Traumatic brain injury, or TBI, is a condition that affects millions worldwide. It happens when a bump, blow, or jolt to the head disrupts normal brain function.
Recent global data from 2021 shows about 20.84 million incident cases of TBI worldwide. This number includes 37.93 million prevalent cases affecting people in all regions.
At Liv Hospital, we are dedicated to top-notch medical care for TBI patients. We have a team of specialists ready to offer complete care and support. They help those affected by this serious health issue.
Key Takeaways
- Traumatic brain injury (TBI) is a major global health concern.
- TBI affects millions of people worldwide, across all age groups.
- Falls and motor vehicle accidents are among the leading causes of TBI.
- Liv Hospital provides complete care and support for TBI patients.
- Understanding the causes and effects of TBI is key for effective treatment.
The Fundamentals of Traumatic Brain Injury (TBI)

It’s important to know about Traumatic Brain Injury (TBI) for everyone. TBI means brain injury from a force, like a bump or jolt. It can be mild or severe and affects brain function.
Definition and Basic Mechanisms
TBI is when the brain changes because of an outside force. This force can be a direct hit to the head or a jolt, like in a car crash. The injury starts with the initial hit and then leads to more damage.
Primary brain injury happens right at the moment of impact. It can cause fractures, hemorrhages, and other damage to the brain.
Primary vs. Secondary Brain Injury
It’s key to know the difference between primary and secondary brain injury. Primary injury happens right away from the trauma. Secondary injury is the damage that comes after, from things like low blood pressure or high pressure in the skull.
|
Characteristics |
Primary Brain Injury |
Secondary Brain Injury |
|---|---|---|
|
Timing |
Occurs at the moment of impact |
Occurs after the initial injury |
|
Causes |
Mechanical forces (e.g., direct blow, acceleration/deceleration) |
Complications (e.g., hypotension, hypoxia, raised ICP) |
|
Examples |
Fractures, hemorrhages, axonal injuries |
Edema, infection, further neuronal damage |
Pathophysiology of TBI: How Brain Damage Occurs
It’s key to understand how TBI causes brain damage to find better treatments. Traumatic Brain Injury sets off a chain of changes in brain cells and molecules. These changes can greatly affect how the brain works.
Cellular and Molecular Changes
After a TBI, the brain goes through many changes. These include disruption of the blood-brain barrier, inflammation, and neuronal death. The first injury can harm brain cells and tissues right away.
This harm can start a series of secondary injuries. These injuries make the damage worse.
The damage from TBI can be bleeding, swelling, and tearing of nerve fibers. These injuries can cause both focal and diffuse brain damage. This depends on the trauma’s nature and severity.
Normal Brain vs. TBI Brain Function
Normal brains and TBI brains work differently. In a normal brain, neurons talk well, and brain areas work together. This helps control our body and mind.
In a TBI brain, neurons don’t communicate well. This leads to many symptoms like cognitive, emotional, and physical problems.
The main reason for these differences is the changes in cells and molecules after a TBI. Knowing these changes helps us find better treatments for TBI patients.
The Global Impact of TBI: Statistics and Prevalence
It’s important to know how Traumatic Brain Injury (TBI) affects the world. TBI is a big health problem that hurts people and society too.
Worldwide Incidence and Prevalence
In 2021, about 20.84 million people got TBI worldwide. This shows how big of a problem TBI is. It costs a lot in terms of money, health, and society.
How common TBI is changes from place to place. Things like road safety, violence, and healthcare access play a role. Knowing these differences helps us tackle TBI better.
TBI in the United States: A Growing Public Health Concern
In the U.S., over 69,000 people died from TBI in 2021. That’s about 190 deaths every day. This shows how serious TBI is in the U.S.
The numbers for TBI in the U.S. are scary. They show a big challenge for healthcare, emergency services, and prevention. Here are some important stats:
|
Category |
Number |
Rate per 100,000 |
|---|---|---|
|
TBI-related Emergency Department Visits |
223,135 |
68.6 |
|
TBI-related Hospitalizations |
27,604 |
8.4 |
|
TBI-related Deaths |
69,473 |
21.1 |
The table shows the huge problem TBI is in the U.S. It shows a lot of visits to emergency rooms, hospital stays, and deaths. These numbers highlight the need for more work in prevention, treatment, and recovery.
By understanding TBI’s global and U.S. impacts, we can try to make it less common. We can also help those who have it get better.
What Causes Brain Injury: Common Mechanisms and Risk Factors
It’s important to know what causes brain injuries to prevent them. Brain injuries happen when the brain gets hurt from outside forces. This can lead to physical, mental, and emotional problems.
Falls: The Leading Cause Across Age Groups
Falls are the top reason for brain injuries in all ages. The elderly and young kids are more at risk because of their age. This is due to things like weak bones or being in a growing stage.
- Slippery or uneven surfaces contribute significantly to fall-related injuries.
- Lack of safety measures, such as handrails or non-slip mats, increases the risk.
- Age-related factors, including decreased mobility and balance issues, play a critical role.
Motor Vehicle Accidents and Traffic-Related Trauma
Car crashes are a big cause of brain injuries, mainly in kids and young adults. The crash can cause serious head injuries. This can change someone’s life forever.
Key factors contributing to motor vehicle accident-related TBI include:
- High-speed collisions that increase the severity of impact.
- Failure to use safety restraints, such as seatbelts or helmets.
- Distracted driving, which reduces reaction time and increases the risk of accidents.
Violence, Assaults, and Blunt Trauma to the Head
Violence and assaults also lead to brain injuries. These incidents can cause serious and lasting health problems for survivors.
We need to work on preventing these causes of brain injury. By understanding how and why brain injuries happen, we can find ways to stop them. This will help people affected by brain injuries get better care and outcomes.
Sports-Related TBI and Concussions
Sports-related traumatic brain injuries (TBI) and concussions are big worries in contact sports. They affect athletes at all levels. We look at the dangers in different sports, the range from concussion to TBI, and the harm from repeated head hits.
High-Risk Sports and Activities
Some sports carry a higher risk of head injuries because they involve contact. Football, hockey, and rugby are examples where head collisions are common. Knowing these risks helps us take steps to keep athletes safe.
From Concussion to TBI: Understanding the Spectrum
A concussion is a mild form of TBI, but it’s serious. Its effects can last from minutes to months, depending on the injury and how the person reacts. It’s important to grasp this range to help manage and recover from these injuries.
Repetitive Head Trauma and Cumulative Effects
Repetitive head trauma, seen in athletes with many concussions or subconcussive hits, can cause lasting harm. This includes changes in thinking, feeling, and behavior. We explore the long-term effects and ways to reduce them.
By knowing the risks and impacts of sports-related TBI and concussions, we can protect athletes better. This helps improve their outcomes and well-being.
Military and Combat-Related Brain Injuries
Modern warfare has led to more brain injuries in the military. These injuries often come from blasts and are a big worry for healthcare. They affect both the military and veterans’ health.
Blast Injuries and Their Unique Mechanisms
Blast injuries from roadside bombs are common in military conflicts. Most of these are mild head injuries but can have lasting effects. Blast injuries can damage through shockwaves, then from fragments and being thrown.
Post-TBI Syndrome in Veterans
Veterans with TBI often face ongoing symptoms, known as post-TBI syndrome. Symptoms include headaches, dizziness, memory issues, mood swings, and depression. It’s key to understand and treat these symptoms well.
Dealing with military TBI is complex. We need a mix of medical care and support. This helps our veterans and military personnel with brain injuries.
Types and Classification of TBI
Traumatic Brain Injury (TBI) is complex and needs a detailed understanding of its types. It’s classified based on severity, how it happened, and how it affects the brain. This helps doctors create the best treatment plans for each patient.
Severity-Based Classification: Mild, Moderate, and Severe TBI
The severity of TBI is key in deciding treatment and predicting outcomes. The Glasgow Coma Scale (GCS) helps doctors classify TBI into mild, moderate, or severe levels.
- Mild TBI: Has a GCS score of 14-15. It might cause brief loss of consciousness and symptoms like headaches and dizziness.
- Moderate TBI: Scores 9-13 on the GCS. This shows a more serious brain injury, leading to long-term cognitive and physical issues.
- Severe TBI: Scores 8 or less. This indicates severe brain damage, often with lasting effects.
|
TBI Severity |
GCS Score |
Common Symptoms |
|---|---|---|
|
Mild |
14-15 |
Headache, dizziness, confusion |
|
Moderate |
9-13 |
Cognitive impairments, physical disabilities |
|
Severe |
8 or less |
Significant cognitive and physical impairments, possible coma |
Open vs. Closed Craniocerebral Trauma
TBI can also be classified as open or closed craniocerebral trauma. Open TBI means the skull is penetrated, which can lead to infections. Closed TBI happens without skull penetration, like from falls or car accidents.
Focal and Diffuse Brain Damage
TBI can also be categorized by the extent and location of brain damage. Focal brain damage is in one area, often from penetrating trauma. Diffuse brain damage affects more areas, usually from forces that cause damage throughout the brain.
Knowing these TBI classifications is vital for effective treatment. It helps doctors tailor treatments to each patient’s needs, improving outcomes.
Recognizing TBI Symptoms Across the Severity Spectrum
It’s important to know the symptoms of Traumatic Brain Injury (TBI) to get the right treatment. TBI can show up in different ways, based on how severe it is. We’ll look at the symptoms of TBI, from mild to severe.
Physical and Neurological Manifestations
Physical signs of TBI include headaches, dizziness, nausea, and feeling very tired. In serious cases, people might have seizures, blurry vision, or lose consciousness. Neurological signs can be anything from feeling things differently to trouble moving.
- Headaches and dizziness are common first signs.
- Nausea and vomiting can happen, mostly in serious cases.
- Feeling very tired is a common symptom that lasts.
Neurological symptoms can vary a lot, including:
- Sensory issues like hearing ringing or being too sensitive to light.
- Motor problems, like being weak or paralyzed.
Cognitive and Behavioral Changes
TBI can cause big changes in how you think and act. These changes can include feeling confused, disoriented, and having trouble focusing or remembering things. Behavioral changes can range from being easily upset or having mood swings to more serious mental health issues.
Cognitive symptoms can make everyday tasks hard:
- Having trouble concentrating or making choices.
- Memory problems, like forgetting things right away.
Behavioral changes can be tough for the person and their family. These can include:
“Changes in personality, such as increased irritability or mood swings, are not uncommon following a TBI.”
Emergency Signs Requiring Immediate Medical Attention
Some symptoms need immediate medical help. These include:
- Repeated vomiting or nausea.
- Convulsions or seizures.
- Loss of consciousness, even briefly.
If you or someone else is showing these symptoms, get medical help right away.
Special Populations and TBI Risk
Understanding TBI is key to knowing its impact on different groups. This includes children, the elderly, and athletes. Each group faces unique challenges and risks. They need special prevention and treatment plans.
Children and Developmental Considerations
Children are very vulnerable to TBI because their brains and bodies are growing. Head injuries in kids can affect their thinking, feelings, and physical health for a long time. Their skulls are thinner and more flexible, making them more likely to get hurt. Also, their brains are developing, which can change how they recover from TBI.
It’s hard to diagnose TBI in kids because they can’t explain their symptoms well. Doctors have to watch for signs and listen to parents to figure out how bad the injury is. Parents and caregivers should watch for changes in behavior, appetite, or sleep. If they think a kid has a head injury, they should get medical help right away.
Elderly and Age-Related Vulnerabilities
The elderly are also at high risk for TBI, mainly because of falls. As people get older, their bones get weaker and they have trouble balancing, making falls more likely. Older adults might also have health problems that make TBI harder to treat.
Older adults are more likely to have serious problems from TBI, like bleeding in the brain. It’s very important to get medical help quickly if an older person has a head injury. This can really help their recovery.
Athletes and Occupational Hazards
Athletes, like those in football, hockey, and soccer, are at high risk for TBI. Getting hit in the head many times can cause a brain disease called CTE, leading to memory loss, depression, and dementia. Sports are making rules and safety plans to lower the risk of head injuries.
Jobs in construction, manufacturing, and the military also increase TBI risk. Workers in these fields often get hurt from falls, being hit by objects, or other head injuries. Employers can help by following safety rules, giving out protective gear, and teaching workers how to avoid hazards.
Diagnosing and Assessing TBI
Diagnosing TBI is complex. It requires a detailed clinical evaluation, advanced neuroimaging, and cognitive and functional tests. Getting it right is key for the right treatment.
Clinical Evaluation in Neurology
Clinical evaluation is the first step in diagnosing TBI. Neurologists check symptoms, medical history, and brain function. They look at consciousness, thinking, and physical skills.
Key components of clinical evaluation include:
- Patient history and symptom assessment
- Neurological examination
- Assessment of cognitive and behavioral changes
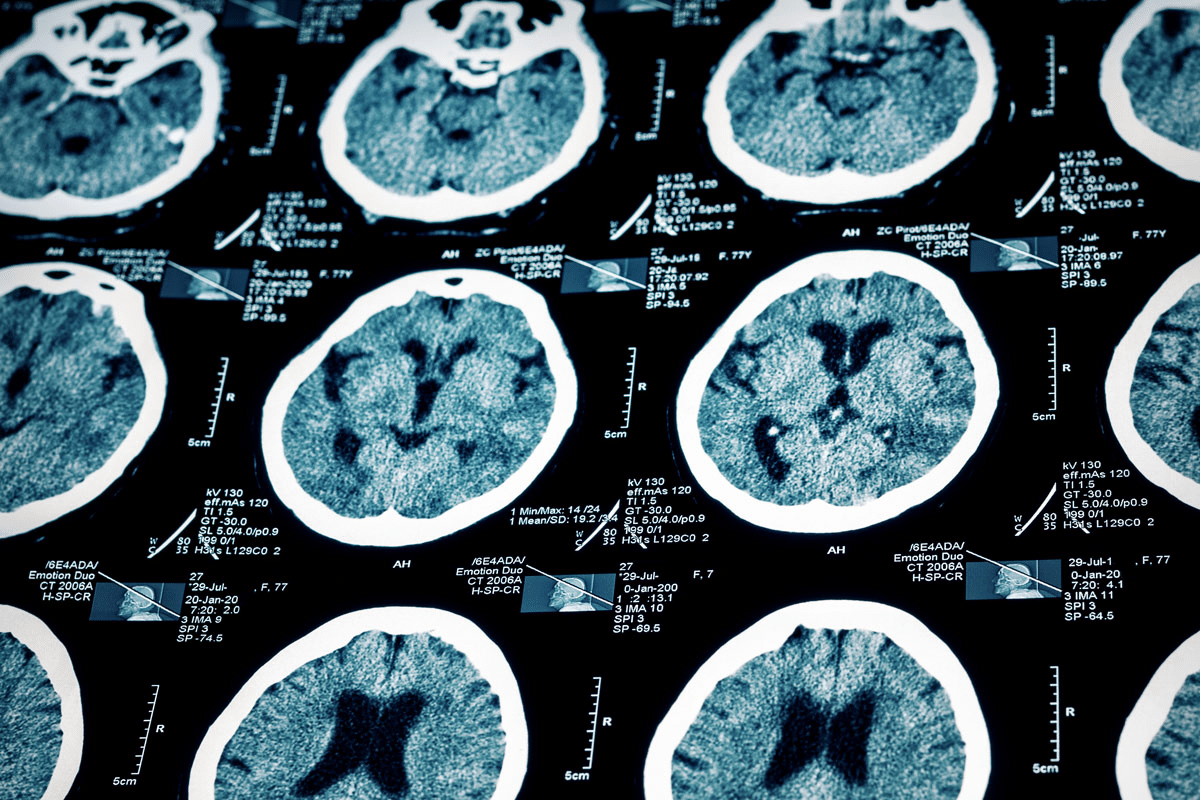
Advanced Neuroimaging Techniques
Advanced neuroimaging is vital for TBI diagnosis. CT scans and MRI show brain structure and injuries. CT scans spot bleeding and fractures quickly. MRI shows soft tissue damage.
Neuroimaging techniques help understand brain damage. They guide treatment choices.
Cognitive and Functional Testing
Cognitive and functional tests check TBI’s effects on thinking, feelings, and behavior. They find where skills are lacking. This helps plan rehabilitation.
Examples of cognitive and functional tests include:
- Neuropsychological assessments
- Cognitive function tests
- Behavioral and emotional assessments
Together, clinical evaluation, neuroimaging, and testing help doctors accurately diagnose TBI. They can then create effective treatment plans.
Treatment Approaches and Rehabilitation Strategies
Effective treatment for TBI needs a mix of acute care, rehab, and long-term support. This mix is key to meeting the complex needs of TBI patients.
Acute Medical Management
The first step in TBI treatment is to keep the patient stable and prevent more brain damage. Acute medical management includes emergency surgery, meds to control pressure, and close watch in ICU.
Quick and right care in the early stages can greatly improve TBI patient outcomes. It’s vital for doctors to stick to proven guidelines for the best care.
Comprehensive Rehabilitation Programs
When the patient is stable, comprehensive rehabilitation programs take over. These programs are made for each person’s needs. They might include physical, occupational, speech, and cognitive therapy.
Rehab aims to help patients get back lost functions, adapt to changes, and boost their life quality. A team of experts works together to make a rehab plan just for that person.
Long-term Support and Adaptation
TBI care doesn’t stop after rehab. It needs long-term support and adaptation strategies. This might include ongoing therapy, psychological help, and support to get back into daily life and community activities.
Long-term support is key for TBI patients and their families to deal with recovery and changes. It also means making home and work places accessible and providing resources for learning and adapting.
By taking a long-term and all-inclusive approach to TBI care, we can greatly improve outcomes for those affected by it.
Conclusion: Advancing TBI Prevention and Care
Understanding and managing Traumatic Brain Injury (TBI) is key to better outcomes. We’ve looked at TBI’s causes, symptoms, diagnosis, and treatments in this article.
Preventing TBI is essential. We can do this by using safety gear and improving safety in risky activities. This can greatly lower TBI risks.
We need to keep improving TBI care. This means raising awareness, supporting research, and creating detailed rehab programs. This will help those with TBI and their families.
Working together on TBI prevention, care, and treatment will lead to better lives for patients. It will also improve their quality of life.
FAQ
What is Traumatic Brain Injury (TBI)?
Traumatic Brain Injury (TBI) is a complex injury. It has a wide range of symptoms and disabilities. It happens when a sudden trauma damages the brain, disrupting its normal function.
What are the primary and secondary brain injuries in TBI?
Primary brain injury is the immediate damage from the trauma. Secondary brain injury is the damage that happens later, due to cellular and molecular changes.
What are the common causes of TBI?
TBI can be caused by falls, motor vehicle accidents, violence, and sports injuries. These incidents can lead to different levels of TBI severity.
How does TBI affect the brain?
TBI can damage the brain in various ways. It can cause focal and diffuse damage. This can lead to changes in brain function, affecting thinking, emotions, and behavior.
What are the symptoms of TBI?
Symptoms of TBI vary widely. They can include physical and neurological signs, changes in thinking and behavior. Symptoms can range from mild to severe.
How is TBI diagnosed?
Diagnosing TBI involves a detailed approach. It includes clinical evaluation, advanced neuroimaging, and cognitive and functional testing. These help assess the injury’s extent.
What are the treatment approaches for TBI?
Treatment for TBI includes immediate medical care and rehabilitation programs. It also includes long-term support to help individuals adapt and recover.
Can TBI be prevented?
While not all TBIs can be prevented, some measures can reduce the risk. Wearing protective gear, following safety guidelines, and being aware of hazards are important.
What is the significance of understanding TBI?
Understanding TBI is key for prevention, better diagnosis and treatment, and support for those affected. It helps improve outcomes for individuals with TBI.
What is the global impact of TBI?
TBI is a major public health issue worldwide. It has a significant incidence and prevalence. It affects individuals, families, and communities greatly.
What is post-TBI syndrome?
Post-TBI syndrome is a set of symptoms that can occur after TBI. It includes cognitive, emotional, and behavioral changes. It affects people differently.
How does TBI affect different populations?
TBI affects different groups, like children, the elderly, and athletes, in unique ways. This requires tailored prevention and treatment strategies.
What is the role of rehabilitation in TBI care?
Rehabilitation is vital in TBI care. It helps individuals regain lost functions and adapt to their condition. It aims to maximize recovery and quality of life.
What is the definition of closed craniocerebral trauma?
Closed craniocerebral trauma is a type of TBI. The skull remains intact, but the brain is damaged due to the injury’s force.
What is blunt trauma to the head?
Blunt trauma to the head is a non-penetrating injury. It can cause TBI and occurs in incidents like falls or motor vehicle accidents.
Reference
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from https://www.cdc.gov/traumatic-brain-injury/data-research/facts-stats/index.html






