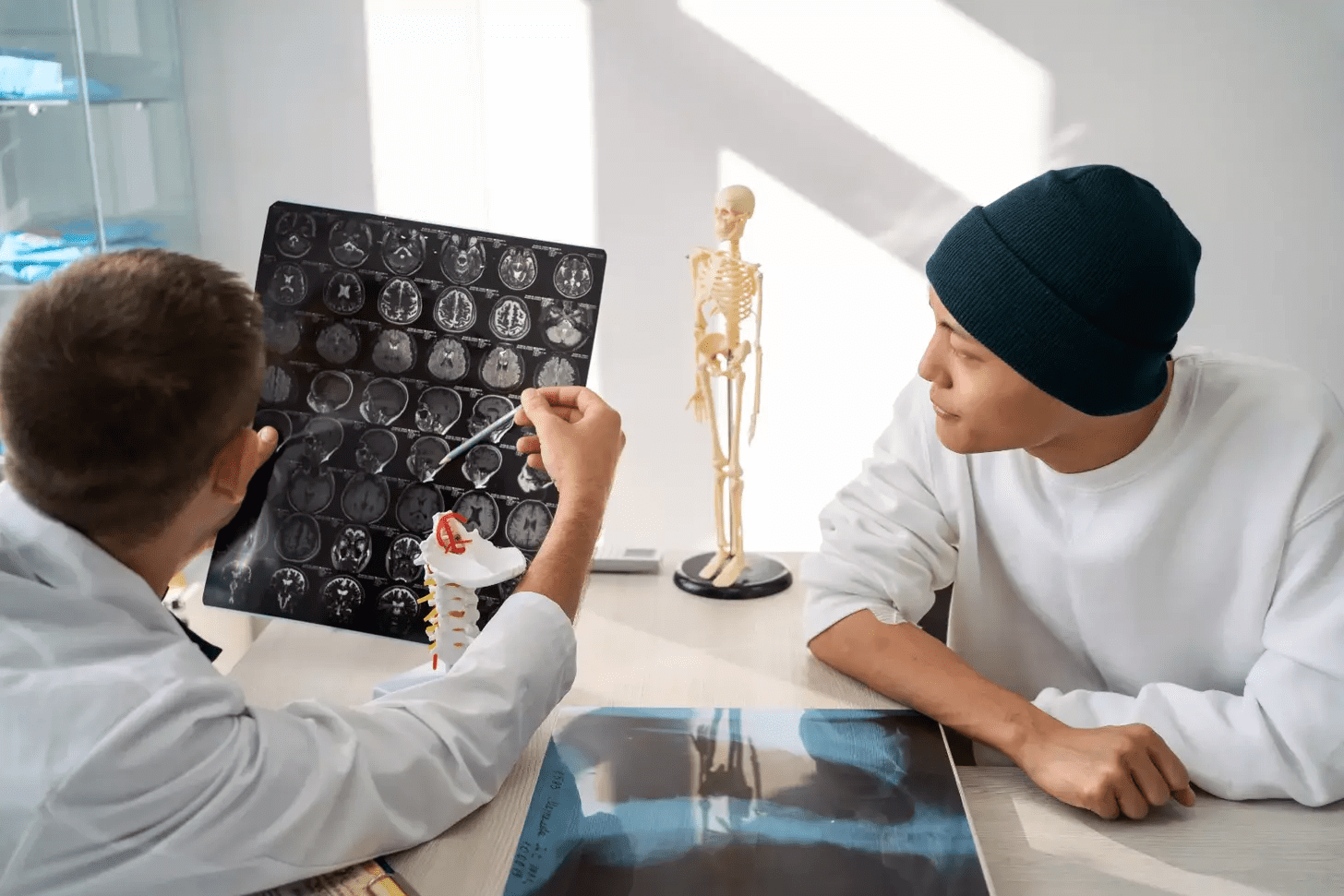
Understanding Colon Surgery and Its Purpose
Colon surgery is complex and involves many aspects. It treats colon-related issues and can greatly improve a patient’s life. Understanding the types, reasons, and potential complications is essential.
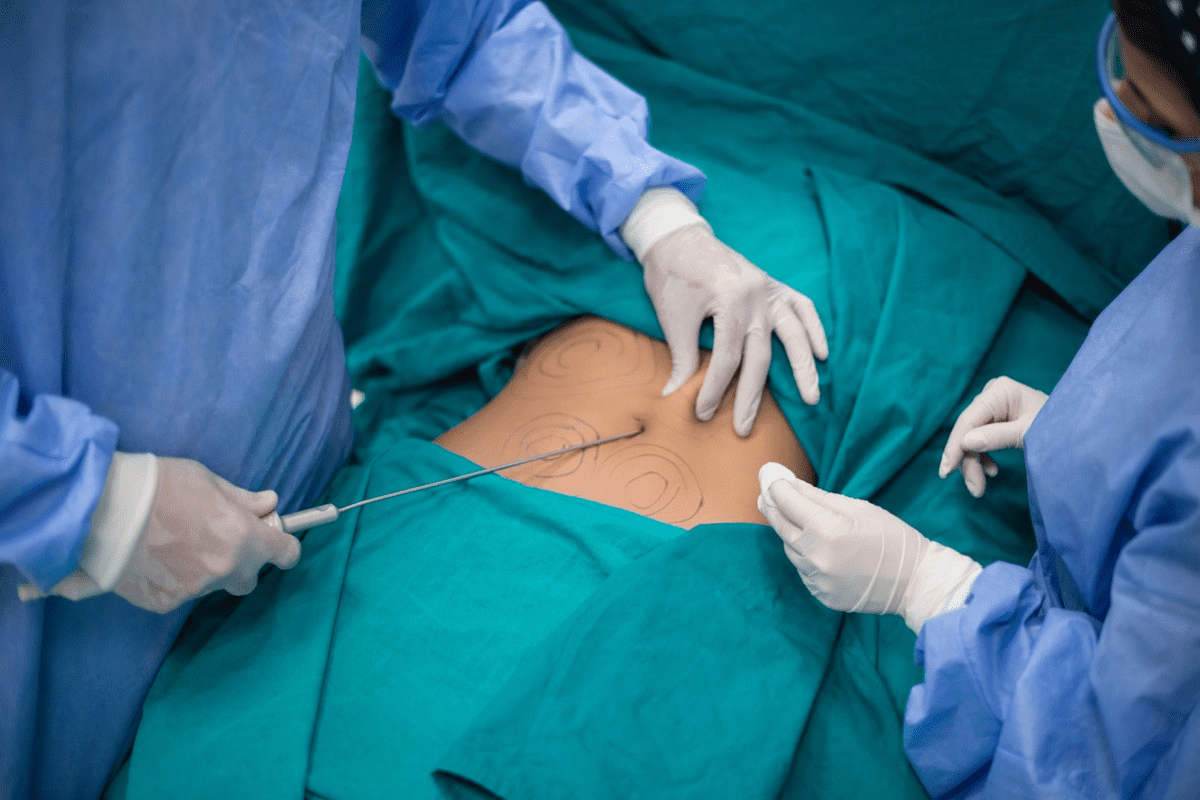
Types of Colon Surgery
There are different types of colon surgery, each for specific reasons and methods. These include:
- Colectomy: Removing part or all of the colon.
- Proctocolectomy: Taking out the colon and rectum.
- Anterior Resection: Removing the sigmoid colon and rectum.
These surgeries help treat issues like colon cancer and diverticulitis.
Reasons for Undergoing Surgery
People may need colon surgery for several reasons. These include:
- Colon Cancer: To remove cancerous tumors.
- Diverticulitis: Treating complications like abscesses or perforations.
- Inflammatory Bowel Disease (IBD): Managing severe ulcerative colitis or Crohn’s disease.
Knowing why you need surgery helps prepare for recovery.
Common Risks and Complications
Colon surgery comes with risks and complications. These include:
- Infection: Bacterial infections at the surgical site.
- Bleeding: Excessive bleeding during or after surgery.
- Adhesions: Scar tissue that can cause bowel obstruction.
Knowing these risks helps patients spot symptoms early and get help quickly.
Why Vomiting Occurs After Colon Surgery
Understanding why vomiting happens after colon surgery can ease worries and help patients recover better. Vomiting is a symptom caused by several factors related to the surgery and how the body reacts to it.
Effects of Anesthesia
Anesthesia is a main reason for vomiting after colon surgery. It’s used to prevent pain during surgery. But, it can also upset the stomach, causing nausea and vomiting. The type and amount of anesthesia used can affect how bad these symptoms are.
- General anesthesia, which makes patients unconscious, is more likely to cause nausea and vomiting than local or regional anesthesia.
- Certain anesthetic agents can slow down bowel movements, leading to nausea.
Postoperative Recovery Process
The body’s response to surgery also affects vomiting after colon surgery. After surgery, the body heals, recovers from anesthesia, and gets back to normal. This process includes inflammation, pain, and discomfort, which can cause nausea and vomiting.
It’s important to manage pain well and follow postoperative care instructions to reduce these symptoms.
Changes in Diet and Digestion
Changes in diet and digestion are also key factors. After colon surgery, digestive function changes. This can lead to slowed bowel movements or different food processing. Patients may feel nauseous when starting to eat again.
- Starting with clear liquids and gradually moving to solid foods can help manage these issues.
- It’s best to avoid heavy or greasy foods in the early recovery period.
By understanding these factors, patients can better manage their recovery from colon surgery and deal with symptoms like vomiting more effectively.
When Is Vomiting Considered Normal?
Knowing when vomiting is normal after colon surgery helps patients recover better. The post-surgery period can be tough. It’s key to tell normal side effects from serious problems.
Typical Timeline for Recovery
Recovery times after colon surgery vary. But most people start feeling better in a few weeks. Vomiting usually peaks in the first few days. We watch patients closely during this time to handle any bad symptoms.
Duration of Nausea and Vomiting
Nausea and vomiting can last from a few days to a week. The surgery type, health, and how well you handle anesthesia play a role. Following post-surgery care closely can help reduce these symptoms.
Post-Surgery Day | Expected Symptoms | We are here to help guide you through your postoperative symptoms. |
1-3 | Nausea, vomiting, discomfort | Follow prescribed medication regimen, stay hydrated |
4-7 | Gradual reduction in nausea, possible return to light diet | Continue medication as needed, introduce bland foods |
7+ | Significant improvement, return to normal diet | Resume normal activities gradually, monitor for any unusual symptoms |
Indicators of Normal Recovery
Signs of normal recovery include less vomiting, better appetite, and feeling better overall. Patients should start feeling normal again in a few weeks. Regular check-ups are vital to track recovery.
Understanding post-surgery care helps patients know when to worry. This knowledge makes the recovery journey smoother.
[Сontent section5 article] Westrong Page Page emphasize the importance recognizing these signs early.
“Early detection health issues significantly improves patient outcomes.”
Page Let’s discuss some key complications.
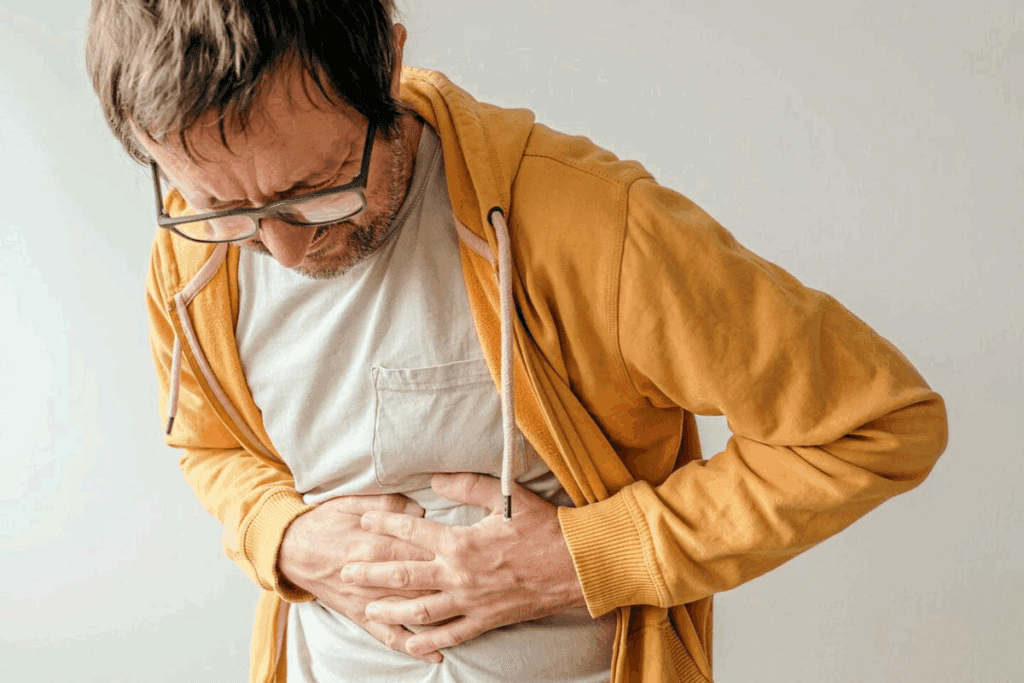
Signs Infection
Watching signs like fever chillsiv, andincreased heart sanfranis important.
Potential Bowel Obstruction
Bowel obstruction is another serious issue. Symptoms include severe abdominal pain, bloating, and trouble passing stool or gas.
Dehydration Risks
Vomiting can quickly , Page 2 characterized excessive thirst, dark urine, d Page dizziness. Ensuring adequate hydration is vital.
- Monitoring urine output
- Recognizing signs dehydration
By being aware of these complications, patients can take proactive steps to manage their recovery effectively.
Management of Vomiting After Surgery
Managing vomiting after colon surgery is key for a smooth recovery. Vomiting can cause dehydration and electrolyte imbalances. It can also lead to longer hospital stays. We’ll share strategies to help manage vomiting and make recovery easier.
Dietary Recommendations
Changing your diet after colon surgery can help reduce vomiting. Start with clear liquids like broth or electrolyte-rich drinks. Then, slowly add more solid foods.
- Start with small, frequent meals to ease digestion.
- Avoid spicy, fatty, or heavy foods that can irritate the stomach.
- Choose bland foods like crackers, toast, or plain rice.
It’s important to stay hydrated by drinking lots of fluids. But, avoid caffeinated or carbonated drinks as they can make nausea worse.
Medications for Nausea Relief
Medications might be needed to control nausea and vomiting. Antiemetics are designed to prevent or reduce nausea.
It’s vital to follow the dosage and instructions given by your doctor. This helps the medication work best and avoids side effects.
Importance of Hydration
Keeping hydrated is very important after colon surgery, even with vomiting. Dehydration can cause serious problems like electrolyte imbalances and low blood pressure.
We are here to help guide you through your postoperative symptoms.
- Drink small amounts of fluid often.
- Check your urine to make sure it’s pale yellow or clear.
- Use electrolyte-rich drinks or supplements if your doctor suggests it.
By following these tips, patients can manage vomiting after colon surgery. This helps reduce discomfort and supports a better recovery.
When to Contact Your Healthcare Provider
After colon surgery, it’s key to watch your health closely. We’ll help you know when to reach out to your doctor. We’ll talk about when to seek more medical help, the role of follow-up care, and how a symptom diary aids in your healing.
Warning Signs to Look For
Knowing the warning signs for complications after colon surgery is vital. These include:
- Severe abdominal pain that doesn’t get better with medicine.
- Vomiting blood or constant vomiting.
- Fever over 101.5°F (38.6°C).
- Increasing redness, swelling, or discharge from the surgery area.
If you notice any of these signs, don’t wait to call your healthcare provider.
Recommended Follow-Up Care
Follow-up care is a big part of getting better. Your doctor will check on you regularly. At these visits, make sure to:
- Talk about any worries or symptoms you have.
- Check your medicine list.
- Get advice on slowly getting back to your usual activities.
Keeping a Symptom Diary
Keeping a symptom diary is very helpful during your recovery. It lets you track your symptoms, medicine, and important events. This helps you:
- Spot patterns or issues that need attention.
- Give your doctor all the details at check-ups.
- Feel more in charge of your healing journey.
We suggest keeping your diary current and sharing it with your doctor at your follow-up visits.
Emotional and Psychological Factors
Recovering from colon surgery is more than just physical. It also involves emotional and psychological aspects. These factors greatly affect a patient’s overall well-being. As patients go through recovery, they feel many emotions, like anxiety, stress, relief, and hope.
Stress and Anxiety Post-Surgery
It’s normal for patients to feel stressed and anxious after colon surgery. They worry about their recovery and possible complications. They also notice changes in their body. Seeing these feelings as part of recovery helps them cope better.
Managing stress and anxiety is key for a smooth recovery. Deep breathing, meditation, and gentle exercise can help. Also, having a strong support system is very important for emotional well-being.
Coping Strategies for Recovery
Using effective coping strategies is vital for emotional and psychological challenges in recovery. Keeping a positive outlook, setting realistic goals, and doing things that bring joy are helpful. Staying connected with family, friends, and healthcare providers also provides emotional support.
- Practice relaxation techniques, such as deep breathing or progressive muscle relaxation.
- Stay engaged with loved ones through regular communication.
- Participate in activities that promote mental well-being, such as reading or listening to music.
Importance of Support Systems
A strong support system is key for patients recovering from colon surgery. Family, friends, and support groups offer emotional support and practical help. Having a support system makes patients feel more secure and less alone.
We encourage patients to ask for help from loved ones and healthcare providers. This way, they can build a network of care that meets their emotional and psychological needs during recovery.
Role of Healthcare Professionals
Healthcare professionals play a big role in helping patients recover after colon surgery. They offer the support needed to make the recovery smoother. With their help, patients can get through this tough time more easily.
Surgeon’s Protocols for Postoperative Care
Surgeons create care plans for each patient. These plans are made just for them, based on their surgery and health.
We follow strict protocols. This includes:
- Watching for any complications
- Helping manage pain
- Guiding on diet changes
By sticking to these protocols, we lower the chance of problems after surgery. This helps patients recover faster and better.
Importance of Nursing Support
Nurses are key in postoperative care. They are always there, giving emotional support, managing meds, and watching for any issues.
A study in the Journal of Clinical Nursing highlights their role. It says nurses are vital in the team, giving constant care and support to patients.
“Nurses are often the first point of contact for patients. They offer emotional support and answer questions quickly.”
– Journal of Clinical Nursing
Patient Education and Resources
Teaching patients about their care is key for a good recovery. We give them info on managing symptoms, diet, and follow-up care.
Resource | Description |
Postoperative Guidelines | Detailed instructions on postoperative care |
Nutritional Counseling | Advice on dietary changes post-surgery |
Follow-Up Appointments | Scheduling and reminders for postoperative check-ups |
By giving patients the knowledge and support they need, we improve their recovery. This makes their experience better and the outcomes better too.
Conclusion: Navigating Recovery After Colon Surgery
We are here to help guide you through your postoperative symptoms.
Key Considerations
It’s important for patients to keep talking to their provider about any worries. This includes talking about food, managing nausea, and watching for signs of trouble like infection or blockages.
Long-Term Outcomes
Putting a focus on long-term health and sticking to follow-up care plans is key. This helps patients avoid problems and get back to full health.
By being informed and active, Stem Cell patients can smoothly navigate their recovery. We stress the need for teamwork between patients and their healthcare team for the best outcomes.
FAQ
What is considered a normal duration for nausea and vomiting after colon surgery?
Nausea and vomiting usually last a few days after colon surgery. But, it can vary based on the surgery type, anesthesia, and health. If symptoms last more than a week, see your doctor.
How can I manage vomiting after colon surgery?
To manage vomiting, start with a clear liquid diet. Then, add bland foods slowly. Drink lots of fluids to stay hydrated. Your doctor might also give you anti-nausea meds.
What are the signs of complications related to vomiting after colon surgery?
Look out for signs of infection like fever or more pain. Also, watch for bowel obstruction signs like severe pain or constipation. Dehydration signs include too much thirst or dark urine. If you see these, call your doctor right away.
When should I contact my healthcare provider regarding vomiting after colon surgery?
Call your doctor if vomiting is bad or lasts a long time. Also, if you have dehydration signs, more pain, fever, or can’t keep fluids down. Keeping a symptom diary helps track your recovery.
How can I cope with stress and anxiety after colon surgery?
Try relaxation techniques like deep breathing or meditation. Stay in touch with loved ones and get support from healthcare teams. Emotional support is key for a smooth recovery.
What role do healthcare professionals play in postoperative care?
Healthcare teams, including surgeons and nurses, are vital in post-op care. They guide symptom management, watch for complications, and offer emotional support. They teach self-care and follow-up to help you recover well.
Why is it important to stay hydrated after colon surgery?
Staying hydrated prevents dehydration and its risks like electrolyte imbalances or low blood pressure. Drinking small amounts of fluids helps your recovery.
What dietary adjustments should I make after colon surgery?
Start with a clear liquid diet, then bland foods like crackers or toast. As you get better, you can eat more solid foods. Listen to your body and avoid foods that upset you.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11849839/