Last Updated on December 2, 2025 by Bilal Hasdemir
A lot of people worldwide struggle with obesity. Some weigh over 160kgs (25 stone). This greatly affects their health and social care. Clarifying the typical Weight of Bariatric Patients and the BMI criteria for surgery eligibility.
The term “bariatric” is about the medicine for obesity. Knowing what definition of bariatric means is key to helping these people.
Bariatric patients have big challenges. They might have trouble moving, face health issues, and find it hard to get medical help because of their size.
Key Takeaways
- The term “bariatric” relates to the medical field focusing on obesity.
- Bariatric patients often weigh over 160kgs and face significant health challenges.
- Understanding bariatric care is essential for providing appropriate healthcare.
- Obesity categories are important in figuring out the care needed.
- Bariatric patients need special care because of their unique needs.
Understanding the Term “Bariatric”
It’s important to know what “bariatric” means when talking about obesity treatment. The term “bariatric” refers to the study and treatment of obesity. It includes finding causes, preventing, treating, and managing obesity.
Medical Definition of Bariatric
The word “bariatric” comes from Greek words. “Baros” means weight, and “iatros” means doctor or healer. In medicine, bariatric care helps people with obesity. It includes surgical interventions and non-surgical management strategies.
Origin and Usage in Healthcare
The term “bariatric” started in the early 20th century. But it became more common in the late 20th century as obesity rates increased. Doctors use it to talk about patients, procedures, and equipment for those with obesity.
Distinction Between Bariatric Patients and Procedures
Bariatric patients need special care because of their weight and health issues. Bariatric procedures, like gastric bypass and gastric sleeve, help with weight loss.
It’s key to know the difference between bariatric patients and procedures. This helps doctors give better care and support. They can address the health risks associated with obesity and help patients get better.
Obesity Classifications and BMI Ranges
It’s important to know about obesity classifications to find the right treatment. Obesity is a complex issue. It’s measured by the Body Mass Index (BMI), a key tool for checking body fat.
Body Mass Index (BMI) Explained
BMI is found by dividing your weight in kilograms by your height in meters squared. This simple method shows if your weight is healthy for your height.
BMI Calculation: BMI = weight (kg) / height (m)
WHO and CDC Weight Classifications
The World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) have set BMI categories:
- Underweight: BMI
- Normal weight: BMI = 18.5-24.9
- Overweight: BMI = 25-29.9
- Obese: BMI ≥ 30
The obese category breaks down into three classes:
- Class I obesity: BMI = 30-34.9
- Class II obesity: BMI = 35-39.9
- Class III obesity: BMI ≥ 40
Limitations of BMI as a Measure
BMI is useful but has its downsides. It doesn’t measure body fat directly or tell the difference between fat and muscle. So, athletes or those with a lot of muscle might have a high BMI without being obese.
Even with its flaws, BMI is a key tool for spotting health risks linked to weight. Knowing about BMI categories and their meanings is vital for healthcare professionals and those trying to manage their weight.
The Weight of Bariatric Patients: Average Ranges
It’s key for doctors to know the average weight of bariatric patients. This helps them give the right care and treatment. Bariatric patients usually have a BMI of 40 or more. Or, they have a BMI of 35-39.9 with health problems.
Statistical Data on Bariatric Patient Weights
Research shows that bariatric patients’ weights vary a lot. Studies say these patients are often much heavier than most people.
Average weights for bariatric patients range from 250 to over 400 pounds. This depends on the study group.
Variations by Demographics and Region
The weight of bariatric patients changes based on who they are and where they live. Some groups might be heavier due to genes, environment, or money issues.
According to
“Bariatric Surgery: A Guide for Patients,”
how much weight patients lose after surgery varies. This depends on the surgery type and who the patient is.
Weight Distribution Patterns in the United States
In the U.S., the weight of bariatric patients mirrors the country’s obesity trends. Places with more obesity tend to have more bariatric patients.
The CDC’s data shows obesity rates change across states and groups. This affects the average weight of bariatric patients.
Obesity Classes and Their Clinical Significance
Understanding obesity classes is key to managing this condition. Obesity is divided into classes based on Body Mass Index (BMI). BMI is a common way to measure weight status.
Healthcare providers use these categories to see how severe obesity is. The World Health Organization (WHO) has outlined three main obesity classes: Class I, II, and III.
Class I Obesity (BMI 30-34.9)
Class I obesity is the least severe. People in this range are at higher risk for diabetes and cardiovascular diseases.
Class II Obesity (BMI 35-39.9)
Class II obesity is more serious. It comes with a higher risk of health problems. Patients here need stronger weight management plans.
Class III Obesity (BMI 40+)
Class III obesity is the most severe. It’s divided further, with super obesity being a notable subcategory.
Super Obesity (BMI 50+)
Super obesity, with a BMI of 50 or more, is extremely severe. People with super obesity face big challenges in losing weight. They are at high risk for serious health issues.
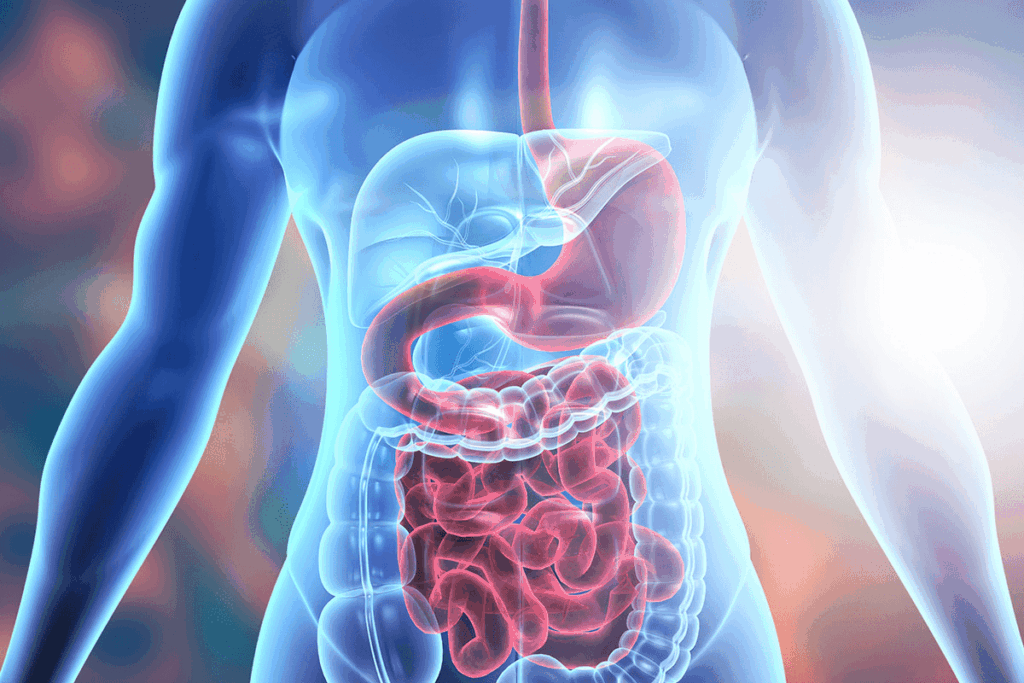
Health Risks Associated with Severe Obesity
Severe obesity poses many health risks, affecting different parts of the body and overall health. It’s a complex issue that raises the risk of many health problems. These problems can affect how long someone lives and their quality of life.
Cardiovascular Complications
One major risk of severe obesity is heart disease. This includes high blood pressure, heart failure, and blocked arteries. The extra weight strains the heart, leading to serious complications.
Metabolic Disorders
Severe obesity is also linked to metabolic disorders like type 2 diabetes. Obesity often leads to insulin resistance, which can cause diabetes. This makes health problems even worse.
Musculoskeletal Issues
Obesity can cause musculoskeletal problems, like osteoarthritis. The extra weight strains joints, mainly in the hips, knees, and lower back. This can lead to chronic pain and trouble moving.
Respiratory Problems
People with severe obesity often face respiratory issues. These include sleep apnea and obesity hypoventilation syndrome. These conditions can greatly affect daily life and need careful management.
Impact on Longevity and Quality of Life
The health risks of severe obesity can shorten life expectancy and lower quality of life. It’s important to manage obesity through medical care and lifestyle changes. This can help reduce these risks.
Bariatric Surgery Eligibility Criteria
To be eligible for bariatric surgery, several factors are considered. These include weight and health conditions. Patients must meet specific criteria to see if they’re a good fit for the surgery.
Weight Requirements for Surgery
Weight is a key factor in deciding if someone can have bariatric surgery. A Body Mass Index (BMI) of 40 or higher usually means you qualify. If your BMI is between 35-39.9, you need to have obesity-related health issues too.
Comorbidity Considerations
Health problems like type 2 diabetes and sleep apnea are important when deciding if you can have surgery. These issues can make life harder and raise surgery risks. But, they also show you really need help to lose weight.
Insurance Coverage Requirements in the US
In the US, insurance for bariatric surgery varies. Most plans cover it for those who meet certain criteria. This includes trying to lose weight and getting a full medical check-up. The rules for insurance often match the medical guidelines for surgery.
Changes in Eligibility Guidelines Over Time
Eligibility rules for bariatric surgery have changed over time. At first, only those with very high BMIs were considered. Now, more people can get surgery thanks to better understanding of obesity and better surgery and care after it.
Patient Selection Process for Bariatric Procedures
The process to choose patients for bariatric surgery is detailed. It checks if a patient is right for surgery. This careful check helps patients get the best results.
Medical Evaluation Components
A detailed medical check is key to see if someone can have bariatric surgery. It looks at the patient’s health, their medical history, and any health risks.
A study in a Journal showed a risk. Patients with heart disease face more problems during surgery.
“A thorough medical check is vital to spot high surgical risks.”
Psychological Assessment
Checking a patient’s mental health is also important. It finds any mental issues that might affect following surgery advice.
- Checking mental health
- Looking at how they cope
- Finding mental risks
Nutritional Evaluation
Looking at a patient’s diet and nutrition is also needed. It finds diet areas to improve and prepares for post-surgery eating changes.
Nutritional Component | Pre-Surgery Requirements | Post-Surgery Recommendations |
Protein Intake | 60-80 grams/day | 80-100 grams/day |
Fluid Intake | At least 8 cups/day | At least 8 cups/day |
Team Approach to Patient Selection
A team decides if someone is right for bariatric surgery. This team has a surgeon, psychologist, dietitian, and more.
This team works together. They check the patient’s health and well-being. This ensures the patient gets full care during surgery.
Pre-Surgery Weight Management Protocols
Patients getting ready for bariatric surgery need to follow a detailed weight management plan. This step is key to getting them healthy and ready for surgery.
Required Weight Loss Before Surgery
One important part is losing a certain amount of weight. The exact amount varies but aims to shrink the liver and body fat. This makes surgery easier and safer.
Dietary Preparation
Getting your diet right is also critical. Patients are often told to eat a specific way. This might include:
- Low-calorie intake: To lose weight and shrink the liver.
- Nutritional balance: Make sure to get enough protein, vitamins, and minerals.
- Hydration: Drink lots of water to stay hydrated.
Medical Weight Management Options
Some might also get medical help to lose weight before surgery. This could include:
- Very Low-Calorie Diets (VLCD): These diets, watched by doctors, help lose a lot of weight.
- Prescription weight loss medications: Certain drugs can help with weight loss, but only with a doctor’s guidance.
Benefits of Pre-Surgical Weight Loss
There are many good reasons to lose weight before surgery. These include:
- Less time and risk during surgery
- Quicker and easier recovery after surgery
- Better health and feeling overall
Impact of Weight on Surgical Outcomes
The weight of a patient greatly affects the success of bariatric surgery. A patient’s weight can change how complex and risky the surgery is. It also impacts how well they recover and how long-term the results are.
Operative Risks Related to Weight
Patients who are heavier often face more operative risks. These risks include more complications during surgery. They can have less lung space, lose more blood, and need longer surgeries.
Recovery Time Correlations
The recovery time for bariatric surgery patients can vary a lot. Patients with a higher BMI usually need longer hospital stays. They also face a tougher recovery because of health issues.
Long-term Success Predictors
Long-term success after bariatric surgery depends on several things. These include the patient’s starting weight, following diet plans after surgery, and any health problems they have. Patients with a lower initial BMI usually see better long-term weight loss.
Surgical Technique Modifications for Higher-Weight Patients
For patients who are much heavier, surgeons might change their surgical techniques. They do this to fit the patient’s body and lower risks. These changes can include different surgical methods, tools, and care plans after surgery.
Post-Surgical Weight Loss Expectations
It’s important to know what to expect after bariatric surgery. Patients usually lose a lot of weight, but how much and how fast can vary.
Typical Weight Loss Trajectories
In the first year, most patients lose a lot of weight. The biggest weight loss happens in the first 6-12 months. Then, the weight loss slows down.
- Rapid Weight Loss Phase: The first 3-6 months see the most dramatic weight loss.
- Steady Weight Loss Phase: Between 6-12 months, the weight loss continues but at a slower pace.
- Weight Loss Plateau: After 12-18 months, many patients reach a plateau where weight loss slows down significantly or stops.
Factors Affecting Weight Loss Success
Many things can affect how well you lose weight after surgery. These include:
- Dietary Adherence: Sticking to the recommended dietary guidelines is key.
- Physical Activity: Regular exercise helps with weight loss and health.
- Behavioral Modifications: Changing eating habits and lifestyle is important for lasting success.
Managing Weight Loss Plateaus
Plateaus are common, but there are ways to deal with them:
- Adjusting dietary habits to avoid nutritional deficiencies.
- Increasing physical activity levels.
- Seeking support from healthcare professionals or support groups.
Realistic Goal Setting
Setting realistic weight loss goals is key for success. Patients should work with their healthcare providers to set goals that fit their situation.
Lifestyle Changes for Long-term Weight Management
Long-term success in weight management is closely tied to adopting and maintaining healthy lifestyle habits. After bariatric surgery, patients must make significant changes to their daily routines. This ensures sustained weight loss and overall health improvement.
Physical Activity Recommendations
Regular physical activity is key for keeping weight off and improving health. The American Heart Association suggests at least 150 minutes of moderate-intensity aerobic activity weekly. Or, 75 minutes of vigorous-intensity aerobic activity, or a mix of both.
Strength training exercises at least twice a week also help. They build muscle and boost metabolism.
- Aim for 30 minutes of moderate-intensity exercise per day, five days a week.
- Incorporate high-intensity interval training (HIIT) for enhanced calorie burn.
- Include strength training to build muscle and improve body composition.
Sustainable Dietary Habits
Adopting sustainable dietary habits is essential for long-term weight management. Focus on nutrient-dense foods, control portion sizes, and avoid high-calorie, high-fat, and high-sugar foods.
Food Group | Recommended Foods | Foods to Avoid |
Proteins | Lean meats, fish, eggs, tofu | Processed meats, high-fat meats |
Fruits and Vegetables | Variety of colorful fruits and vegetables | Fried or high-calorie versions |
Grains | Whole grains, brown rice, quinoa | Refined grains, sugary cereals |
Behavioral Modifications
Behavioral changes are critical for maintaining weight loss. This includes developing healthy eating habits, managing stress, and staying hydrated.
Building Healthy Routines
Establishing a routine is key for long-term weight management. Set realistic goals, track progress, and seek support when needed.
- Set specific, achievable goals for physical activity and dietary changes.
- Keep a food and exercise diary to track progress.
- Seek support from healthcare professionals, support groups, or family and friends.
By incorporating these lifestyle changes, bariatric patients can achieve and maintain significant weight loss. This improves their overall health and quality of life.
Psychological Aspects of Bariatric Weight Management
Psychological factors are key to success in bariatric weight management. The journey to losing weight involves physical and mental changes.
Body Image Concerns
People getting bariatric surgery often worry about their body image. This worry can come from losing weight fast, which might leave loose skin. Or it can be from getting used to a new body.
Body image issues can really affect someone’s mental health and happiness. It’s important to get support from doctors, family, and friends to deal with these worries.
Emotional Relationship with Food
How we feel about food is also very important. Many people who get bariatric surgery use food to handle stress.
“Understanding and changing one’s emotional relationship with food is key to successful weight management.”
Support Systems and Their Importance
Having a strong support system is vital for bariatric patients. This includes family, friends, and support groups.
Having a good support system can really help with bariatric weight management.
Addressing Weight Stigma and Discrimination
Weight stigma and discrimination are big problems for bariatric patients. It’s important to tackle these issues for their mental health.
Impact | Consequences | Support Measures |
Emotional Distress | Low Self-Esteem, Anxiety | Counseling, Support Groups |
Social Isolation | Depression, Loneliness | Family Support, Social Integration |
Nutritional Support for Bariatric Patients
Nutritional support is key for bariatric patients. It includes dietary guidelines, supplements, and ongoing monitoring. Bariatric patients need special nutrition because of their obesity and surgery.
Dietary Guidelines Before and After Surgery
Bariatric patients must follow certain diets before and after surgery. Before surgery, they eat very few calories to shrink their liver. After surgery, they start with liquids, then move to soft foods, focusing on protein and vitamins.
Nutritional Deficiencies and Supplementation
Bariatric surgery can cause nutrient deficiencies because the body absorbs less. Common issues include vitamin B12, iron, calcium, and vitamin D. Taking supplements is vital to avoid these problems, and patients often need them for life.
Nutritional Deficiency | Common Supplements |
Vitamin B12 | Oral or injectable Vitamin B12 |
Iron | Iron tablets or intravenous iron |
Calcium and Vitamin D | Calcium and Vitamin D supplements |
Long-term Nutritional Monitoring
Monitoring nutrition long-term is vital for bariatric patients. It helps ensure they get the nutrients they need and fixes any issues quickly. Regular check-ups with healthcare teams, including dietitians, are essential.
Working with Registered Dietitians
Registered dietitians are critical for bariatric patients. They offer tailored dietary advice, check nutritional levels, and manage nutrition-related problems. Working closely with dietitians greatly improves patient results.
“The role of the registered dietitian is key in the team caring for bariatric surgery patients. They offer nutrition expertise and help improve patient outcomes.”
Conclusion: Comprehensive Care for Bariatric Patients
Getting the right care is key for bariatric patients to manage their weight and improve health. This care comes from a team of doctors, nutritionists, and psychologists. Each patient needs a plan that fits their unique needs, helping them reach their weight loss goals.
Support groups, nutrition advice, and exercise programs are big helps for bariatric patients. They make the journey easier. Also, how insurance covers weight-related treatments is very important. It affects what treatments and procedures patients can get.
Teaching bariatric candidates about their care is also vital. It gives them the knowledge to make smart choices. Knowing the risks and benefits of surgery helps them make the best decisions for long-term success.
FAQ
What is the definition of bariatric?
“Bariatric” is about treating obesity and related health issues. It’s for people with a Body Mass Index (BMI) of 40 or higher. Or those with a BMI of 35 or higher and health problems linked to obesity.
What are the eligibility criteria for bariatric surgery?
To get bariatric surgery, you need a BMI of 40 or higher. Or a BMI of 35 or higher with health issues. Insurance rules vary, but most want you to try other weight loss methods first.
What is the average weight of bariatric patients?
Bariatric patients’ weights vary. But, they usually weigh between 300-400 pounds. Some can weigh over 500 pounds.
What are the health risks associated with severe obesity?
Severe obesity brings serious health risks. These include heart problems, metabolic disorders, and breathing issues. These can greatly affect your life and how long you live.
What is the patient selection process for bariatric procedures?
Choosing patients for bariatric surgery is a detailed process. It includes medical, psychological, and nutritional checks. This team approach ensures patients are ready for surgery and have support for success.
What are the pre-surgery weight management protocols?
Before surgery, patients follow weight management plans. This includes diet, weight loss, and medical help. These steps help patients reach a healthier weight and reduce surgery risks.
How does weight impact surgical outcomes?
Weight affects surgery outcomes a lot. It influences risks, recovery time, and success chances. Heavier patients might need special surgery techniques to reduce risks and improve results.
What are the post-surgical weight loss expectations?
Weight loss after surgery varies by person and surgery type. But, most lose a lot of weight in the first year. They can lose 50-80% of excess body weight.
What lifestyle changes are necessary for long-term weight management?
Keeping weight off long-term needs lifestyle changes. This includes exercise, healthy eating, and behavior changes. Patients also need ongoing support and monitoring to keep their weight loss and health.
What nutritional support is required for bariatric patients?
Bariatric patients need nutritional help before and after surgery. This includes diet advice, supplements, and ongoing nutrition checks. Working with a dietitian helps ensure good nutrition and lowers complication risks.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30535365/